Abstract
Entrenched economic and gender inequities together are driving a globally expanding, increasingly female, human immunodeficiency virus (HIV)/AIDS epidemic. To date, significant population-level declines in HIV transmission have not been observed, at least in part because most approaches to prevention have presumed a degree of individual control in decision making that does not speak to the reality of women’s and girls’ circumstances in many parts of the world. Such efforts have paid insufficient attention to critical characteristics of the risk environment, most notably poverty and gender power inequities. Even fewer interventions have addressed specific mechanisms through which these inequities engender risky sexual practices that result in women’s disproportionately increased vulnerabilities to HIV infection. This article focuses on identifying those mechanisms, or structural pathways, that stem from the interactions between poverty and entrenched gender inequities and recommending strategies to address and potentially modify those pathways. We highlight four such structural pathways to HIV risk, all of which could be transformed: (1) lack of access to critical information and health services for HIV/sexually transmitted infection (STI) prevention, (2) limited access to formal education and skill development, (3) intimate partner violence, and (4) the negative consequences of migration prompted by insufficient economic resources. We argue for interventions that enhance women’s access to education, training, employment, and HIV/STI prevention information and tools; minimize migration; and by working with men and communities, at the same time reduce women’s poverty and promote gender-equitable norms. In conclusion, we identify challenges in developing and evaluating strategies to address these structural pathways.
Keywords: poverty, gender, HIV risk, structural pathways
Introduction
Entrenched economic and gender inequities together are driving the globally expanding female human immunodeficiency virus (HIV)/AIDS epidemic.1 Poverty and gender inequities operate cyclically: the myriad manifestations of poverty—insufficient income, restrictions in educational attainment and access to labor markets, and minimized decision-making autonomy—are fueled by inequities in gender-based norms and values and thus reinforce women’s lower social and economic status. This cycle is exacerbated by growth of the HIV epidemic, which is expected to escalate poverty rates and thus further increase women’s vulnerability to HIV.3
The HIV epidemic represents one of today’s most profound challenges in improving global health. Women represent a growing proportion among people living with HIV and AIDS, and the ratio of infected men to women is particularly skewed among young people. At the end of 2006, in sub-Saharan Africa, for every HIV-infected young man (15–24 years old) there were nearly three infected young women.4 Halting further expansion of the HIV pandemic within the next decade is a top priority of governments and civil society the world over and one of eight Millennium Development Goals set by the United Nations.5 Reaching this goal will hinge upon the success of prevention efforts in reducing women’s risk of HIV and other sexually transmitted infections (STIs).
Despite billions of dollars spent on programs designed to modify risky behavior, the annual number of incident HIV infections and other STIs has not declined.6,7 More than 80% of HIV infections occur through sexual contact with an infected partner8—infections that could have been prevented through the adoption of safer sexual practices, such as delayed sexual debut, abstaining from unprotected sex, and/or avoiding multiple and concurrent partnerships. Efforts to apply this knowledge to the development of interventions that lead to population-level reductions in HIV transmission have, however, had limited success.9 One possible explanation is that most approaches to prevention have presumed a degree of individual control in decision making that does not speak to the reality of women’s and girls’ circumstances in many parts of the world. Such efforts have paid insufficient attention to critical characteristics of the risk environment, most notably poverty and gender power inequities. Even fewer interventions to date have acted on the mechanisms through which these inequities lead to the risky sexual practices that result in women’s increased likelihood of infection.2 This article focuses on identifying those mechanisms, or structural pathways, that stem from the interactions between poverty and entrenched gender inequities and on recommending strategies to address and potentially modify those pathways.
At the outset, it must be acknowledged that HIV/AIDS is neither a women’s disease nor a disease of poverty alone. Men who have sex with men, individuals who inject drugs, and incarcerated populations are among the most vulnerable to HIV.4 Further, some data (such as those recently published from Tanzania and Kenya) have demonstrated a positive association between household wealth and HIV.10 These findings suggest that increased resources and greater mobility enable wealthier individuals to engage in high-risk sexual relationships more often than their lower-income counterparts.11 Such findings do not, however, contradict the general observation that because of their limited access both to economic and educational resources as well as to prevention information and tools,2 women and girls in many parts of the world are at increased HIV risk because of their dependency on and vulnerability to male partners.
The key challenge to reducing women’s HIV risk is to identify and act upon such structural pathways that link the underlying risk environment characterized by poverty and gender inequities and existing adverse health outcomes, such as HIV and other STIs. Here, we highlight four such structural pathways to HIV risk (Fig. 1), all of which could be transformed:
FIGURE 1.
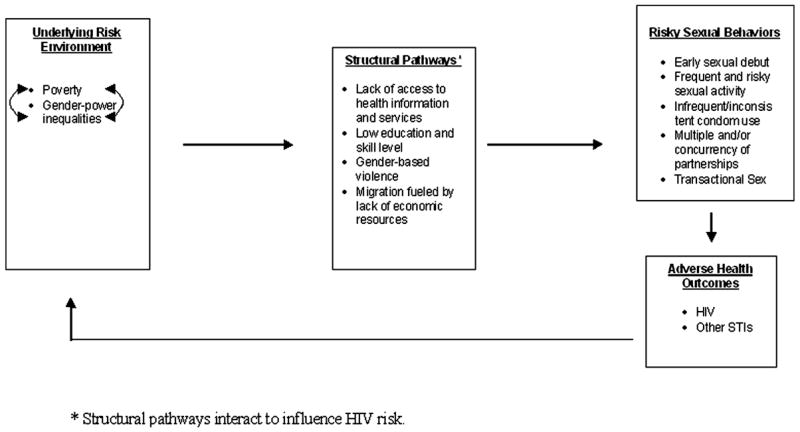
Structural pathways to HIV risk.
lack of access to critical information and health services for HIV/STI prevention;
limited access to formal education and skill development;
intimate partner violence (IPV); and
the negative consequences of migration prompted by insufficient economic resources.
Pathways 1 and 2 emerge directly from impoverished and skewed gender-power environments. IPV, although primarily the result of gender-power imbalances, is linked to and exacerbated by poverty. In contrast, migration is an example of a pathway that may be prompted by poverty and/or other socioeconomic and political conditions, such as conflict, economic collapse, and environmental disasters, and that intersects with gender-power inequities to disproportionately affect women’s HIV risk.
Below, we describe how each pathway links poverty, gender-power inequities, and HIV risk, and we discuss intervention strategies that we and others are exploring. We argue for those economic strategies that enhance women’s access to education, training, employment, and HIV/STI prevention information and tools; minimize migration; and by working with men and communities, at the same time reduce women’s poverty and promote gender-equitable norms. We conclude by identifying challenges in developing and evaluating strategies to address these structural pathways.
Pathways to HIV Risk
Because they condition and constrain the so-called choices available to vulnerable women and girls,12 the structural pathways highlighted here are directly linked to sexual risk-taking behaviors. For example, a significant risk behavior associated with HIV risk is transactional sex, which is tied to each of these pathways. Girls may unwittingly engage in risky sexual behaviors because they lack complete information about the risks they face or may be bound to enter into sexual relationships in exchange for food, clothing, or school fees. Similarly, many women may be compelled to engage in high-risk behaviors as a means to manage their economic situation, not only because their current options are limited but also because they cannot envision the potential for a better life. Others remain in violent, risky relationships as a result of economic dependency on male partners combined with social norms that condone male dominance. Thus, these pathways, by shaping the kinds of alternatives available and by influencing decision-making abilities, profoundly affect the HIV risk of women and girls. We elaborate on these observations below.
Lack of Access to Health Information and Services for HIV Prevention
Limited access to HIV prevention–related information and services is the one pathway linking poverty, gender-power inequities, and women’s HIV risk. Knowledge regarding HIV/AIDS is a necessary albeit insufficient resource for positive health behavior change.13 Evidence from sub-Saharan Africa and South Asia indicates that women are less likely than men to have adequate information about HIV transmission.14,15 Moreover, women belonging to poorer ethnic minority groups tend to have even less information. In Cambodia, analysis of Demographic and Health Survey data revealed that women in the wealthiest quintile were twice as likely to know how to prevent HIV transmission and nearly four times more likely to have information about HIV testing services than women in the poorest quintile.16 Similar findings have been reported in sub-Saharan Africa.15
Studies, such as those in Thailand and Kenya, have found that women are underrepresented among clients seeking voluntary counseling and testing (VCT)17,18 and STI diagnosis and treatment services,19–21 highlighting poverty and gender-related barriers to women’s use of what are widely recognized as cornerstones of HIV prevention.22–24 Women’s access to VCT is often associated with antenatal care services, which continue to be limited, particularly for poor women, in many countries.25 Seeking testing and treatment for HIV/STIs is particularly stigmatizing for women in many contexts, and they may risk the stability of their relationships in doing so.19,26,27
Limited Access to Formal Education and Skill Development
A second pathway to HIV risk, tied to that described above, is limited access to formal education and skill development. Lack of education and skills has myriad effects on girls’ and women’s HIV risk, for example, influencing their level of economic dependency on partners, the type of partners they have, and their likelihood of engaging in risky sexual behaviors. Even the cost of school fees, uniforms, and transport can propel girls into risky transactional relationships to pay for education.28 One longitudinal study in Kwazulu-Natal, South Africa, reported that girls who were not enrolled in school were more likely to have sex than those who were enrolled.29 Formal education for girls has been associated with improved knowledge and understanding of HIV and AIDS30; enhanced ability to act on HIV prevention messages,29 including acceptance of VCT services31; and increased power within relationships.32,33 Girls who received more education started having sex at a later age; had higher levels of condom use; experienced lower levels of coercive sex; were less likely to engage in transactional and/or intergenerational sex; and had lower odds of testing positive for at least one STI.29,34 Furthermore, education might shape girls’ perspective of the future, reducing the feeling of fatalism that sometimes justifies engaging in risky behaviors.29
Interactions between poverty and gender inequities contribute to the withholding of girls’ education. When families are stressed financially and cannot afford to educate all their children, the decision is often made to keep male rather than female children in school.35 In many cultural contexts, girls are intentionally kept out of school because families would rather have them carrying out domestic duties at home36 or because parents view education for girls as a waste of resources when they will soon be married off to other families.37,38 This gender gap is widest in Africa, the Middle East, and South Asia.39 Curtailed educational opportunities accompany early marriage, early initiation of sexual activity, and truncated future economic opportunities, serving to entrench further young women’s poverty and subordination and heighten their vulnerability to HIV.
Intimate Partner Violence
IPV, the most common and deadliest form of gender-based violence, is both more frequent and severe in lower socioeconomic groups40,41 and is closely associated with HIV risk.42–44 In a recent population-based study in 10 countries, 15%–71% of women reported physical or sexual violence by an intimate partner, and in most sites between 30% and 56% of these women reported both physical and sexual violence.45 IPV is now recognized as a key factor undermining women’s ability to control their reproductive and sexual health.46 Physical, sexual, and psychological manifestations of IPV decrease women’s ability to refuse sex with their intimate partner, to question their partner’s fidelity, and to request the use of barrier methods.46,47
The power imbalances reflected and reinforced by IPV may be skewed further when material goods and/or financial transactions are involved in a relationship.48 Often, accepting material goods or money indicates an acquiescence to engage in sexual intercourse on the man’s terms.48 Men who give material goods in exchange for sex are more likely to report multiple partners as well as violent and controlling behaviors than men who do not.49 Also, women who engage in transactional sex are more likely to experience IPV49 and to stay in abusive relationships that provide resources.49,50
Economic Migration and HIV/STI Risk
In much of South Asia and sub-Saharan Africa, millions of people living in poverty have no viable employment opportunities close to home, forcing individuals to migrate from their communities in search of higher wages and a means to provide economic resources for their families. Migrants, people who are mobile within populations and people with unstable living arrangements, tend to be at increased risk for HIV and STIs.51–53 Because of changing market demands and socioeconomic norms, women have become an increasingly larger proportion of the migrant population.52,54,55 Social and economic inequities, including gender norms, shape how migration influences HIV risk52,56,57; also, patterns of migration themselves influence the risk of HIV/STI transmission.
Women exposed to migration directly or indirectly, through the migration of their partner, experience a disproportionately heightened risk for HIV/STIs. Because disparities in formal education and vocational training leave women with fewer opportunities for employment, female migrants are exposed to economic vulnerabilities not experienced by their male counterparts. The persistence of a gender-based division of labor leads female migrants into low-status, low-paying jobs. Such inequities leave women economically vulnerable and even forced women to exchange sex for money, both formally and informally, as their only means of survival.58,59 As demonstrated by a study in China, for example, the prevalence of engaging in casual and commercial sex among female temporary migrants was substantially higher than that among female nonmigrants. In contrast, between male migrants and nonmigrants, the practice of casual and commercial sex did not vary.56
Isolated from the social protections provided by families and communities, female migrants experience violence (including IPV), rape, and sexual assault, both during the migration journeys52,57 and in destination communities.60 Even in regions where the migrants themselves are men, nonmigrating women may suffer an increased HIV risk due to male migration. For example, circular migration patterns with high frequency of partner return exponentially increase HIV risk among nonmigrating women who may be exposed to the virus on each visit home.61 Also, women left with little financial support while their partners are away have been found to engage in transactional sex as a means of economic survival.57 Furthermore, after long periods of separation from partners, women may seek emotional and physical comfort through new partnerships, which also increases opportunities for HIV and STI transmission.
Strategies That Address the Effect of Poverty and Gender Inequities on HIV Risk
Economic interventions affect women’s poverty can decrease their vulnerability to HIV infection in important ways. Such interventions, for example, may mitigate their need to stay in violent relationships or to engage in transactional sex. Although these strategies may facilitate change in prevailing inequitable gender norms, evidence suggests that these norms are more intransigent and require more direct focus. That is, economic strategies alone may be insufficient to address the structural pathways that result from the combined effects of poverty and gender-power inequities. Thus, approaches that work to reduce poverty while promoting gender equity, and vice versa, are more likely to have an enduring success. An integrated approach can profoundly alter the structural pathways to HIV, affecting the underlying risk environment, and thereby enhancing HIV prevention in ways not achieved by traditional methods of prevention.
Effective approaches to transform the structural pathways are likely to have two critical components: (1) an economic strategy to improve women’s access to education, training, and employment; enhance HIV/STI prevention information and tools; and/or minimize the necessity for migration and (2) gender transformation efforts, that is, strategies that challenge women and girls as well as men, families, and the broader community to question and rethink gender socialization and norms. Below we describe a few promising examples of these strategies.
Economic Interventions for Poverty Reduction
Three economic interventions stand out as having significant potential to address the structural pathways that derive from women’s experience of poverty: conditional cash transfers (CCTs), microcredit, and economic livelihoods. These strategies may not only address pathways, such as girls’ and women’s access to income, education, and health information and services, but also can reduce the necessity for migration prompted by economic insecurity, even within politically and economically unstable environments.62 Finally, these strategies can enhance decision-making abilities and even reduce IPV63 by empowering women and instilling optimism for the future.
One such economic intervention is CCTs. These programs link the receipt of cash transfers to individuals or households conditionally on certain behaviors, such as keeping children in school or visiting health centers for preventive care.64 Compelling evidence in favor of the promising effect of CCT interventions on structural pathways, such as access to education and health services, comes from one of the largest of such programs, Oportunidades, which is located in Mexico. In addition to national investments in the health care and educational systems to improve availability of services, Oportunidades offered cash transfers to poor families conditionally on their participation in primary health center visits and children’s school attendance. Major findings from a community randomized controlled trial of the program included an overall increase in household income, a 40% reduction in childhood and adult illness, improved child nutrition, and improved consistency with school attendance.64–66 Evaluations of similar programs in Nicaragua and Columbia have shown comparable effects.
Microcredit is a second promising economic strategy that provides small loans to the poor outside formal banking structures, usually through group lending models. Because loans are guaranteed by each member of the group, this collective guarantee overcomes the need for collateral required by formal banks and has the secondary benefit of promoting social and community relations that build social capital.67 A recent review of studies conducted on microcredit programs involving women showed significant increases in household income, contraceptive use, and child nutrition. However, these effects were diminished among women who had relatively less control over their income (highlighting the importance of addressing gender norms).68 Although microcredit can greatly reduce poverty, this strategy may not be appropriate for all population groups, such as the poorest of the poor or youth, for whom taking loans may only propel them into greater poverty and therefore greater risk.69 In such cases, a broader array of microfinance services, such as microgrants (capital that is not repaid) and saving programs, either alone or in combination with livelihoods promotion (described below), may be more appropriate.68,69
The goal of an economic livelihood approach, our third example of promising economic interventions, is to enhance the capabilities, resources, and opportunities that enable individuals to pursue their economic goals.70 This approach entails building capabilities through training in life skills, formal and informal education, enhancing self-confidence, facilitating the formation of peer and social support networks, and promoting decision-making ability. It seeks to increase such resources as physical assets (e.g., housing, land, and infrastructure), social assets (e.g., social ties, networks, and trusting relationships), and, when appropriate, financial assets (e.g., loans and savings). Finally, it expands participants’ current and future opportunities through vocational, job, and business training; financial literacy; and/or linkages to microfinance. Although this approach could be targeted to a variety of population groups, recent interest has focused on women and adolescents, and in particular girls and orphans.71
Strategies for Gender Transformation
Enhancing the strategies described above to specifically address gender-power inequities directly is critical to their success in mitigating the effects of structural pathways to HIV infection on women. Many microcredit and livelihood programs have begun to address gender norms through life skills training and HIV education; the social support and peer networks inherent in the design of these programs can foster not just individual- but also group-level changes in perceptions of gender. This assertion is supported by recent research that has demonstrated that focused educational activities in small-group settings can lead to the adoption of gender-equitable attitudes.72 Recently, the IMAGE study conducted in South Africa evaluated the effectiveness of a microcredit program combined with gender education in reducing HIV risk behavior and acquisition among women. Although researchers found a decrease in reported IPV among those in the intervention villages, they detected no change in HIV incidence or the rate of unprotected sexual intercourse with a nonspousal partner.73
Similarly, CCT programs could target low education levels and poor health service utilization more directly while working to reduce gender inequities. For example, greater incentives could be provided to families to keep girls in school than boys. Evidence suggests that when support is provided for girls’ education, families are more likely to send boys as well.74 CCT could also be used to increase women’s uptake of preventive reproductive health care or VCT, mitigating poverty- and gender-related barriers to health service utilization.
Transforming gender norms also entails working with men. During the last decade, there has been increasing recognition of the importance of addressing the links among gender norms, risky male sexual behavior, and women’s HIV risk.75 This recognition has been accompanied by a variety of efforts to involve men in reproductive health promotion, to work with men as partners, and to focus on men’s sexual health and HIV risk.75,76 Whereas the first two have engaged men on issues, such as safe motherhood and family planning, the last emphasized the need to meet men’s own sexual and reproductive health needs. All three approaches have demonstrated some change in knowledge; gender-related attitudes; and to a limited extent, behaviors (including gender-based violence and sexual risk behaviors) within relatively short project time-frames.77,78
Creating an enabling environment for change also requires support from families and communities.79 Relatively few HIV prevention interventions have focused on families. One promising example is CHAMP (Collaborative HIV Prevention and Adolescent Mental Health Project), which was originally developed in the United States and later adapted for South African and Caribbean settings.80,81 A preliminary study of CHAMP in South Africa and Trinidad and Tobago suggested that the intervention improved parental knowledge of HIV transmission, increased communication between parents and youth on sensitive topics, such as puberty and sex, and reduced HIV/AIDS stigma among parents. Another similar strategy is the motivation of a diverse set of community actors (e.g., key opinion leaders, youth groups, local businesses, or community-based organizations) to tackle a common concern, such as HIV/AIDS.82 Such community mobilization may include community-employed health workers to engage in HIV prevention, care and support activities, and the organization of HIV/AIDS awareness rallies. Although promising, the effect of these efforts on HIV risk remains to be investigated.
Although evidence suggests that young women who believe that their future economic prospects are bright are less likely to engage in risky behavior,83 few economic interventions either alone or combined with gender education/transformation (except the IMAGE study described earlier73) components have yet targeted or been rigorously evaluated for reducing HIV infection. Nevertheless, we posit that these promising multicomponent strategies, which simultaneously address women’s poverty and gender-power inequities, can greatly reduce HIV risk among women and girls in ways not achieved previously.
Challenges and Conclusions
From the available evidence, a strong case can be made for framing individual HIV risk as the result of much more than biology and individual behavior. Risk is a complex construct, shaped and conditioned by the environment, of which poverty and gender-power inequities are critical components. Comprehending, predicting, and explaining the influence of the risk environment is critical for developing effective HIV prevention interventions. In this article, we have highlighted several structural pathways that mediate the influence of the risk environment on individual choice and behaviors that lead to HIV infection. These pathways are connected and have overlapping influences on individuals. For example, young women’s limited access to education and skills is associated with migration in search of economic opportunities, and both in turn constrain women’s resources and decisions, increasing the likelihood of transactional sex.
HIV prevention strategies that focus solely on individual decisions and risk behaviors are unlikely to be optimally effective. Rather, strategies that acknowledge and address pathways through which the risk environment impinges upon individual choices have the greatest potential. These approaches emphasize working with young people, whose identities are still forming and therefore amenable to change.75 Although few strategies focusing on expanding young women’s economic resources, such as CCT or livelihood programs, have yet targeted or been evaluated specifically for reducing HIV infection, they have had some effect on several of the structural pathways to HIV infection, including increased access to health services and improved information, skills, and education for women and girls. Interventions that have focused on men and communities have demonstrated that gender norms are in fact amenable to change. Although none of these approaches alone is likely to substantially affect the structural pathways resulting from poverty and gender-power inequities, they can do so when combined.
The relevance, appropriateness, and success of such strategies are likely to be shaped by the ways in which poverty and gender-power inequities manifest themselves in communities at particular points in time. Missing from our discussion are the ways in which communities’ history, culture, and politics determine the nature of poverty and gender-power inequities and modify these structural pathways and their influence on individuals. Choosing an appropriate strategy will entail understanding these multiple dimensions of the risk environment and will require applying context-specific social science research.
Strategies that address the structural pathways from risk environment to risk behaviors are likely to involve partnerships and collaborations between communities, practice-based organizations, and researchers.84 The nature of these alliances and the power dynamics within them can have a profound influence on the process of implementation and change, exemplified by the following comment by Potvin et al.: “The main barriers are the time-consuming nature of the negotiation process, the absence of a common language, and the need to design research activities that both respect people’s real preoccupations and are compatible with a goal of ‘empowering the community.’”84
Once a potential strategy based on an understanding of local contexts is identified, a key challenge is to ensure that implementation is accompanied by systematic monitoring and evaluation to detect their effects on HIV risk. Accumulating evidence on the effect of these approaches is likely to be hampered because changes in gender norms take place over a longer time than program evaluations, and thus a change in HIV infection might become manifest even after this. Furthermore, the complexities of these approaches, in terms of strategies used and constituencies involved, is likely to pose a major challenge to evaluating their effect. In these contexts, new ways of thinking about generating evidence on effectiveness will need to be developed.85
Most importantly, although promising intervention models may exist, there is inadequate understanding of how such models (if effective) can be scaled up. More resources will need to be invested in research to explore and specify the process of replication and scaleup of effective approaches. In the longer term, collaborative relationships among communities, public health practitioners, and researchers that address the pathways to HIV risk that emanate from the underlying interactions between poverty and gender inequities offer the greatest promise to redressing the inequities and injustices that fuel this epidemic.
Acknowledgments
We thank Maria Vivas, Julie Roley, and Kalyani Subbiah. The following authors received research and salary support from the National Institute of Chile Health and Human Development: Krishnan (R01 HD41731 and the Presidential Early Career Award for Scientists and Engineers 2005), Minnis (K01 HD047434), and Dunbar and Padian (R01 HD045135-04). Dunbar and Padian also received support from the Office of AIDS Research, Office of the Director of the National Institutes of Health (R01 HD045135-04), and the Tides Foundation. Minnis and Padian received partial support from the National Institute of Allergies and Infectious Diseases (R01-AI48749). Minnis received additional research and salary support from the University of California Institute for Mexico and the U.S., California-Mexico Health Initiative, UC Office of the President, National Institute of Child Health and Human Development. Medlin and Padian received support from the NIH Roadmap Exploratory Centers for Interdisciplinary Research (P20 RR020817).
Footnotes
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.UNAIDS/UNFPA/UNIFEM. 2004. Women and HIV/AIDS: confronting the Crisis.
- 2.Loewenson R. Exploring equity and inclusion in the responses to AIDS. AIDS Care. 2007;19:S2–S11. doi: 10.1080/09540120601114790. [DOI] [PubMed] [Google Scholar]
- 3.Loewenson RW, Whiteside A. HIV/AIDS: Implications for Poverty Reduction. United Nations Development Programme; New York: 2001. [Google Scholar]
- 4.UNAIDS. Report on the Global AIDS Epidemic.2006. [Google Scholar]
- 5.United Nations Millennium Project. Investing in development: a practical plan to achieve the millennium development goals. Overview 2005 [Google Scholar]
- 6.UNAIDS. 2005. AIDS Epidemic Update 2005.
- 7.UNAIDS. 2006. 2006 Report on the Global AIDS Epidemic.
- 8.Askew I, Berer M. The contribution of sexual and reproductive health services to the fight against HIV/AIDS: a review. Reprod Health Matters. 2003;11:51–73. doi: 10.1016/s0968-8080(03)22101-7. [DOI] [PubMed] [Google Scholar]
- 9.Bertozzi S, Padian NS, Wegbreit J, et al. HIV/AIDS prevention and treatment. In: Jamison DB, et al., editors. Disease Control Priorities in Developing Countries. 2. Oxford University Press and The World Bank; Washington, DC: 2006. pp. 331–369. [Google Scholar]
- 10.Shelton J, Cassell M, Adetunji J. Is poverty or wealth at the root of HIV? Lancet. 2005;366:1057–1058. doi: 10.1016/S0140-6736(05)67401-6. [DOI] [PubMed] [Google Scholar]
- 11.Fenton L. Preventing HIV/AIDS through poverty reduction: the only sustainable solution? Lancet. 2004;364:1186–1187. doi: 10.1016/S0140-6736(04)17109-2. [DOI] [PubMed] [Google Scholar]
- 12.Kabeer N. Resources, agency, achievements: reflections on the measurement of women’s empowerment. Dev Change. 1999;30:435–464. [Google Scholar]
- 13.Kowalewski M, Henson K, Longshore D. Rethinking perceived risk and health behavior: a critical review of HIV prevention research. Health Educ Behav. 1997;24:313–325. doi: 10.1177/109019819702400305. [DOI] [PubMed] [Google Scholar]
- 14.World Bank. South Asia Multisector Briefs on HIV/AIDS. The World Bank; Washington, DC: 2006. [Google Scholar]
- 15.UNAIDS. 2005. AIDS Epidemic Update: December 2005.
- 16.Bloom D, Associates RP, Sevilla J. Health, wealth, AIDS and poverty. Asian Development Bank; Manila, Philippines: 2002. [Google Scholar]
- 17.Taegtmeyer M, Kilonzo N, Mung’ala L, et al. Using gender analysis to build voluntary counselling and testing responses in Kenya. Trans R Soc Trop Med Hyg. 2006;100:305–311. doi: 10.1016/j.trstmh.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 18.Khongphatthanayothin M, Tantipaibulvut S, Nookai S, et al. Demographic predictors of a positive HIV test result among clients attending a large metropolitan voluntary counselling and testing centre in Thailand. HIV Med. 2006;7:281–284. doi: 10.1111/j.1468-1293.2006.00377.x. [DOI] [PubMed] [Google Scholar]
- 19.Malta M, Bastos F, Strathdee S, et al. Knowledge, perceived stigma, and care- seeking experiences for sexually transmitted infections: a qualitative study from the perspective of public clinic attendees in Rio de Janeiro, Brazil. BMC Public Health. 2007;7:18. doi: 10.1186/1471-2458-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fonck K, Mwai C, Ndinya-Achola J, et al. Health-seeking and sexual behaviors among primary healthcare patients in Nairobi, Kenya. Sex Transm Dis. 2002;29:106–111. doi: 10.1097/00007435-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Go V, Quan V, Chung A, et al. Barriers to reproductive tract infection (RTI) care among Vietnamese women—Implications for RTI control programs. Sex Transm Dis. 2002;29:201–206. doi: 10.1097/00007435-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Grosskurth H, Mosha F, Todd J, et al. Impact of improved treatment of sexually-transmitted diseases on HIV infection in rural Tanzania—randomized controlled trial. Lancet. 1995;346:530–536. doi: 10.1016/s0140-6736(95)91380-7. [DOI] [PubMed] [Google Scholar]
- 23.Wolitski R, MacGowan R, Higgins D, et al. The effects of HIV counseling and testing on risk-related practices and help-seeking behavior. AIDS Educ Prev. 1997;9:52–67. [PubMed] [Google Scholar]
- 24.WHO. Guidance on provider-initiated HIV testing and counseling in health facilities. 2007. [Google Scholar]
- 25.Coovadia HM. Access to voluntary counseling and testing for HIV in developing countries. Prev Treatment HIV Infect Infants Children. 2000;918:57–63. doi: 10.1111/j.1749-6632.2000.tb05474.x. [DOI] [PubMed] [Google Scholar]
- 26.Voeten HACM, O’Hara H, Kusimba J, et al. Gender differences in health care-seeking behavior for sexually transmitted diseases—a population-based study in Nairobi, Kenya. Sex Transm Dis. 2004;31:265–272. doi: 10.1097/01.olq.0000124610.65396.52. [DOI] [PubMed] [Google Scholar]
- 27.Lichtenstein B. Stigma as a barrier to treatment of sexually transmitted infection in the American deep south: issues of race, gender and poverty. Soc Sci Med. 2003;57:2435–2445. doi: 10.1016/j.socscimed.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 28.Longfield K, Glick A, Waithaka M, Berman J. Relationships between older men and younger women: implications for STIs/HIV in Kenya. Stud Fam Plann. 2004;35:125–134. doi: 10.1111/j.1728-4465.2004.00014.x. [DOI] [PubMed] [Google Scholar]
- 29.Kaufman CE, Clark S, Manzini N, et al. Communities, opportunities, and adolescents’ sexual behavior in KwaZulu-Natal, South Africa. Stud Fam Plann. 2004;35:261–274. doi: 10.1111/j.0039-3665.2004.00030.x. [DOI] [PubMed] [Google Scholar]
- 30.Hargreaves J, Boler T. Education and HIV Series 01. 2006. Girl power: the impact of girls’ education on HIV and sexual behaviour. [Google Scholar]
- 31.Sherr L, Lopman B, Kakowa M, et al. Voluntary counselling and testing: uptake, impact on sexual behaviour, and HIV incidence in a rural Zimbabwean cohort. AIDS. 2007;21:851–860. doi: 10.1097/QAD.0b013e32805e8711. [DOI] [PubMed] [Google Scholar]
- 32.Crosby R, DiClemente R, Wingood G, et al. The protective value of school enrolment against sexually transmitted disease: a study of high-risk African American. Sex Transm Infect. 2007;83:223–227. doi: 10.1136/sti.2006.022590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DiClemente RLS, Crosby R, Rosenthal S. Prevention and control of sexually transmitted infection among adolescents: the importance of a sociecological perspective- a commentary. Public Health. 2005;119:825–836. doi: 10.1016/j.puhe.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 34.Crosby R, DiClemente R, Wingood G, et al. The protective value of school enrollment against sexually transmited disease: a study of high-risk African American. Sex Transm Infect. 2007;83:223–227. doi: 10.1136/sti.2006.022590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.UNESCO. Education for all. Who is excluded and why. 2004. [Google Scholar]
- 36.UNAIDS. UNAIDS Best Practice Collection. 1999. Gender and HIV/AIDS: taking stock of research and programmes. [Google Scholar]
- 37.De Bruyn M. Women and AIDS in developing countries. J Soc Sci Med. 1992;34:249–263. doi: 10.1016/0277-9536(92)90267-t. [DOI] [PubMed] [Google Scholar]
- 38.Hunter S. Orphans as a window on the AIDS epidemic in sub-Saharan Africa: initial results and implications of a study in Uganda. J Soc Sci Med. 1990;31:681–690. doi: 10.1016/0277-9536(90)90250-v. [DOI] [PubMed] [Google Scholar]
- 39.UNICEF. Gender Achievements and Prospects. GAP Report. 2005. [Google Scholar]
- 40.Martin S, Tsui A, Maitra K, et al. Domestic violence in northern India. Am J Epidemiol. 1999;150:417–426. doi: 10.1093/oxfordjournals.aje.a010021. [DOI] [PubMed] [Google Scholar]
- 41.Jewkes R. Intimate partner violence: causes and prevention. Lancet. 2002;359:1423–1429. doi: 10.1016/S0140-6736(02)08357-5. [DOI] [PubMed] [Google Scholar]
- 42.Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse. 2007;8:149–177. doi: 10.1177/1524838007301162. [DOI] [PubMed] [Google Scholar]
- 43.Maman S, Campbell J, Sweat MD, et al. The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med. 2000;50:459–478. doi: 10.1016/s0277-9536(99)00270-1. [DOI] [PubMed] [Google Scholar]
- 44.Martin SL, Kilgallen B, Tsui AO, et al. Sexual behaviors and reproductive health outcomes—associations with wife abuse in India. JAMA. 1999;282:1967–1972. doi: 10.1001/jama.282.20.1967. [DOI] [PubMed] [Google Scholar]
- 45.Garcia-Moreno C, Jansen H, Ellsberg M, et al. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368:1260–1269. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 46.Heise L, Ellsberg M, Gottmoeller M. A global overview of gender-based violence. Int J Gynecol Obstet. 2002;78:S5–S14. doi: 10.1016/S0020-7292(02)00038-3. [DOI] [PubMed] [Google Scholar]
- 47.Blanc AK. The effect of power in sexual relationships on sexual and reproductive health: an examination of the evidence. Stud Fam Plann. 2001;32:189–213. doi: 10.1111/j.1728-4465.2001.00189.x. [DOI] [PubMed] [Google Scholar]
- 48.Dunkle K, Jewkes R, Nduna M, et al. Transactional sex with casual and main partners among young South African men in the rural Eastern Cape: prevalence, predictors, and associations with gender-based violence. Soc Sci Med. 2007;65:1235–1248. doi: 10.1016/j.socscimed.2007.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dunkle KRJ, Brown H, et al. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med. 2004;59:1581–1592. doi: 10.1016/j.socscimed.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 50.Kaufman C, Stavrous S. ‘Bus fare please’: the economics of sex and gifts among young people in urban South Africa. Cult Health Sex. 2004;6:377–391. [Google Scholar]
- 51.Hatton T, Williamson J. Demographic and economic pressure on emigration out of Africa. Scand J Econ. 2003;105:465–486. [Google Scholar]
- 52.DeHaan A. Livelihoods and poverty: the role of migration—a critical review of the migration literature. J Dev Stud. 1999;36:1–47. [Google Scholar]
- 53.Lurie M. The epidemiology of migration and HIV/AIDS in South Africa. J Ethn Migr Stud. 2006;32:649–666. [Google Scholar]
- 54.Mercer A, Khanam R, Gurley E, et al. Sexual risk behavior of married men and women in Bangladesh associated with husbands’ work migration and living apart. Sex Transm Dis. 2007;34:265–273. doi: 10.1097/01.olq.0000240384.61924.65. [DOI] [PubMed] [Google Scholar]
- 55.Lucas R. Migration and economic development in Africa: a review of evidence. J Afr Econ. 2006;15:337–395. [Google Scholar]
- 56.Yang X, Xia G. Gender, migration, risky sex, and HIV infection in China. Stud Fam Plann. 2006;37:241–250. doi: 10.1111/j.1728-4465.2006.00103.x. [DOI] [PubMed] [Google Scholar]
- 57.Wardlow H. Men’s extramarital sexuality in rural Papua New Guinea. Am J Public Health. 2007;97:1006–1014. doi: 10.2105/AJPH.2006.088559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang B, Stanton B, Fang X, et al. HIV-related risk behaviors and history of sexually transmitted diseases among male migrants who patronize commercial sex in China. Sex Transm Dis. 2007;34:1–8. doi: 10.1097/01.olq.0000222668.95038.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huang Y. Gender, hukou, and the occupational attainment of female migrants in China (1985/1990) Environ Plann. 2001;3:257–279. [Google Scholar]
- 60.Puri M, Cleland J. Sexual behavior and perceived risk of HIV/AIDS among young migrant factory workers in Nepal. J Adolesc Health. 2006;28:237–246. doi: 10.1016/j.jadohealth.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 61.Gray R, Li X, Wawer M, et al. Determinants of HIV-1 load in subjects with early and later HIV infections, in a general-population cohort of Rakai, Uganda. J Infect Dis. 2004;189:1209–1215. doi: 10.1086/382750. [DOI] [PubMed] [Google Scholar]
- 62.Boungou Bazika J. Effectiveness of small scale income generating activities in reducing risk of HIV in youth in the Republic of Congo. AIDS Care. 2007;19:23–24. doi: 10.1080/09540120601114444. [DOI] [PubMed] [Google Scholar]
- 63.Schuler S, Hashemi S, Riley A. The influence of women’s changing roles and status in Bangladesh’s fertility transition: evidence from a study of credit programs and contraceptive use. World Dev. 1997;25:563–575. [Google Scholar]
- 64.Rawlings B, Rubio M. Evaluating the impact of conditional cash transfer programs. World Bank Res Obs. 2005;20:29–55. [Google Scholar]
- 65.Gertler P. Do conditional cash transfers improve child health? Evidence from Progresa’s control randomized experiment. Am Econ Rev. 2004;94:336–341. doi: 10.1257/0002828041302109. [DOI] [PubMed] [Google Scholar]
- 66.Gertler, P. 2000. Final Report: The Impact of Progesa on Health. International Food Policy Research Institute, Food Consumption and Nutrition Division.
- 67.UNICEF. 2004. The Role of Social Support and Economic Skill Building Programs in Mitigating Adolescents’ Vulnerabilities: Perspectives and UNICEF’s Experience to Date.
- 68.Goldberg, N. 2005. Measuring the impact of microfinance: taking stock of what we know. Grameen Foundation USA Publication Series.
- 69.Dunbar M, Kang M-S, Laver S, et al. Combining economic livelihood and behavioral interventions to reduce HIV/STI risk among adolescent female orphans in Zimbabwe. International Society for Sexually Transmitted Disease Research.2005. [Google Scholar]
- 70.Chambers R, Conway G. Discussion paper no. 296. 2000. Sustainable Rural Livelihoods: Practical Concepts for the 21st Century. [Google Scholar]
- 71.Masanjala W. The poverty-HIV/AIDS nexus in Africa: a livelihood approach. Soc Sci Med. 2007;64:1032–1041. doi: 10.1016/j.socscimed.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 72.Barker, G. 2006. Engaging boys and men to empower girls: reflections from practice and evidence of impact. United Nations Division for the Advancement of Women, EGM/DVGC/2006/EP.3: 15–21.
- 73.Pronyk P, Hargreaves J, Kim J, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368:1973–1983. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 74.Kim J, Alderman H, Orazem PF. Can private school subsidies increase enrollment for the poor? The Quetta Urban Fellowship Program. World Bank Econ Rev. 1999;13:443–465. [Google Scholar]
- 75.Agardh A, Egerö B, Eriksson N, et al. Article no. SIDA37158en: 1–34. 2007. Men Matter! AIDS, Gender and Masculinities. Sida Department of Democracy and Social Development. [Google Scholar]
- 76.Interagency Gender Working Group and Who. A Summary of the ‘So What?’ report: A look at whether integrating a gender focus into programmes makes a difference. Population Reference Bureau; Washington, DC: 2005. [Google Scholar]
- 77.Wilder J, Masilamani R, Daniel E. Promoting change in the reproductive behavior of youth: Pathfinder International’s PRACHAR Project, Bihar, India. Pathfinder International; New Delhi: 2005. pp. 1–28. [Google Scholar]
- 78.Pulerwitz J, Barker G, Segundo M. Promoting healthy relationships and HIV/STI prevention for young men: Positive findings from an intervention study in Brazil. Population Council and Instituto PROMUNDO; 2004. Research Update. [Google Scholar]
- 79.Painter TM. Voluntary counseling and testing for couples: a high-leverage intervention for HIV/AIDS prevention in sub-Saharan Africa. Soc Sci Med. 2001;53:1397–1411. doi: 10.1016/s0277-9536(00)00427-5. [DOI] [PubMed] [Google Scholar]
- 80.Baptiste DR, Bhana A, Petersen I, et al. Community collaborative youth- focused HIV/AIDS prevention in South Africa and Trinidad: preliminary findings. J Pediatr Psychol. 2006;31:905–916. doi: 10.1093/jpepsy/jsj100. [DOI] [PubMed] [Google Scholar]
- 81.Voisin DR, Baptiste DR, Da Costa D, et al. Exporting a USHI/VAIDS prevention program to a Caribbean island-nation—lessons from the field. Int Soc Work. 2006;49:75–86. [Google Scholar]
- 82.Ziff MA, Harper GW, Chutuape KS, et al. Laying the foundation for Connect to Protect (R): a multi-site community mobilization intervention to reduce HIVAIDS incidence and prevalence among urban youth. J Urban Health. 2006;83:506–522. doi: 10.1007/s11524-006-9036-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Peter Aggleton CC. Young people’s sexual health: a framework for policy debate. Can J Hum Sex. 1999;8:249–262. [Google Scholar]
- 84.Potvin L, Cargo M, McCombera A, et al. Implementing participatory intervention and research in communities: lessons from the Kahnawake Schools Diabetes Prevention Project in Canada. Soc Sci Med. 2003;56:1295–1305. doi: 10.1016/s0277-9536(02)00129-6. [DOI] [PubMed] [Google Scholar]
- 85.McQueen DV. Perspectives on health promotion: theory, evidence, practice and the emergence of complexity. Health Promot Int. 2000;15:95–97. [Google Scholar]


