Abstract
We evaluated the association between radiographically-assessed extension and density of root canal fillings and post-operative apical radiolucencies (AR) using data from 288 participants in the Veterans Affairs Dental Longitudinal Study. Study subjects were not VA patients; all received their medical and dental care in the private sector. Generalized Estimating Equations were used to account for multiple teeth within subjects and to control for covariates of interest. Defective root filling density was associated with increased odds of post-operative AR among teeth with no pre-operative AR (Odds Ratio=3.0, 95%CI=1.3–7.1), though pre-operative AR was the strongest risk factor for post-operative AR (Odds Ratio=29.2, 95%CI=13.6–63.0 among teeth with ideal density). Compared to well-extended root fillings, neither over- nor under-extended root fillings separately were related to post-operative AR, but when those two categories were collapsed into one “poorly-extended” category, poor extension was related to post-operative AR (Odds Ratio=1.8, 95%CI=1.1–3.2).
Keywords: endodontics, epidemiology, longitudinal studies, periapical periodontitis, root canal therapy
INTRODUCTION
With regard to published studies of root canal therapy (RCT) and apical periodontitis (AP), several consistencies have emerged, including: AP and RCT are common (1.4 – 8.5% and 1.5 – 21.5% of teeth, respectively); AP is more prevalent among root canal filled (RCF) teeth than non-RCF teeth (16.7 – 61.0% of RCF teeth versus 0.53 – 4.4% of non-RCF teeth); and overall quality of root fillings generally is poor (inadequate quality in 51 – 86% of RCF teeth) (1–3). Criteria used to assess quality of root fillings often are based on the radiographically-assessed characteristics of density (the extent to which the root filling material uniformly and completely fills the canals) and extension (the distance from the end of the root filling material to the radiographic apex). Root fillings designated as inadequate by these criteria do not necessarily lead to unsatisfactory endodontic results, nor do root fillings designated as adequate by these criteria lead to satisfactory endodontic results. Still, many follow-up clinical studies on RCF teeth suggest that poor root filling density and extension are associated with post-operative AP (4–7).
It is difficult to make direct comparisons between relevant articles because studies differ in many ways. Gaps in the literature include the following:
One gap relates to methodologic flaws. Correlations among teeth within individuals often are ignored (7–9). Analyses that do not account for clustering of observations (i.e., teeth) within individuals ignore the appropriate correlation structure and can lead to incorrect inferences in hypothesis testing (10, 11), while analyses that randomly select one observation per person are inefficient because not all data are used.
Another gap relates to the limited populations studied. Conclusions made from epidemiological studies generally are considered more valid if similar findings are observed among different populations and across different conditions. In one recent review (12), only one U.S. study (13) was included among the 11 identified observational cohort studies. In addition, all previous U.S. studies involved either patients from dental clinics or teaching hospitals (4, 13–16) or enrollees in dental insurance programs (17); none has used a population-based sample, thus endodontic outcomes in the general U.S. population remain unstudied.
The third gap is that few longitudinal data are available. Compared with cariology and periodontology, epidemiological data on endodontology are scarce. Cross-sectional designs or longitudinal designs with only 6–12 months of observation prevail among existing studies. Healing and growth of periapical lesions are dynamic processes that require considerable time; 3–4 years or more may be required to record a stable treatment outcome (18, 19).
To address these gaps we conducted the present study, the aim of which was to investigate the association between radiographically-assessed extension and density of root fillings and the prevalence of apical radiolucencies (AR) three years after RCT, while controlling for the presence of pre-operative AR and other tooth- and person-level covariates.
MATERIAL AND METHODS
Data analyzed in this study were from the Veterans Affairs Dental Longitudinal Study (VADLS), an ongoing, closed-panel longitudinal study of oral health and disease among 1,231 adult males aged 25–85 years at baseline. The cohort was established starting in 1968 through community-based recruitment of adult men from the greater Boston metropolitan area. Subjects were not patients of the VA system; rather, they received dental and medical care through the private sector.
One goal of the VADLS has been to identify determinants of oral health in an aging population. Participants had varying oral conditions at baseline, though all were free of chronic medical conditions. Since baseline, study participants have been seen once every three years for comprehensive dental and medical examinations. Dental examinations include both clinical and radiographic components. The clinical component records DMFS (i.e., decayed, missing or filled coronal tooth surfaces) and periodontal status. The radiographic component includes a full mouth series of intra-oral radiographs (20).
To date, the cohort has been under observation for over 30 years. The average interval between VADLS exams has been approximately 38 months (21). The present study used the existing computerized VADLS database to identify a random sample of 853 dentate participants, each with a complete record for each of the 32 permanent teeth/tooth spaces at each examination cycle. The protocol for this study was reviewed and approved by the Institutional Review Board on Research Involving Human Subjects at the VA Boston Healthcare System.
Our analysis includes only incident RCT, i.e., those teeth that had RCT initiated and completed after the baseline examination. For these teeth, follow-up started at the cycle when RCT was first detected from radiographs (i.e., the index cycle) and ended at the next examination cycle. At the next cycle, if there was a radiolucency detected around the root apex, the outcome was classified as “presence of post-operative AR” regardless of whether a lesion was present pre-operatively or whether it developed after treatment.
Determinations of root filling extension and density, in addition to AR, were made solely from available radiographs of diagnostic quality. Two second-year endodontic residents from Boston University independently reviewed study subjects’ intra-oral radiographs. Prior to data collection, a training and calibration session for the radiographic examiners was conducted to assure adequate reliability of radiographic examination and to evaluate diagnostic criteria for endodontic assessments. Kappa values describing inter-examiner reliability were excellent for the endodontic variables, ranging from 0.80–1.00, depending on the variable (22).
Diagnostic criteria for radiographic evaluation of AR, extension, and density were adapted from Odesjo et al. (23):
AR (both pre-operative and post-operative)
Present: periapical rarefaction contiguous with periodontal ligament space >1 mm wide, with absence of intact lamina dura.
Not present: apical periodontal ligament space < 1 mm thick
Multi-rooted teeth were classified as AR present if at least one root met the criteria for AR.
Extension
Under-extended: > 2 mm short of the radiographic apex
Well-extended: 0 – 2 mm short of the radiographic apex
Over-extended: root filling material beyond the radiographic apex
Multi-rooted teeth were classified as well-extended only if all roots were well-extended; over-extended if any roots were over-extended; and under-extended otherwise.
Density
Ideal: no voids or inhomogeneous zones visible, no space discernible between filling material and canal wall
Acceptable: no voids or inhomogeneous zones visible in apical third, no space discernible between filling material and canal wall in apical third
Defective: voids or inhomogeneous zone visible in apical third or space is discernible between filling material and canal wall in apical third (also includes any teeth with unfilled canals)
Multi-rooted teeth were classified according to the root filling with the worst density.
In addition to data collected from intra-oral radiographs, other variables were available from the parent VADLS data set and included in this study. Based on their temporal relationships, factors analyzed with respect to endodontic prognosis can be classified as pre-operative (e.g., presence of pre-operative AR, patient age, income, education, smoking, diabetes, hypertension, body mass index, tooth type), intra-operative (e.g., extension and density of root filling, treatment-related complications, year of RCT, type of root filling material, number of posts, post orientation), and post-operative (e.g., open access, crown) (18). Values for the covariates were taken from the index cycle for each tooth.
Statistical analyses were performed in three stages: 1) univariate description of data using frequencies and percentages; 2) bivariate associations between the main exposure variables and the outcome, with preliminary assessment of potential interactions and confounders using contingency tables and Chi-squared tests of proportions; and 3) multivariable logistic regression analyses to evaluate associations in the presence of other factors. Post-operative AR was the dichotomous dependent variable, with extension and density as explanatory variables of primary interest. Pre-operative AR was analyzed as an effect modifier to allow calculation of separate estimates of effect depending on whether a tooth had pre-operative AR, while other covariates were analyzed as potential confounders. Generalized Estimating Equations (GEE) were used to adjust for correlation of teeth within subjects (24, 25). All statistical tests were two-tailed and performed using SAS Version 9.1 (SAS Institute, Inc, Cary, NC).
RESULTS
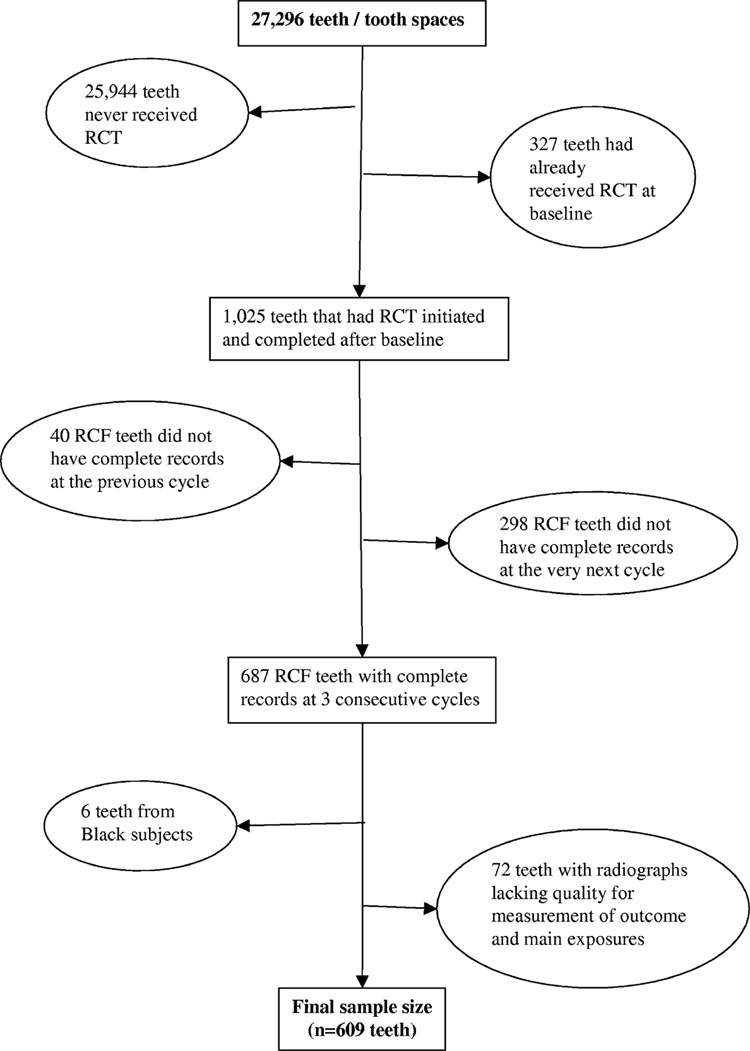
853 participants contributed a total of 27,296 teeth or tooth spaces (Figure). The present analysis included only the 609 teeth that received RCT after baseline and had complete data at three consecutive cycles (i.e., the cycle preceding the index cycle; the index cycle; and the very next cycle). 288 unique individuals contributed to the final sample, with the number of teeth per subject ranging from 1 to 11 (Table 1).
Figure.
Description of Study Sample
Table 1.
Number of Root Canal Filled (RCF) Teeth Contributed by Subjects
| Number of RCF teeth contributed per subject | Number of subjects (%) | Total number of RCF teeth contributed |
|---|---|---|
| 1 | 153 (53) | 153 |
| 2 | 58 (20) | 116 |
| 3 | 32 (11) | 96 |
| 4 | 18 (6) | 72 |
| 5 | 9 (3) | 45 |
| 6 | 10 (4) | 60 |
| 7 | 3 (1) | 21 |
| 8 | 1 (0) | 8 |
| 9 | 3 (1) | 27 |
| 10 | 0 (0) | 0 |
| 11 | 1 (0) | 11 |
| Total | 288 (100) | 609 |
Of the 609 analyzed teeth, 68 (11.2%) had post-operative AR at the end of follow-up (Table 2). Ideal density and adequate extension were observed in 216 teeth (35.5%), leaving 393 (64.5%) with unsatisfactory root filling quality. Pre-operative AR existed in 79 teeth (13.0%). The mean age of participants at the time of RCT for each tooth was 61 years. RCT-related complications were noted infrequently: “perforation” was seen in only 0.5%, “broken instruments” in 1.2%, “unfilled canals” in 1.3%, “unfilled roots” in 1.6%, and “insufficient length of root filling” (< 4 mm of root filling material in the most apical portion of the root canal) in 2.1% of teeth, respectively. In addition, only 3 teeth had open access and 11 teeth were from individuals who had diabetes. Because these occurrences were few, these variables were not analyzed further.
Table 2.
Univariate Distribution of Study Variables (N=609 Teeth)
| Variables | Level | Frequency | Percent (%) |
|---|---|---|---|
| Post-operative AR | Yes | 68 | 11.2 |
| (Outcome) | No | 541 | 88.8 |
| Extension | Under-extended | 85 | 14.0 |
| (Main exposure) | Over-extended | 122 | 20.0 |
| Well-extended | 402 | 66.0 | |
| Density | Acceptable | 154 | 25.3 |
| (Main exposure) | Defective | 158 | 25.9 |
| Ideal | 297 | 48.8 | |
| Pre-operative AR | Yes | 79 | 13.0 |
| No | 530 | 87.0 | |
| Filling material | Gutta percha only | 556 | 91.3 |
| Silverpoint or both | 53 | 8.7 | |
| Number of posts | ≥ 1 | 318 | 52.2 |
| 0 | 291 | 47.8 | |
| Post orientation | Off axis | 17 | 2.8 |
| On axis | 592 | 97.2 | |
| Crown | Yes | 344 | 56.5 |
| No | 265 | 43.5 | |
| Tooth type | Premolar | 213 | 35.0 |
| Molar | 184 | 30.2 | |
| Anterior | 212 | 34.8 | |
| Income a | > $25,000 per year | 200 | 32.8 |
| ≤ $25,000 per year | 397 | 65.2 | |
| Education | College graduate | 191 | 31.4 |
| Some college | 252 | 41.4 | |
| High school or less | 166 | 27.3 | |
| Smoking | Current smoker | 231 | 37.9 |
| Former smoker | 201 | 33.0 | |
| Never smoker | 177 | 29.1 | |
| Hypertension | Yes | 79 | 13.0 |
| No | 530 | 87.0 | |
| Year of RCT | ≥ 1985 | 270 | 44.3 |
| < 1985 | 339 | 55.7 | |
| Age at access | ≥ 65 years | 213 | 35.0 |
| 55 – 64.9 years | 245 | 40.2 | |
| < 55 years | 151 | 24.8 | |
| Body mass index a | ≥ 25 kg/m2 | 369 | 60.6 |
| 13 – 24.9 kg/m2 | 239 | 39.2 | |
n does not add to 609 due to missing values
Bivariate analyses (data not shown) showed defective density, pre-operative AR, and off-axis post orientation to be significantly associated with post-operative AR (p<0.05). Stratified analyses suggested an interaction between defective density and pre-operative AR, and preliminary assessment of potential confounders indicated that filling material, post orientation, the presence of a crown, tooth type, age, income, and smoking history were potential confounders.
In the final model (Table 3), defective density remained significantly associated with increased odds of post-operative AR after controlling for extension and pre-operative AR (P=0.028). The significant interaction term between defective density and pre-operative AR (P<0.0001) demonstrated that the effect of defective density on the odds of post-operative AR differed depending on whether the tooth had pre-operative AR. Using teeth with ideal density and no pre-operative AR as the reference group, odds ratios (95% CI) of post-operative AR were: 3.0 (1.3–7.1) for teeth with defective density but no preoperative AR; 29.2 (13.6–63.0) for teeth with ideal density and pre-operative AR; and 33.2 (12.0–92.0) for teeth with both defective density and pre-operative AR (Table 4). Controlling for the significant interaction term, neither acceptable density (relative to ideal density) nor extension was significantly associated with post-operative AR. However, when the under-extended and over-extended groups were combined into a single “poorly-extended” category, a significant association between poor extension and odds of post-operative AR was observed when compared with well-extended root fillings (Odds Ratio=1.8, 95% CI=1.1–3.2). Variables under investigation but not retained in the final model due to non-significance and minimal confounding included type of root filling material, post orientation, presence of crown, tooth type, age at access, income, smoking history, number of posts, year of RCT, education, hypertension, and body mass index.
Table 3.
Final Multivariable Logistic Regression Model of Associations between Explanatory Variables and Post-operative AR (N=609 Teeth)
| Independent Variable | Level | P-value | Odds Ratio (95% CI) |
|---|---|---|---|
| Extension | Under-extended | 0.199 | 1.7 (0.8, 3.4) |
| Over-extended | 0.082 | 2.0 (1.0, 3.9) | |
| Well-extended (reference) | --- | --- | |
| Density | Acceptable | 0.290 | 1.5 (0.7, 3.2) |
| Defective | 0.028 a | See Table 4 | |
| Ideal (reference) | --- | --- | |
| Pre-operative AR | Yes | <0.0001 a | See Table 4 |
| No (reference) | --- | --- | |
| Defective density * Pre-operative AR | See Table 4 | <0.0001 a | See Table 4 |
Statistically significant at 0.05 level
Table 4.
Assessment of Interaction Between Defective Density and Pre-operative AR in the Final Model (N=609 Teeth)
| Odds Ratio for Post-operative AR (95% CI) | Pre-operative AR |
||
|---|---|---|---|
| Yes | No | ||
| Density | Defective | 33.2 (12.0–92.0) | 3.0 (1.3–7.1) |
| Ideal | 29.2 (13.6–63.0) | 1.0 (reference) | |
Finally, because the impact of pre-operative AR was so strong, we performed an analysis restricted to the 530 teeth without pre-operative AR (Table 5). In this model, defective density remained the only explanatory variable significantly associated with increased odds of post-operative AR (P=0.022). Here, the combined category of poor extension conferred no significantly increased odds of post-operative AR (odds ratio=1.8, 95% CI=0.8–3.7). Income remained in the model due to its confounding effect on the main effects of interest, but its large P-value (0.798) indicates that income itself was not significantly predictive of post-operative AR.
Table 5.
Final Multivariable Logistic Regression Model of Associations Between Explanatory Variables and Post-operative AR (Restricted to N=530 Teeth Without Pre-operative AR)
| Independent Variable | Level | P-value | Odds Ratio (95% CI) |
|---|---|---|---|
| Extension | Under-extended | 0.460 | 1.5 (0.6–3.7) |
| Over-extended | 0.197 | 2.0 (0.8–5.1) | |
| Well-extended (reference) | --- | --- | |
| Density | Acceptable | 0.467 | 1.5 (0.5–4.6) |
| Defective | 0.022 a | 3.2 (1.3–8.2) | |
| Ideal (reference) | --- | --- | |
| Income | > $ 25,000 | 0.798 | 0.9 (0.4–2.0) |
| ≤ $25,000 (reference) | --- | --- | |
Statistically significant at 0.05 level
DISCUSSION
After controlling for pre-operative AR, defective density remained independently, significantly associated with post-operative AR. Voids in the root filling represent spaces that residual microflora could inhabit and subsequently transport endotoxins to the root apex, stimulating an inflammatory response (4). Our finding of significant interaction between pre-operative AR and defective density suggests that the effect of defective density differs depending on whether pre-operative AR exists; while our results confirm the importance of homogeneously dense root fillings, this especially is important when the tooth does not exhibit pre-operative AR.
Under- or over-extended root fillings might lead to a poorer prognosis compared to well-extended root fillings, but our analyses failed to show significant associations between either under- or over-extension and post-operative AR when other factors were considered simultaneously, no matter whether pre-operative AR existed or not. This finding agrees with some previous studies (26, 27) but differs from others (8, 14), and there are several possible explanations. In the case of under-extension, if space is left apical to the tip of the filling material but the apex is free of bacteria, under-extension is unlikely to increase the risk of periapical inflammation. In the case of over-extension, a small amount of excess root filling material extruded into the periapical area may be not enough to induce a significant foreign body reaction. Additionally, the number of teeth in the under- or over-extended group in our sample might be too small for statistically significant influences to be detected. To address this hypothesis, we collapsed under- and over-extended teeth into a single category and found that poor extension conferred significantly increased odds of post-operative AR compared to teeth with well-extended root fillings, but only in the presence of pre-operative AR; this would be consistent with inadequate eradication of bacteria from the root canal space. Radiographic assessment of root filling extension and density is more easily quantified than antibacterial management, which may have resulted in an overemphasis on these factors in some studies.
In the final regression model, pre-operative AR was of greater significance than other variables evaluated. This makes intuitive sense because a) teeth with pre-operative AR presumably already have bacteria present in the apical regions of their root canal systems while teeth without pre-operative AR might or might not have bacteria present there; and b) eradicating bacteria already present throughout the root canal system is more difficult than preventing bacteria from ever reaching the apical regions of the root. However, our study found a much greater impact of pre-operative AR on prognosis than that described previously. This could be explained in part by differences in diagnostic criteria used to define AR between the present study and other studies (28–30) or to differences in the study population and study design (31). For example, the present study participants are relatively older, so their ability to repair pre-existing periapical lesions might be less than in younger populations and thus they might be at greater risk for radiographically evident post-operative inflammation (32). It might take longer for an older host to heal an existing lesion even after well-performed RCT; it has been reported that delayed healing of periapical radiolucency could occur as long as 27 years after treatment (19). The 3-year follow up in our study might not have been sufficient for some pre-operative AR to heal completely.
In the presence of pre-operative AR, the effect of other factors investigated here seems less important, consistent with other studies (29, 33, 34). There are several possible explanations for this consistency. First, many investigated factors truly might not have a confounding effect. Second, the study might have insufficient power to detect relatively small effects associated with certain covariates. Finally, some covariates were excluded from regression modeling procedures because they either had too imbalanced a distribution or too few occurrences to provide meaningful point estimates and confidence intervals. Regardless, for most factors under investigation, the 288 subjects and 609 teeth provided a large enough sample for GEE methodology to produce consistent estimates (25).
A total of 327 RCF teeth were excluded from the analysis because they already had received RCT before baseline (Figure). Additional analyses (not shown here) revealed no meaningful differences between these 327 teeth and the 1025 teeth that received RCT after baseline, except that the excluded teeth tended to be from older subjects and were more likely to be anterior teeth. The prevalence of post-operative AR (11.2%) among the 609 analyzed RCF teeth is slightly lower than the frequencies of AR reported in the literature review. This could be partly because our study population is a community-based cohort, whereas previous studies mostly involved clinic patients. The satisfactory quality of root filling in this sample (35.5%) is comparable with the reported rate in the literature (i.e., 30–40%), which emphasizes the need for improving root filling quality in endodontic practice.
Only White males were included in the present study sample, so caution should be exercised when generalizing these results to other populations. However, because subjects received dental and medical care in the private sector, this sample likely was more socially diverse than participants recruited in many clinical studies, such as those conducted in dental schools or through dental insurance programs (4, 13–17). It is noteworthy, however, that there have been no consistent findings in the literature to indicate that root filling quality or outcome varies by race, ethnicity or sex.
As with all retrospective studies, data quality was dependent on the availability and completeness of documentation. Data collection for many variables was restricted to available information from the electronic database, and certain variables that may be related to post-operative AR were not available (e.g., bacterial levels in the root canal space and adequacy of the coronal restoration). With respect to the collected endodontic variables, potential misclassifications exist for several reasons. First, endodontic variables were assessed based on radiographs, and the use of two-dimensional radiographs to represent three-dimensional structures can be problematic in quantifying variables such as root filling extension and density. Second, this study operated under the assumption that post-operative AR is an undesired health outcome, given the general correlation between AR and histologically-confirmed inflammatory status of the periapical tissues (35). Third, assessment of periapical health did not involve clinical evaluation of study subjects. Though post-operative AR are not always associated with clinical symptoms (12), not all AR represent chronic apical periodontitis, but could instead be periapical cysts, foreign body reactions, or scar tissue. Finally, radiographic assessment is an uncertain process with wide variations among dentists, but this concern was minimized in our study by employing similarly trained examiners and calibrating them prior to data collection.
In conclusion, the major findings from this follow-up study were that: 1) defective root filling density was associated with increased odds of post-operative AR, but only among teeth without pre-operative AR; 2) the most significant risk factor for post-operative AR was the presence of pre-operative AR; 3) the statistical significance of root filling extension was dependent on how the variable was classified; and 4) none of the other tooth- or person-level covariates assessed was significantly related to post-operative AR. Failure of endodontic treatment is caused by microbes and their byproducts either being introduced into or remaining in the root canal system and periapical region, and root fillings with inadequate extension or density can only facilitate the infectious process.
Acknowledgments
The authors would like to thank Drs. Jeffrey Hutter and John Stamm, without whose assistance this study would not have been possible. The VA Dental Longitudinal Study and the VA Normative Aging Study are components of the Massachusetts Veterans Epidemiology Research & Information Center, VA Boston Healthcare System, Boston, MA. The studies are supported by the VA Cooperative Studies Program/ERIC, U.S. Department of Veterans Affairs. Dr. Garcia was the recipient of a Career Development Award in Health Services Research from VA HSR&D Service. He is supported by a VA Epidemiology Merit Review Award and by NIH grant K24-DE00419 from the National Institute of Dental and Craniofacial Research. The study also was supported by NIDCR Grant R01-DE13807.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Soikkonen KT. Endodontically treated teeth and periapical findings in the elderly. Int Endod J. 1995;28:200–203. doi: 10.1111/j.1365-2591.1995.tb00300.x. [DOI] [PubMed] [Google Scholar]
- 2.Weiger R, Hitzler S, Hermle G, Lost C. Periapical status, quality of root canal fillings and estimated endodontic treatment needs in an urban German population. Endod Dent Traumatol. 1997;13:69–74. doi: 10.1111/j.1600-9657.1997.tb00013.x. [DOI] [PubMed] [Google Scholar]
- 3.Marques MD, Moreira B, Eriksen HM. Prevalence of apical periodontitis and results of endodontic treatment in an adult, Portuguese population. Int Endod J. 1998;31:161–165. doi: 10.1046/j.1365-2591.1998.00136.x. [DOI] [PubMed] [Google Scholar]
- 4.Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J. 1995;28:12–18. doi: 10.1111/j.1365-2591.1995.tb00150.x. [DOI] [PubMed] [Google Scholar]
- 5.Kirkevang LL, Orstavik D, Horsted-Bindslev P, Wenzel A. Periapical status and quality of root fillings and coronal restorations in a Danish population. Int Endod J. 2000;33:509–515. doi: 10.1046/j.1365-2591.2000.00381.x. [DOI] [PubMed] [Google Scholar]
- 6.Tronstad L, Asbjornsen K, Doving L, Pedersen I, Eriksen HM. Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod Dent Traumatol. 2000;16:218–221. doi: 10.1034/j.1600-9657.2000.016005218.x. [DOI] [PubMed] [Google Scholar]
- 7.Hommez GM, Coppens CR, De Moor RJ. Periapical health related to the quality of coronal restorations and root fillings. Int Endod J. 2002;35:680–689. doi: 10.1046/j.1365-2591.2002.00546.x. [DOI] [PubMed] [Google Scholar]
- 8.Sjogren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16:498–504. doi: 10.1016/S0099-2399(07)80180-4. [DOI] [PubMed] [Google Scholar]
- 9.Farzaneh M, Abitbol S, Lawrence HP, Friedman S. Treatment outcome in endodontics-the Toronto Study. Phase II: initial treatment. J Endod. 2004;30:302–309. doi: 10.1097/00004770-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Kleinbaum DG, Klein M. Logistic regression: a self-learning text. 2nd edition. New York: Springer-Verlag Inc; 2002. [Google Scholar]
- 11.Caplan DJ, Slade GD, Gansky SA. Complex sampling: implications for data analysis. J Public Health Dent. 1999;59:52–59. doi: 10.1111/j.1752-7325.1999.tb03235.x. [DOI] [PubMed] [Google Scholar]
- 12.Friedman S. Prognosis of initial endodontic therapy. Endod Topics. 2002;2:59–88. [Google Scholar]
- 13.Trope M, Delano EO, Orstavik D. Endodontic treatment of teeth with apical periodontitis: single vs. multivisit treatment. J Endod. 1999;25:345–350. doi: 10.1016/S0099-2399(06)81169-6. [DOI] [PubMed] [Google Scholar]
- 14.Buckley M, Spangberg LS. The prevalence and technical quality of endodontic treatment in an American subpopulation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:92–100. doi: 10.1016/s1079-2104(05)80081-2. [DOI] [PubMed] [Google Scholar]
- 15.Chugal NM, Clive JM, Spangberg LS. A prognostic model for assessment of the outcome of endodontic treatment: Effect of biologic and diagnostic variables. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:342–352. doi: 10.1067/moe.2001.113106. [DOI] [PubMed] [Google Scholar]
- 16.Chugal NM, Clive JM, Spangberg LS. Endodontic infection: some biologic and treatment factors associated with outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:81–90. doi: 10.1016/s1079-2104(02)91703-8. [DOI] [PubMed] [Google Scholar]
- 17.Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30:846–850. doi: 10.1097/01.don.0000145031.04236.ca. [DOI] [PubMed] [Google Scholar]
- 18.Friedman S. Treatment outcome and prognosis of endodontic therapy. In: Ørstavik D, Pitt Ford TR, editors. Essential Endodontology. Prevention and treatment of apical periodontitis. Oxford: Blackwell Science Ltd; 1998. pp. 367–401. [Google Scholar]
- 19.Fristad I, Molven O, Halse A. Nonsurgically retreated root filled teeth--radiographic findings after 20–27 years. Int Endod J. 2004;37:12–18. doi: 10.1111/j.1365-2591.2004.00743.x. [DOI] [PubMed] [Google Scholar]
- 20.Garcia RI, Krall EA, Vokonas PS. Periodontal disease and mortality from all causes in the VA Dental Longitudinal Study. Ann Periodontol. 1998;3:339–349. doi: 10.1902/annals.1998.3.1.339. [DOI] [PubMed] [Google Scholar]
- 21.Krall EA, Garvey AJ, Garcia RI. Alveolar bone loss and tooth loss in male cigar and pipe smokers. J Am Dent Assoc. 1999;130:57–64. doi: 10.14219/jada.archive.1999.0029. [DOI] [PubMed] [Google Scholar]
- 22.Landis JR, Koch CG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 23.Odesjo B, Hellden L, Salonen L, Langeland K. Prevalence of previous endodontic treatment, technical standard and occurrence of periapical lesions in a randomly selected adult, general population. Endod Dent Traumatol. 1990;6:265–272. doi: 10.1111/j.1600-9657.1990.tb00430.x. [DOI] [PubMed] [Google Scholar]
- 24.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 25.Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS system. 2nd edition. Cary, NC: SAS Institute Inc; 2000. [Google Scholar]
- 26.Bystrom A, Happonen RP, Sjogren U, Sundqvist G. Healing of periapical lesions of pulpless teeth after endodontic treatment with controlled asepsis. Endod Dent Traumatol. 1987;3:58–63. doi: 10.1111/j.1600-9657.1987.tb00543.x. [DOI] [PubMed] [Google Scholar]
- 27.Sjogren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 1997;30:297–306. doi: 10.1046/j.1365-2591.1997.00092.x. [DOI] [PubMed] [Google Scholar]
- 28.Ørstavik D, Qvist V, Stoltze K. A multivariate analysis of the outcome of endodontic treatment. Eur J Oral Sci. 2004;112:224–230. doi: 10.1111/j.1600-0722.2004.00122.x. [DOI] [PubMed] [Google Scholar]
- 29.Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: the Toronto Study. Phase 1: initial treatment. J Endod. 2003;29:787–793. doi: 10.1097/00004770-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 30.Dugas NN, Lawrence HP, Teplitsky PE, Pharoah MJ, Friedman S. Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J. 2003;36:181–192. doi: 10.1046/j.1365-2591.2003.00640.x. [DOI] [PubMed] [Google Scholar]
- 31.Caplan DJ. Epidemiologic issues in studies of association between apical periodontitis and systemic health. Endodontic Topics. 2004;8:15–35. [Google Scholar]
- 32.Ashcroft GS, Mills SJ, Ashworth JJ. Ageing and wound healing. Biogerontology. 2002;3:337–345. doi: 10.1023/a:1021399228395. [DOI] [PubMed] [Google Scholar]
- 33.Aleksejuniene J, Eriksen HM, Sidaravicius B, Haapasalo M. Apical periodontitis and related factors in an adult Lithuanian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:95–101. doi: 10.1067/moe.2000.107059. [DOI] [PubMed] [Google Scholar]
- 34.Kirkevang LL, Wenzel A. Risk indicators for apical periodontitis. Community Dent Oral Epidemiol. 2003;31:59–67. doi: 10.1034/j.1600-0528.2003.00032.x. [DOI] [PubMed] [Google Scholar]
- 35.Ørstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2:20–34. doi: 10.1111/j.1600-9657.1986.tb00119.x. [DOI] [PubMed] [Google Scholar]