Abstract
Overexpression of transforming growth factor β (TGF-β) is frequently associated with metastasis and poor prognosis, and TGF-β antagonism has been shown to prevent metastasis in preclinical models with surprisingly little toxicity. Here we have used the transplantable 4T1 model of metastatic breast cancer to address underlying mechanisms. We showed that efficacy of the anti-TGF-β antibody 1D11 in suppressing metastasis was dependent on a synergistic combination of effects on both the tumor parenchyma and microenvironment. The main outcome was a highly significant enhancement of the CD8+ T-cell mediated anti-tumor immune response, but effects on the innate immune response and on angiogenesis also contributed to efficacy. Treatment with 1D11 increased infiltration of NK cells and T cells at the metastatic site, and enhanced expression of coactivators (NKG2D) and cytotoxic effectors (perforin and granzyme B) on CD8+ T-cells. On the tumor cells, increased expression of an NKG2D ligand (Rae1γ) and of a death receptor (TNFRSF1A) contributed to enhanced immune cell-mediated recognition and lysis. The data suggest that elevated TGF-β expression in the tumor microenvironment modulates a complex web of intercellular interactions that aggregately promote metastasis and progression. TGF-β antibodies reverse this effect, and the absence of a major effect of TGF-β antagonism on any one cell compartment may be critical for a good therapeutic window and the avoidance of autoimmune complications.
Keywords: metastasis, anti-TGF-β, immune surveillance, mouse models, breast cancer
Introduction
The past decade has seen a dramatic increase in the number of molecularly targeted therapeutics entering the clinic for the treatment of cancer. Such therapeutics generally either target driving oncogenic lesions within the tumor (eg. Herceptin), or interfere with the establishment or maintenance of a tumor-permissive stroma (eg. Avastin). TGF-βs are pleiotropic growth factors whose overexpression by many advanced tumors correlates with metastasis and poor prognosis (1-4). Emerging evidence suggests that TGF-βs are important mediators of the dynamic and reciprocal interactions between the tumor parenchyma and cells of the tumor microenvironment (5), so targeting this pathway offers the attractive possibility of impacting on both compartments simultaneously.
The complex biology of the TGF-βs poses challenges for the development of effective therapeutic strategies however. In the normal adult animal, TGF-βs play important roles in maintenance of homeostasis, particularly in the immune system, and in orchestration of the organismal response to injury (6;7). In epithelial carcinogenesis, there is a wealth of clinical and pre-clinical data supporting the hypothesis that TGF-βs generally play a tumor suppressor role in the early stages of the process, and only switch to a tumor promoting role later in disease progression (1;2). Tumor cells and stromal cells are critical targets at both stages. Early in the process, loss of TGF-β response in an initiated epithelial cell can promote the early stages of tumorigenesis through impairment of tumor-cell autonomous suppressor mechanisms, such as growth inhibition, differentiation, apoptosis and maintenance of genomic stability (2). However, loss of TGF-β response in fibroblasts or T-cells can also promote tumorigenesis in overlying epithelia, due at least in part to ectopic secretion of tumor-promoting growth factors and cytokines (8;9). In contrast in the later stages of the carcinogenic process, overexpression of TGF-β can promote tumor progression by enhancing migration, invasion and survival of the tumor cells, and by generating a tumor-promoting stroma, primarily through enhanced angiogenesis and suppression of immune surveillance (1;2). The therapeutic challenge is to selectively ablate the tumor promoting effects of TGF-β while sparing desirable effects on normal homeostasis and tumor suppression.
Despite this complex biology, initial pre-clinical studies showed considerable efficacy of antibody-like TGF-β antagonists in suppressing metastasis, with few of the anticipated toxicities such as increased spontaneous tumorigenesis or autoimmune manifestations (10;11). Anti-TGF-β antibodies also completely inhibited tumor recurrence in a fibrosarcoma model, and reduced metastases in a colon cancer model (12). As a result of these and other studies, a number of TGF-β pathway antagonists are in late pre-clinical or early clinical development for treatment of patients with advanced cancer (13;14). Rational development of these agents will require a detailed understanding of which cell compartments and which biological processes are affected by TGF-β antagonism in vivo. Using the 4T1 transplantable mouse model of metastatic breast cancer (15), here we show that treatment with an anti-TGF-β antibody suppresses metastasis through a combination of effects on multiple interacting cell types. Most of these effects occur locally at the tumor site and cooperate to enhance CD8+ T cell activity. We propose that this locally distributed mechanism of action may underlie the surprising lack of toxicity of this class of TGF-β antagonist (10;16).
Materials and Methods
Cell culture and reagents
The 4T1 cell line was provided by Dr. Fred Miller at the Barbara Ann Karmanos Cancer Institute, Detroit, MI, and cultured as previously described (17). TGF-β1 and TNF-α were purchased from R&D Systems (Minneapolis, MN). Staurosporine was purchased from Sigma-Aldrich. Anti-CD8 monoclonal antibody (clone 2.43 rat IgG2b; American Type Culture Collection TIB210) was generated by Harlan Bioproducts, Madison WI. Anti-asialo GM1 was purchased from Wako (Osaka, Japan). The anti-TGF-β murine monoclonal antibody, 1D11, which neutralizes all three isoforms of TGF-β (18), and an isotype-matched IgG1 monoclonal antibody 13C4, which was raised against Shigella toxin and serves as a control, were provided by Genzyme Corp., (Framingham, MA).
In vivo tumorigenicity and metastasis assay
All animals were maintained according to the National Cancer Institute's Animal Care and Use Committee guidelines, under approved animal study protocols. For the spontaneous metastasis format, 4 × 104 4T1 cells in 40 μl of phosphate-buffered saline were inoculated into the surgically exposed left thoracic mammary fat pad (m.f.p.) of anesthetized 7-week-old female BALB/cANCr mice. After inoculation, the mice were randomized into two treatment groups, with 10-15 animals/group. Anti-TGF-β antibody (1D11) or control antibody (13C4) were administered three times per week i.p at 5mg/Kg., starting one day after cell inoculation. Primary tumors were surgically excised on day 10. Mice were euthanized by carbon dioxide narcosis on day 28. Macroscopic quantitation of metastases was performed by counting the number of nodules on the surface of the inflated lung. For microscopic quantitation of lung metastases, each lobe of the lung was processed for hematoxylin-eosin staining and evaluated by a board-certified veterinary pathologist (MRA). For the experimental metastasis format, 4,500 4T1 cells were injected into the tail-vein of 7-week-old female BALB/c mice. In select experiments, mice were injected i.p. with rat anti-CD8 antibody (clone 2.43; 0.5mg/mouse) or rabbit anti-asialo-GM1 antibody (30 μl/mouse) at day -4, -3, -2, 3, 10 and 17 days relative to the tumor injection to deplete CD8+ or natural killer (NK) cells. Depletion was confirmed to be >90% by FACS analysis of blood samples from the treated mice. Lungs were harvested on day 21 and analyzed as above.
Quantitative reverse-transcription polymerase chain reaction (RTQ-PCR)
The real-time quantitative PCR was performed using the iCycler iQ Real-time PCR Detection System (Bio-Rad) with SYBR green dye (Stratagene, Cedar Creek, TX). First-strand cDNA was prepared from total RNA using a SuperScript III first strand synthesis kit (Invitrogen). The quantitative RT-PCR was done in triplicate. Primer details are given in Supplementary Material.
Transfection of tumor cells
A C-terminally Myc-tagged dominant negative type II TGF-β receptor (‘DNR’), comprising nucleotides 1-656 of the human sequence was ligated into pB vector (a kind gift from Dr. Jan Pinkas at Genzyme), and transfected into 4T1 cells using Lipofectamine 2000 transfection reagent (Invitrogen). Stable transfectants were selected and DNR expression was confirmed by promoter-reporter assay and immunoblotting analysis. To minimize the effect of clonal variation, we pooled populations of transfected clones.
In vitro apoptosis assay
Apoptosis of 4T1 cells in vitro was quantitated using the Cell Death Detection ELISA assay kit (Roche), or by FACS detection using the Annexin V-FITC apoptosis kit (BD Biosciences Pharmingen, San Diego, CA). Briefly, 4T1 cells were treated with or without TGF-β1 (5 ng/ml) for 4 days in DMEM containing 3.5% FBS, and then TNF-α (25 ng/ml) was added to select wells for the final two days prior to harvesting for assessment of apoptosis as above.
Conditioned medium collection, tissue extraction and ELISA Assays
Serum-free conditioned medium was prepared from near confluent cell cultures and assayed for TGF-βs, following acid activation of the medium. TGF-β levels in mammary glands and tumors were determined following acid ethanol extraction as previously described (19). Quantitation of TGF-β1, TGF-β2 and TNFRSF1 was performed by using Quantikine ELISA kits (R&D Systems, Minneapolis MN), while TGF-β3 was quantitated by ELISA as described (19).
Immunocytochemistry and immunofluorescence
Active and total TGF-β in sections from metastasis-bearing lungs were visualized by immunofluorescence on fresh frozen tissue cryosections essentially as described (20). Assessment of proliferation, apoptosis, blood vessel density and T-cell infiltration was done on formalin-fixed paraffin-embedded sections, immunostained with anti-phospho-histone H3 (06-570, Upstate), ApopTag Peroxidase In Situ Apoptosis Kit (Chemicon), anti-CD3 (A0452, Dako) or anti-CD31 (sc1506, Santa Cruz). Images of the entire section were acquired using an Aperio Scanscope (model T3). Individual images were manually adjusted for luminosity to compensate for variable counterstain intensity and image analysis was conducted using Image-Pro Plus v 5.1 (Media Cybernetics). A set of standardized color segmentation, morphological filters and area calibration files, was used to quantitate the number of metastases, the individual metastasis area and the number of positive cells (marker dependent) per metastasis. A minimum of one randomly selected high power field (200x) was assessed for each metastasis within a given lung section. For primary tumors, a minimum of 10 random high power fields were assessed for each tumor. All data were exported into Excel for further analysis.
Immunophenotyping and FACS analysis
Primary tumors or tumor-bearing lungs were excised, minced with scissors to a fine slurry in 15ml/lung digestion buffer (RPMI 1640, 5%FBS, 1mg/ml collagenase, 30μg/ml DNase) and digested at 37°C for 30 min. The suspension was pelleted, resuspended and spun through a discontinuous 40%:70% Percoll gradient to enrich for leukocytes. Single-cell suspensions were stained and analyzed on FACSCalibur (Becton Dickinson, Mountain View, CA) using CellQuest (BD BioSciences) software. For direct staining to determine the phenotype of lymphocyte populations, conjugated antibodies were purchased from BD BioSciences or eBiosciences (San Diego, CA); CD45PerCP, CD4 APC, CD8APC, CD3PerCP, DX-5 APC, NKG2D PE, CD25 PE, CD69 FITC, CD122PE. For determination of Rae-1γ levels on tumor cells, 4T1 cells were harvested after 4 days incubation with or without TGF-β1 (5 ng/ml), then fixed and stained with PE rat anti-mouse Rae-1γ (BD Biosciences Pharmingen, San Diego, CA) and analyzed by flow cytometry.
Statistical analysis
Unpaired parametric Student t test or non-parametric Mann-Whitney U tests were used to analyze the data, unless otherwise indicated in the text.
Results
4T1 cells retain some responsiveness to TGF-β in vitro, and make moderately elevated levels of TGF-β in vivo
Like many aggressive cancer cell lines, 4T1 cells in culture were at best only weakly growth inhibited by TGF-β, but they did respond to TGF-β by phosphorylating Smad2, and inducing Smad-dependent reporter gene expression (Suppl. Fig. 1). 4T1 cells in culture secreted predominantly TGF-β1 (28 ng/106cells/48h), some TGF-β3 (6.9 ng/106cells/48h), and low to no TGF-β2 (<0.4 ng/106cells/48h). In vivo, 4T1 tumors had TGF-β1 protein levels that were ∼3-fold elevated in the primary tumor when compared with the normal mammary gland (220 +/- 24 vs. 79 +/- 16 ng TGF-β1/g wet weight of tissue (n=5), p <0.001). Immunostaining also showed mildly elevated total TGF-β in 4T1 lung metastases when compared with the surrounding lung parenchyma, though without any major increases in the active TGF-β fraction (Suppl. Fig. 2). TGF-β pathway activation within metastases, as assessed by immunostaining for phosphoSmad2, was evident but heterogeneous (Suppl. Fig 2). Finally, in common with some studies on human breast cancers (21;22), we did not see significantly elevated circulating levels of TGF-β in the plasma of tumor-bearing mice when compared with age- and sex-matched normal mice (2.5 +/- 0.8 ng/ml; n=5 vs 1.7 +/- 0.1 ng/ml; n=5, P=NS). Thus the 4T1 model has many of the TGF-β-related properties that we would expect to find in a human breast tumor caught before end stage, and does not have a particularly exaggerated TGF-β production or response.
Suppression of 4T1 cell metastasis by anti-TGF-β antibody treatment is dependent on both the innate and the adaptive arms of the immune system
In the 4T1 model, following orthotopic implantation of tumor into the #2 mammary fat pad, large numbers of small lung metastases were seen (typically 30-80/mouse), while if metastasis was initiated by injection of 4T1 cells into the tail vein, we observed smaller numbers of metastases (6-12/mouse) that were of larger size. However, regardless of experimental format, in multiple independent experiments we found that treatment with the 1D11 anti-TGF-β antibody caused a statistically significant 50-60% reduction in the number of macroscopic and of histologically confirmed lung metastases (Fig 1A,B). Mice treated with the 1D11 antibody were healthier than mice treated with the 13C4 control antibody, as judged by their higher body weight, and they showed less infiltration of tumor cells into the thoracic lymph nodes (Suppl. Fig 3). Histologically, there were no obvious differences between tumors from the two treatment groups (data not shown).
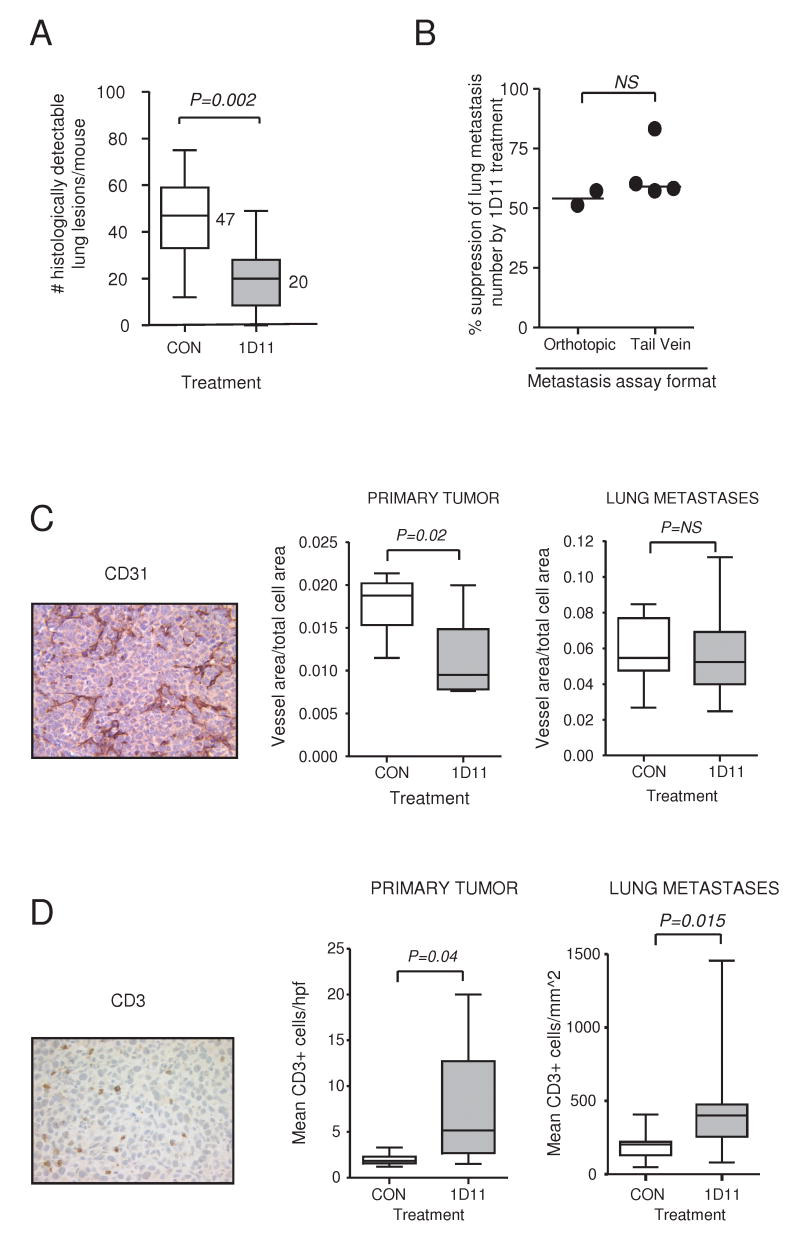
Figure 1. Suppression of lung metastasis by 1D11 in the 4T1 model is associated with increased infitration of T-cells and reduced angiogenesis.
A. Numbers of histologically detectable metastases in the lung. 4T1 cells were implanted orthotopically into the left thoracic mammary fat pad of syngeneic BALB/c mice and mice were randomized to treatment with anti-TGF-β (1D11) or control 13C4 antibody (CON) antibody starting at day 1 after innoculation. Primary tumors were surgically excised at day 10, mice were euthanized on day 28. Boxes, median values with upper and lower quartiles; whiskers, range. (Control group, 11 mice; 1D11 group, 13 mice). B. Comparison of 1D11 efficacy in reducing lung metastasis number using either the orthotopic implantation or the tail vein injection experimental formats. The extent of metastasis suppression for each experiment was determined by comparing the median number of metastases in the 1D11-treated group with that in the control group. Each point represents the results of an independent experiment that contained a minimum of 10 mice/treatment group. Metastasis suppression was statistically significant in each case. C and D. The effect of 1D11 on microvessel density (C: CD31 marker) or on the number of infiltrating T-cells (D: CD3 marker) in the primary tumors and lung metastases from the experiment in (A) was determined by semiautomated analysis of immunohistochemically stained sections as described in Methods. Representative images are shown for each marker. A minimum of 10 randomly selected fields were quantitated for each primary tumor, or the entire area of every metastasis in each set of lung lobe cross-sections was evaluated, to determine the mean marker density for that mouse. For primary tumors, 8 mice were evaluated/group and for metastases, 8-11 mice were evaluated/group. Boxes, median values with upper and lower quartiles; whiskers, range.
Since the tail vein injection format introduces tumor cells directly into the vasculature, the similarity of the results in the two experimental formats suggests that 1D11 acts primarily on a step in the metastasic cascade that lies down-stream of invasion and intravasation. TGF-β has previously been shown to promote the extravasation step in the MMTV-Neu transgenic model of metastatic breast cancer (23). In the 4T1 model, we found that the majority of metastases were extravascular regardless of treatment (85+/-7% in control antibody-treated mice; n=11 vs 90 +/- 11% in 1D11-treated mice; n=12, P = NS), suggesting that if extravasation is a TGF-β-dependent step in this model, it is either not rate-limiting or not accessible to the antibody.
Depending on the model system used, studies with other TGF-β antagonists have implicated effects either on angiogenesis or on immune surveillance as mechanisms that may underlie efficacy (12;24-29). By immunohistochemical approaches, we saw evidence in support of both mechanisms in the 4T1 model. Treatment with 1D11 was associated with a statistically significant decrease in microvessel density in the primary tumor, though not in the lung metastases, and with significantly increased T-cell infiltration at both sites (Fig. 1C,D).
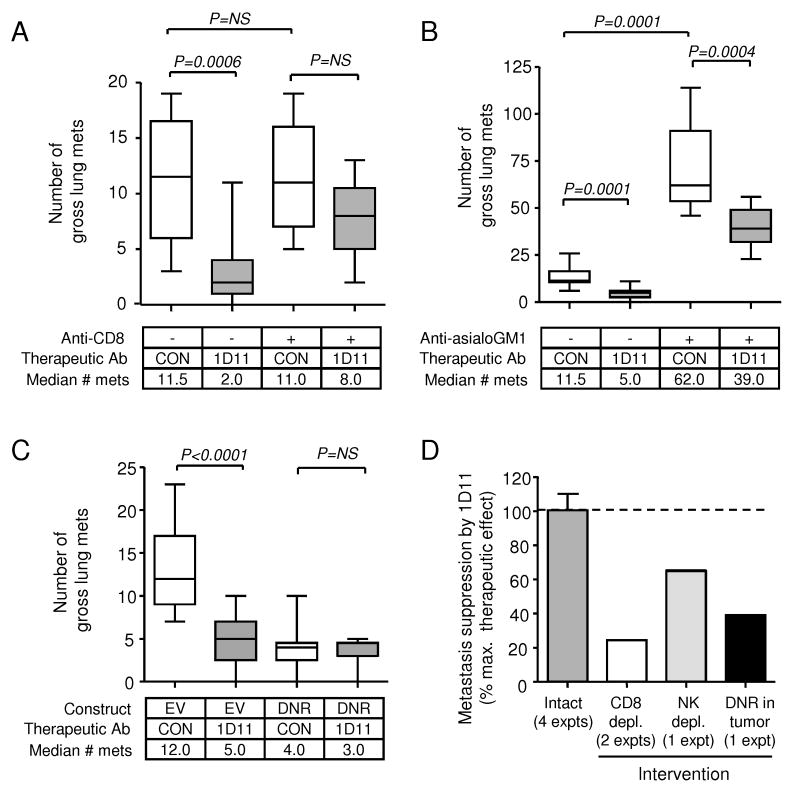
TGF-β has potent suppressive effects on the generation and/or effector function of most immune cells (30). To address the potential role of immune-mediated mechanisms in the current model, we depleted mice of CD8+ cells or NK cells. Depletion of CD8+ cells had no effect on the number of lung metastases in the absence of 1D11 treatment, suggesting that there is no effective T-cell mediated immune surveillance in this model in the untreated state (Fig. 2A, compare columns 1 and 3). In contrast, depletion of NK cells resulted in a dramatic increase in the number of lung metastases (Fig. 2B, compare columns 1 and 3), suggesting that the innate arm of the immune surveillance system is quite active. Most of the efficacy of 1D11 treatment was lost on depletion of CD8+ cells (Fig. 2A; compare columns 1 vs 2 with 3 vs 4), whereas treatment with 1D11 was still capable of suppressing metastasis in the NK-depleted mice, though to a lesser extent than in intact mice (Fig. 2B). Thus 1D11 treatment appears to unmask effective immune surveillance. Interestingly, blockade of TGF-β response in the 4T1 tumor cells using a dominant negative type II TGF-β receptor (DNR) also ablated most of the metastasis suppressing effect of 1D11 (Fig. 2C). Combining data from multiple experiments, we can calculate that ∼75% of the antibody efficacy is dependent on the presence of CD8+ cells, while ∼35% is dependent on the presence of NK cells, and ∼60% requires an intact TGF-β response in the tumor cell itself (Fig. 2D). Since the sum of these effects is >100%, the data suggest that treatment with 1D11 enhances anti-tumor immune responses by a cooperative mechanism that involves several cellular compartments, including the CD8+ T cells, NK cells and the tumor itself.
Figure 2. Maximum efficacy of 1D11 in suppressing metastasis is dependent on the presence of CD8+ cells, NK cells and an intact TGF-β response in the tumor cell.
4T1 cells were injected into the tail-vein of BALB/c mice, and mice were treated with 1D11 or CON antibody with dosing and scheduling as in Fig. 1. Mice were euthanized on day 21 and the number of grossly visible metastases/lung was determined. All experimental groups had 10-13 mice/group. Boxes, median values with upper and lower quartiles; whiskers, range. A. Effect of CD8 cell depletion. Where indicated, mice were treated with anti-CD8 antibody, prior to the injection of tumor cells, to deplete CD8+ cells. One experiment representative of two replicates is shown. B. Effect of NK cell depletion. Where indicated, mice were treated with anti-asialoGM1, prior to injection of tumor cells, to deplete NK cells. C. Effect of loss of TGF-β response in the tumor cell. 4T1 cells were transfected with either an empty vector (EV) or with a dominant negative type II TGF-β receptor (DNR) and pooled transfectants were used for the metastasis assay. D. Summary of the efficacy of 1D11 in suppressing metastasis following the interventions above. The extent of suppression of lung metastases by 1D11 was first determined by comparing median numbers of lung metastases in mice treated with 1D11 and CON for each of the individual interventions. The efficacy of 1D11 following each experimental intervention was then expressed as a % of the maximum therapeutic effect seen in the unmanipulated (“intact”) system. Results are the mean +/- SD for the indicated number of replicate experiments.
Effects of anti-TGF-β antibody treatment on immune cell number and function are only seen locally at the primary tumor or metastatic site
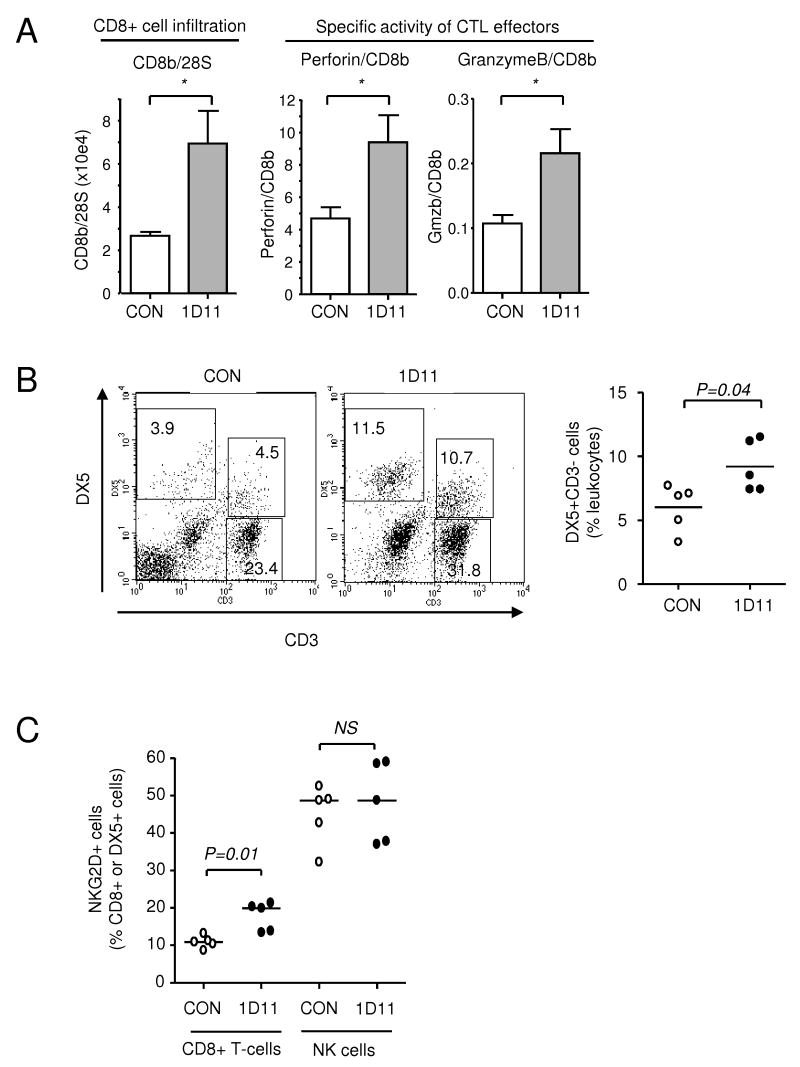
Enhanced immune surveillance is frequently associated with increased numbers of tumor-specific cytotoxic T-cells (CTLs) in the spleen. However, we were unable to demonstrate any increase in splenic CTL activity against 4T1 cells following treatment of the mice with 1D11 in repeated experiments, using multiple different experimental formats (data not shown). In addition, there were no significant effects of 1D11 treatment on relative numbers or activation status of immune cells in the spleen (data not shown). In respect to the lack of splenic CTL activity, our results differed from those of others, using different antagonists in this and other models (27-29). We reasoned that 1D11 might be primarily affecting immune cell infiltration and function specifically at the primary tumor or metastatic sites. We were unable to recover sufficient viable immune cells from the primary tumor for functional analysis. However, by RTQ-PCR of tumor-derived RNA, we showed that 1D11 treatment was associated with a two-fold increase in CD8b mRNA, consistent with an increased infiltration of the tumor by CD8+ T-cells. Furthermore, the ratio of perforin/CD8b and granzyme B/CD8b mRNAs in the primary tumor was also increased ∼ 2-fold, consistent with enhanced expression of cytotoxic effector molecules in the infiltrating CD8+ cells (Figure 3A). These data are consistent with localized increases in cytotoxic T-cell number and activity at the primary tumor site.
Figure 3. Effect of 1D11 treatment on numbers of immune cells and markers of activity.
A. RTQ-PCR analysis of mRNA levels of CD8b, and of the cytotoxic T-cell effectors, perforin and granzyme B from primary tumors treated with anti-TGF-β (1D11) or control (CON) antibody. Results are the mean +/- SD for 5 tumors/treatment group. P<0.05. B and C. FACS analysis of immune cells recovered from tumor-bearing lungs of mice injected orthotopically with 4T1 cells and treated with anti-TGF-β (1D11) or control (CON) antibody. Lungs were harvested at day 28, digested with collagenase, enriched for viable cells using a Percoll gradient, and then immune cells were analyzed for expression of specific markers by FACS. B. Representative FACS plot for determination of the effect of antibody treatment on the representation of T-cells (CD3+) or NK cells (CD3-DX5+) in the leukocyte gate by dual immunostaining. The scatter plot shows the % NK cells in the leukocyte gate for 5 mice/treatment group. Median values are indicated. C. The % of cells expressing the activator/coactivator NKG2D was determined individually for the CD8+ and the DX5+ (NK) cell populations for 5 mice/group. Median values are indicated.
To address the nature and activation status of immune cells at the metastatic site, we prepared cell suspensions from the lungs of tumor-bearing mice treated with 1D11 or control antibody 13C4, and analyzed the infiltrating immune cells by FACS. We found no statistically significant differences in the percentage of B cells (CD19+) or myeloid cells (Gr-1+ and CD11b+) in the leukocyte gate, and no change in the ratio of CD4+ to CD8+ T-cells (CD3+ gate). However, there was a significant increase in the percentage of NK cells (CD3-DX5+) in 1D11-treated lungs (Fig. 3B). We also examined expression of a number of markers associated with immune cell activation or function. While there was no increase in the CD4+CD25+ fraction that includes the FoxP3+ regulatory T-cells (Suppl. Fig 4) and no change in expression of CD25 or CD69 early activation markers in either CD4+ or CD8+ T-cell subsets (data not shown), there was a mild but significant increase in the fraction of CD8+ cells expressing CD122 (IL-2/IL-15Rβ) in the lungs, and a trend towards increased expression of TRAIL in the CD8+ compartment (Suppl. Fig 4). NKG2D, which is an activating receptor on NK cells and a coactivator on CD8+ T-cells, has previously been shown to be downregulated on NK cells in patients whose tumors overexpress TGF-β (31). We found that 1D11 treatment significantly increased NKG2D expression in the CD8+ T-cell compartment, while having no effect on NKG2D expression on NK cells where it was already high (Fig. 3C).
TGF-β antagonism increases tumor cell susceptibility to recognition and killing by the immune system
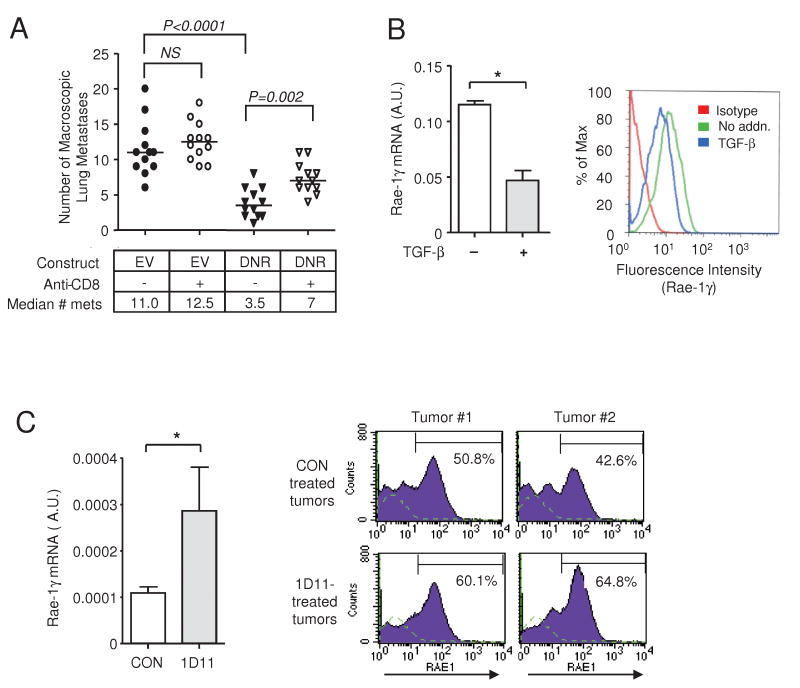
Since effects of 1D11 treatment on the immune cell compartment were relatively mild and seemed unlikely alone to account for the therapeutic efficacy, we next asked whether 1D11 might affect the tumor cell itself in such a way as to further enhance immune surveillance. Blocking the response to TGF-β specifically in the tumor cell compartment using a dominant negative TGF-β receptor (DNR) caused a decrease in metastatic efficiency (Fig. 4A, compare columns 1 and 3), suggesting that endogenous TGF-β acts on the tumor cell to promote metastasis. Part of this suppressive effect was lost if the mice were depleted of CD8+ T-cells (Fig. 4A, compare columns 3 and 4), suggesting that a direct effect of TGF-β on the tumor cell itself must contribute to the evasion of effective immune surveillance.
Figure 4. Efficacy of 1D11 involves effects on the tumor cell as well as the immune compartment.
A. Effect of TGF-β blockade on metastatic efficiency in the presence or absence of CD8+ cells. TGF-β response was blockaded specifically in the tumor cell by transfection with a dominant negative type II receptor (DNR) or empty vector control (EV). The number of lung metastases was determined using the tail vein injection protocol, with or without pre-treatment of the mice with anti-CD8 antibody to deplete CD8+ cells (12 mice/group). The horizontal line indicates the median number of metastases. B. RTQ-PCR and FACS analysis of Rae-1γ expression in 4T1 cells after 4 days of treatment with TGF-β (5ng/ml). Rae-1γ mRNA was normalized to 28SrRNA, and results are the mean +/- SD (n=3). C. RTQ-PCR and FACS analysis of Rae-1γ expression in primary tumors derived from mice treated with anti-TGF-β (1D11) or control antibody (CON). RTQ-PCR results are the mean +/- SD for 5 tumors/group and Rae-1γ mRNA expression was normalized to 28s rRNA. FACS results for two representative tumors in each treatment group are shown. *P<0.001; Students T-test.
TGF-β has been shown to down-regulate expression of major histocompatibility complex components in other systems (32), which should render the tumor cell less visible to the immune system. However, we did not find a significant effect of TGF-β or 1D11 on basal or IFN-γ-induced expression of the MHC class I component H2Kd in vitro or in vivo as assessed by RTQ-PCR and FACS analysis (data not shown) in the 4T1 model. Since we had shown that 1D11 treatment upregulates expression of the co-activating receptor NKG2D on CD8+ T cells, we looked for effects of 1D11 on the expression of Rae-1γ, the cognate NKG2D ligand, on the tumor cells. Rae-1γ is a stress-induced molecule that alerts the immune system to the presence of an incipient tumor (33). TGF-β treatment significantly down-regulated Rae-1γ mRNA and protein in 4T1 cells in vitro (Fig. 4B), and conversely, 1D11 treatment upregulated Rae-1γ mRNA in 4T1 primary tumors in vivo (Fig. 4C). Rae-1γ expression was also enhanced on the surface of tumor cells recovered from 1D11-treated mice as determined by FACS analysis (Fig. 4C). This increased expression of an NKG2D ligand on the tumor would be expected to enhance immune cell activation, particularly in the context of upregulated NKG2D expression on the immune cells. Indeed, such an effect has been shown in a glioma model system using antisense strategies for TGF-β blockade (34).
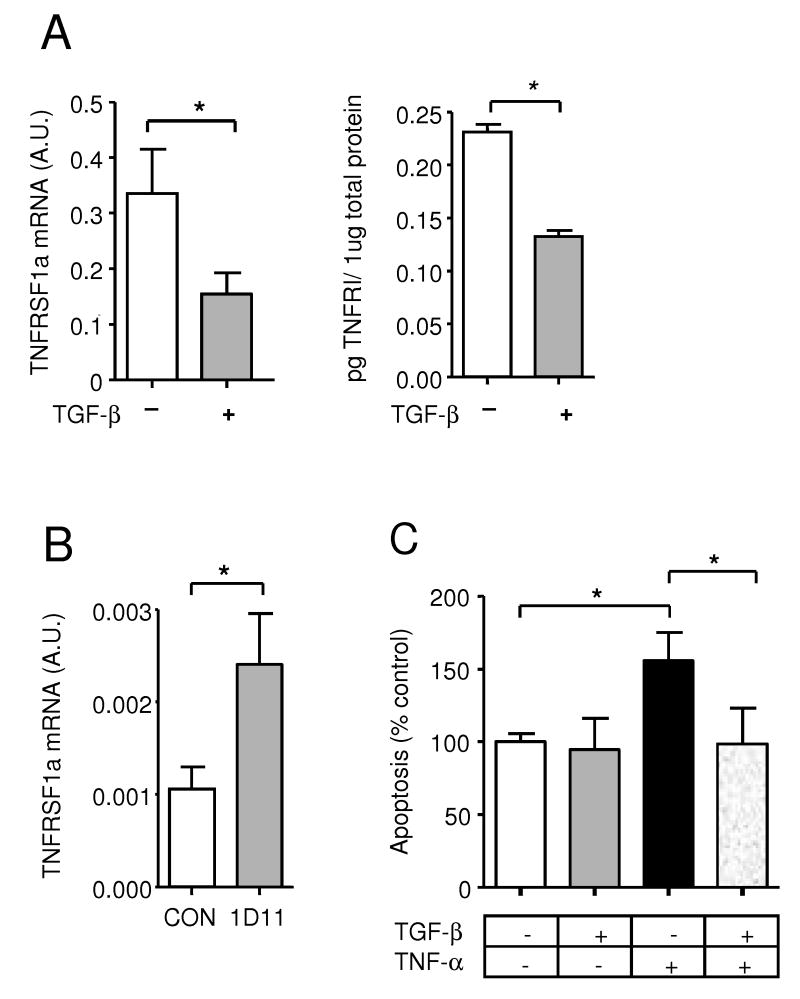
TGF-β has complex effects on cell survival, acting either as a pro-apoptotic factor or as a pro-survival factor, depending on the cell type and biological context (35). TGF-β treatment had no effect on survival of 4T1 cells in response to serum deprivation (data not shown), suggesting that there was no generalized pro-survival effect of TGF-β on the intrinsic cell death pathway and downstream apoptotic machinery in this cell type. However, immune cells kill in part by activation of death receptors on the target cell, so we next looked for effects on the extrinsic death pathway. Expression of Fas and Fas ligand on 4T1 tumor cells was unaffected by TGF-β in vitro or 1D11 in vivo (data not shown). However, we found that TGF-β treatment significantly down-regulated expression of the TNF-α death receptor, TNFRSF1a, on 4T1 cells in vitro at the mRNA and protein level (Fig. 5A) Conversely, 1D11 treatment upregulated TNFRSF1a mRNA in 4T1 tumors in vivo (Fig. 5B). Down-regulation of TNFRSR1a by TGF-β in vitro was associated with enhanced resistance to cell killing by TNF-α (Fig. 5C), consistent with the possibility that 1D11 treatment makes tumor cells more susceptible to death receptor-mediated cell killing in vivo. The inhibitory effect of TGF-β on expression of both TNFRSF1a and Rae-1γ was not restricted to the 4T1 line but was also seen in EMT6 (mouse), MDA MB231 (human) and Hs578T (human) breast cancer cell lines (Suppl. Fig 5).
Figure 5. Effect of TGF-β on TNF-α receptor expression and sensitivity of 4T1 cells to induction of apoptosis by TNF-α.
A. Expression of TNF-α receptor 1 (TNFRSF1a) mRNA and protein in 4T1 cells were treated for 2 days in vitro with 5ng/ml TGF-β or vehicle control. TNFRSF1a mRNA was determined by RTQ-PCR, and the level of TNFR1 protein in 4T1 cell lysates was detected by ELISA assay. Results are the mean +/- SD for 3 determinations. B. RTQ-PCR analysis of TNFRSF1a expression in 4T1 primary tumors following 9 days of treatment in vivo with anti-TGF-β (1D11) or control (CON) antibody. TNFRSF1a expression was normalized to the 28S rRNA in each case. Results are mean +/- SD for 5 tumors/treatment group. C. In vitro apoptosis assay in 4T1 cells after treatment with TGF-β (5ng/ml) or vehicle control for 4 days, with TNF-α (25ng/ml) also present for the final two days. Results are normalized to the no TGF-β, no TNF-α control conditions, and are the mean +/- SD of 3 determinations. * indicates P<0.001, Student's T-test.
Discussion
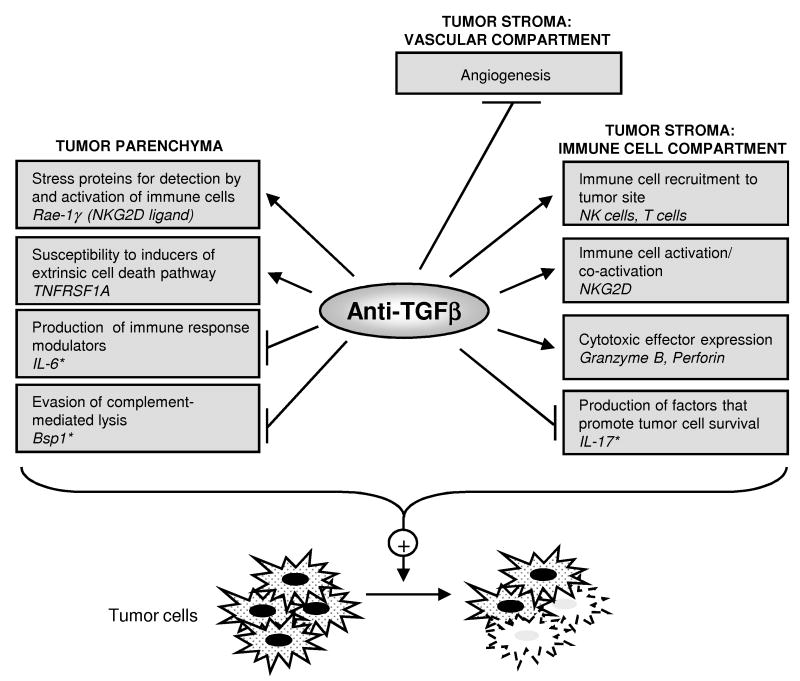
Most pre-clinical studies using TGF-β antagonists to suppress tumor progression have found surprisingly little toxicity (13;14), so it is of considerable interest to understand how such agents can selectively antagonize the undesirable effects of TGF-β on tumor progression. Our data in the 4T1 breast cancer model suggest that anti-TGF-β antibody therapy reduces the number of lung metastases primarily through the integration of many biological effects on multiple cellular compartments. Quantitatively the most important outcome of these effects is the unmasking of effective CD8+ T cell activity against the tumor. Local recruitment and/or activation of cells of both the innate and adaptive arms of the immune system were increased by 1D11 treatment, and tumor cell visibility to the immune system and susceptibility to cell killing were also enhanced. Additionally, angiogenesis was mildly suppressed in the treated tumors, as has also been observed with small molecule receptor kinase antagonists (27). Since the effects of the anti-TGF-β antibody are distributed over multiple cellular compartments and molecular effectors, we refer to this therapeutic mechanism as “death by a thousand cuts” (see model in Fig. 6). The distributed aspect of this mechanism may be critical for a good therapeutic index, and has a number of important implications as discussed below.
Figure 6. Model for the multiple effects of anti-TGF-β antibody on different cellular compartments within the tumor.
Antagonism of TGF-β by anti-TGF-β antibody treatment in the 4T1 breast cancer model has many small magnitude effects locally on the tumor parenchyma and stromal compartments. Most of these effects cooperate to enhance effective anti-tumor immune responses, and aggregately they result in a reduction in metastatic burden (“death by a thousand cuts”). Some effects lead to synergy between different cellular compartments, such as the upregulation of Rae-γ, an NKG2D ligand, on the tumor cell and enhanced expression of NKG2D on CD8+ T-cells. *The effects of 1D11 on Bsp1, IL-6 and IL-17 expression in this model are been described elsewhere ((17) and accompanying manuscript)
The overall importance of immune mechanisms to the therapeutic efficacy of TGF-β antagonists is highlighted by a number of recent studies (12;26-29;36;37). However, the relative contributions of the different immune compartments to the therapeutic efficacy of TGF-β antagonism appear to vary from tumor to tumor. For example, in the 4T1 model, we found that anti-TGF-β treatment primarily activated CD8-mediated anti-tumor immunity, showing only a relatively small enhancement of NK activity. However in a syngeneic rat glioma model, the therapeutic efficacy of TGF-β antagonism using a soluble TGF-β receptor showed a much greater dependency on NK cells (37), and nude mice, which have higher than normal levels of NK cells, may show a particularly exaggerated contribution from the innate arm (25). Similarly, in models of renal and prostate cancer the 1D11 antibody was recently shown to decrease the number of FoxP3+ regulatory T-cells in lung metastases (38), but there was no evidence for 1D11-induced down-regulation of FoxP3+ tumor infiltrating lymphocytes in the 4T1 breast model (Xin Chen, personal communication). Regardless of the details of the immune mechanism however, it is clear that full efficacy of TGF-β antagonists will not be seen in conventional xenograft models using immunodeficient hosts.
TGF-βs have long been known to have potent suppressive effects on the immune system (7). However, integrating our data with published studies, it is clear that the extent or the nature of TGF-β antagonism can dramatically affect the immunological outcome. Near total blockade of TGF-β response specifically in T-cells caused increased resistance to tumorigenesis and metastasis, associated with robust anti-tumor immune responses (39-42). However, this approach also results in the development of widespread autoimmune manifestations (43), such as are seen in the TGF-β1 null mouse (44), suggesting that such profound TGF-β blockade in the T-cell compartment may not be desirable. In contrast, the enhanced anti-tumor immunity that we saw in the current study appeared to be the local result of synergism between many smaller magnitude effects of anti-TGF-β antibodies on multiple cellular compartments, including the tumor cells themselves, and treatment was not associated with a generalized immune activation. Unlike investigators who have used small molecule TGF-β receptor kinase inhibitors (26;27;29), we did not detect increases in anti-tumor CTL activity or in activation status of splenocytes from mice treated with 1D11. Since one such study also used the 4T1 model (27), the data suggest there may be differences in the mode of action of these two types of agent, possibly reflecting a more extensive TGF-β blockade with the kinase inhibitors.
While the locally distributed mode of action of anti-TGF-β antibodies in the vicinity of the tumor may be critical to their lack of immunotoxicity, it also poses practical problems. The development of useful biomarkers of effective TGF-β antagonism in vivo by this class of agent may be difficult, since there is no major change in any one molecular marker in a readily accessible cell compartment. Furthermore, although the general principle of distributed action is likely to be broadly applicable, the specific cellular target and detailed nature of the molecular changes may vary between tumor types. For example, tumor-derived TGF-β was implicated in the down-regulation of NKG2D expression on NK cells in colon cancer and glioblastoma patients (31;34). In contrast, in the 4T1 model we found that NKG2D expression on NK cells at the metastatic site was unaffected by 1D11 treatment, while expression of NKG2D on CD8+ T-cells was significantly enhanced. TGF-β antibodies may therefore represent a class of therapeutics for which a very broad net will have to be cast to capture a constellation of potential biomarkers on several different cell types, only a fraction of which may be affected in any given patient. Emerging technologies for efficient assay multiplexing will be useful in this regard.
In the present work, we have focused on mechanisms underlying the effect of anti-TGF-β treatment on metastasis number. In a companion study, we show that anti-TGF-β treatment decreases the size of lung metastases by a distinct immune-mediated mechanism, in which anti-TGF-β suppresses the ability of the tumor to subvert CD8+ T cells into making IL-17, a tumor cell survival factor (Nam et al, submitted). Both effects of anti-TGF-β combine to reduce overall metastatic efficiency. It is of interest that TGF-β antibodies were as efficacious as the conventional chemotherapeutic paclitaxel in suppressing metastasis in the 4T1 model (45), despite the fact that this model does not show a particularly high level of TGF-β production or activation in the tumor or circulation. The data suggest that even patients with relatively low level TGF-β expression in their tumors may have compromised anti-tumor immune responses that could be at least partially restored by TGF-β antagonism. Combining TGF-β antagonists with other therapeutic approaches, such as nano-micellar drug delivery (46), is likely to give further benefit.
The TGF-βs appeared relatively late in evolution at a time when organismal complexity was considerably increased (47). Since essentially every cell type in the body can respond to TGF-β in some way, TGF-βs may play particularly important roles in higher order functional integration between different cellular compartments. Tonic, low level TGF-β signaling between organ parenchyma and stroma is clearly important for maintenance of homeostasis in normal tissues, as local inactivation of TGF-β pathway components in fibroblasts or immune cells results in the generation of a pro-carcinogenic microenvironment (8;9). However local overexpression of TGF-β, as is seen in many advanced human tumors, also generates a tumor promoting microenvironment, albeit of a different form (1;2). Thus this regulatory system appears to be very delicately poised. We propose that the main effect of anti-TGF-β antibody treatment is to normalize the distortions in this complex intercellular communication network that are caused by tumor-induced overexpression of TGF-β, thereby restoring the microenvironment to a more tumor suppressive state.
Supplementary Material
Reference List
- 1.Pardali K, Moustakas A. Actions of TGF-β as tumor suppressor and pro-metastatic factor in human cancer. Biochim Biophys Acta. 2007;1775:21–62. doi: 10.1016/j.bbcan.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Derynck R, Akhurst RJ, Balmain A. TGF-β signaling in tumor suppression and cancer progression. Nat Genet. 2001;29:117–29. doi: 10.1038/ng1001-117. [DOI] [PubMed] [Google Scholar]
- 3.Gold LI. The role for transforming growth factor-β (TGF-β) in human cancer. Crit Rev Oncog. 1999;10:303–60. [PubMed] [Google Scholar]
- 4.Teicher BA. Transforming Growth Factor-β and the Immune Response to Malignant Disease. Clin Cancer Res. 2007;13:6247–51. doi: 10.1158/1078-0432.CCR-07-1654. [DOI] [PubMed] [Google Scholar]
- 5.Bierie B, Moses HL. Tumour microenvironment: TGFβ: the molecular Jekyll and Hyde of cancer. Nat Rev Cancer. 2006;6:506–20. doi: 10.1038/nrc1926. [DOI] [PubMed] [Google Scholar]
- 6.Roberts AB, Tian F, Byfield SD, et al. Smad3 is key to TGF-β-mediated epithelial-to-mesenchymal transition, fibrosis, tumor suppression and metastasis. Cytokine Growth Factor Rev. 2006;17:19–27. doi: 10.1016/j.cytogfr.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 7.Li MO, Wan YY, Sanjabi S, Robertson AK, Flavell RA. Transforming growth factor-β regulation of immune responses. Annu Rev Immunol. 2006;24:99–146. doi: 10.1146/annurev.immunol.24.021605.090737. [DOI] [PubMed] [Google Scholar]
- 8.Bhowmick NA, Chytil A, Plieth D, et al. TGF-β signaling in fibroblasts modulates the oncogenic potential of adjacent epithelia. Science. 2004;303:848–51. doi: 10.1126/science.1090922. [DOI] [PubMed] [Google Scholar]
- 9.Kim BG, Li C, Qiao W, Mamura M, et al. Smad4 signalling in T cells is required for suppression of gastrointestinal cancer. Nature. 2006;441:1015–9. doi: 10.1038/nature04846. [DOI] [PubMed] [Google Scholar]
- 10.Yang YA, Dukhanina O, Tang B, et al. Lifetime exposure to a soluble TGF-β antagonist protects mice against metastasis without adverse side effects. J Clin Invest. 2002;109:1607–15. doi: 10.1172/JCI15333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muraoka RS, Dumont N, Ritter CA, et al. Blockade of TGF-β inhibits mammary tumor cell viability, migration, and metastases. J Clin Invest. 2002;109:1551–9. doi: 10.1172/JCI15234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terabe M, Matsui S, Park JM, et al. Transforming growth factor-β production and myeloid cells are an effector mechanism through which CD1d-restricted T cells block cytotoxic T lymphocyte-mediated tumor immunosurveillance: abrogation prevents tumor recurrence. J Exp Med. 2003;198:1741–52. doi: 10.1084/jem.20022227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saunier EF, Akhurst RJ. TGF β inhibition for cancer therapy. Curr Cancer Drug Targets. 2006;6:565–78. doi: 10.2174/156800906778742460. [DOI] [PubMed] [Google Scholar]
- 14.Yingling JM, Blanchard KL, Sawyer JS. Development of TGF-β signalling inhibitors for cancer therapy. Nat Rev Drug Discov. 2004;3:1011–22. doi: 10.1038/nrd1580. [DOI] [PubMed] [Google Scholar]
- 15.Aslakson CJ, Miller FR. Selective events in the metastatic process defined by analysis of the sequential dissemination of subpopulations of a mouse mammary tumor. Cancer Res. 1992;52:1399–405. [PubMed] [Google Scholar]
- 16.Ruzek MC, Hawes M, Pratt B, et al. Minimal effects on immune parameters following chronic anti-TGF-β monoclonal antibody administration to normal mice. Immunopharmacol Immunotoxicol. 2003;25:235–57. doi: 10.1081/iph-120020473. [DOI] [PubMed] [Google Scholar]
- 17.Nam JS, Suchar AM, Kang MJ, et al. Bone sialoprotein mediates the tumor cell-targeted prometastatic activity of transforming growth factor β in a mouse model of breast cancer. Cancer Res. 2006;66:6327–35. doi: 10.1158/0008-5472.CAN-06-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dasch JR, Pace DR, Waegell W, Inenaga D, Ellingsworth L. Monoclonal antibodies recognizing transforming growth factor-β. Bioactivity neutralization and transforming growth factor β2 affinity purification. J Immunol. 1989;142:1536–41. [PubMed] [Google Scholar]
- 19.Danielpour D, Roberts AB. Specific and sensitive quantitation of transforming growth factor β3 by sandwich enzyme-linked immunosorbent assay. J Immunol Methods. 1995;180:265–72. doi: 10.1016/0022-1759(94)00322-n. [DOI] [PubMed] [Google Scholar]
- 20.Ehrhart EJ, Segarini P, Tsang ML, Carroll AG, Barcellos-Hoff MH. Latent transforming growth factor β1 activation in situ: quantitative and functional evidence after low-dose gamma-irradiation. FASEB J. 1997;11:991–1002. doi: 10.1096/fasebj.11.12.9337152. [DOI] [PubMed] [Google Scholar]
- 21.Wakefield LM, Letterio JJ, Chen T, et al. Transforming growth factor-β1 circulates in normal human plasma and is unchanged in advanced metastatic breast cancer. Clin Cancer Res. 1995;1:129–36. [PubMed] [Google Scholar]
- 22.Sminia P, Barten AD, van Waarde MA, Vujaskovic Z, van Tienhoven G. Plasma transforming growth factor β levels in breast cancer patients. Oncol Rep. 1998;5:485–8. doi: 10.3892/or.5.2.485. [DOI] [PubMed] [Google Scholar]
- 23.Siegel PM, Shu W, Cardiff RD, Muller WJ, Massague J. Transforming growth factor β signaling impairs Neu-induced mammary tumorigenesis while promoting pulmonary metastasis. Proc Natl Acad Sci U S A. 2003;100:8430–5. doi: 10.1073/pnas.0932636100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bandyopadhyay A, Lopez-Casillas F, Malik SN, et al. Antitumor activity of a recombinant soluble β–glycan in human breast cancer xenograft. Cancer Res. 2002;62:4690–5. [PubMed] [Google Scholar]
- 25.Arteaga CL, Hurd SD, Winnier AR, Johnson MD, Fendly BM, Forbes JT. Anti-transforming growth factor (TGF)-β antibodies inhibit breast cancer cell tumorigenicity and increase mouse spleen natural killer cell activity. Implications for a possible role of tumor cell/host TGF-β interactions in human breast cancer progression. J Clin Invest. 1993;92:2569–76. doi: 10.1172/JCI116871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uhl M, Aulwurm S, Wischhusen J, et al. SD-208, a novel transforming growth factor β receptor I kinase inhibitor, inhibits growth and invasiveness and enhances immunogenicity of murine and human glioma cells in vitro and in vivo. Cancer Res. 2004;64:7954–61. doi: 10.1158/0008-5472.CAN-04-1013. [DOI] [PubMed] [Google Scholar]
- 27.Ge R, Rajeev V, Ray P, et al. Inhibition of growth and metastasis of mouse mammary carcinoma by selective inhibitor of transforming growth factor-β type I receptor kinase in vivo. Clin Cancer Res. 2006;12:4315–30. doi: 10.1158/1078-0432.CCR-06-0162. [DOI] [PubMed] [Google Scholar]
- 28.Suzuki E, Kapoor V, Cheung HK, et al. Soluble type II transforming growth factor-β receptor inhibits established murine malignant mesothelioma tumor growth by augmenting host antitumor immunity. Clin Cancer Res. 2004;10:5907–18. doi: 10.1158/1078-0432.CCR-03-0611. [DOI] [PubMed] [Google Scholar]
- 29.Suzuki E, Kim S, Cheung HK, et al. A novel small-molecule inhibitor of transforming growth factor β type I receptor kinase (SM16) inhibits murine mesothelioma tumor growth in vivo and prevents tumor recurrence after surgical resection. Cancer Res. 2007;67:2351–9. doi: 10.1158/0008-5472.CAN-06-2389. [DOI] [PubMed] [Google Scholar]
- 30.Wrzesinski SH, Wan YY, Flavell RA. Transforming Growth Factor-β and the Immune Response: Implications for Anticancer Therapy. Clin Cancer Res. 2007;13:5262–70. doi: 10.1158/1078-0432.CCR-07-1157. [DOI] [PubMed] [Google Scholar]
- 31.Lee JC, Lee KM, Kim DW, Heo DS. Elevated TGF-β1 secretion and down-modulation of NKG2D underlies impaired NK cytotoxicity in cancer patients. J Immunol. 2004;172:7335–40. doi: 10.4049/jimmunol.172.12.7335. [DOI] [PubMed] [Google Scholar]
- 32.Geiser AG, Letterio JJ, Kulkarni AB, Karlsson S, Roberts AB, Sporn MB. Transforming growth factor β 1 (TGF-β 1) controls expression of major histocompatibility genes in the postnatal mouse: aberrant histocompatibility antigen expression in the pathogenesis of the TGF-β 1 null mouse phenotype. Proc Natl Acad Sci U S A. 1993;90:9944–8. doi: 10.1073/pnas.90.21.9944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Raulet DH. Roles of the NKG2D immunoreceptor and its ligands. Nat Rev Immunol. 2003;3:781–90. doi: 10.1038/nri1199. [DOI] [PubMed] [Google Scholar]
- 34.Friese MA, Wischhusen J, Wick W, et al. RNA interference targeting transforming growth factor-β enhances NKG2D-mediated antiglioma immune response, inhibits glioma cell migration and invasiveness, and abrogates tumorigenicity in vivo. Cancer Res. 2004;64:7596–603. doi: 10.1158/0008-5472.CAN-04-1627. [DOI] [PubMed] [Google Scholar]
- 35.Sanchez-Capelo A. Dual role for TGF-β1 in apoptosis. Cytokine Growth Factor Rev. 2005;16:15–34. doi: 10.1016/j.cytogfr.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 36.Won J, Kim H, Park EJ, Hong Y, Kim SJ, Yun Y. Tumorigenicity of mouse thymoma is suppressed by soluble type II transforming growth factor β receptor therapy. Cancer Res. 1999;59:1273–7. [PubMed] [Google Scholar]
- 37.Witham TF, Villa L, Yang T, et al. Expression of a soluble transforming growth factor-β (TGFβ) receptor reduces tumorigenicity by regulating natural killer (NK) cell activity against 9L gliosarcoma in vivo. J Neurooncol. 2003;64:63–9. doi: 10.1007/BF02700021. [DOI] [PubMed] [Google Scholar]
- 38.Liu VC, Wong LY, Jang T, et al. Tumor evasion of the immune system by converting CD4+CD25- T cells into CD4+CD25+ T regulatory cells: role of tumor-derived TGF-β. J Immunol. 2007;178:2883–92. doi: 10.4049/jimmunol.178.5.2883. [DOI] [PubMed] [Google Scholar]
- 39.Gorelik L, Flavell RA. Immune-mediated eradication of tumors through the blockade of transforming growth factor-β signaling in T cells. Nat Med. 2001;7:1118–22. doi: 10.1038/nm1001-1118. [DOI] [PubMed] [Google Scholar]
- 40.Zhang Q, Yang X, Pins M, et al. Adoptive transfer of tumor-reactive transforming growth factor-β-insensitive CD8+ T cells: eradication of autologous mouse prostate cancer. Cancer Res. 2005;65:1761–9. doi: 10.1158/0008-5472.CAN-04-3169. [DOI] [PubMed] [Google Scholar]
- 41.Shah AH, Tabayoyong WB, Kimm SY, Kim SJ, Van Parijs L, Lee C. Reconstitution of lethally irradiated adult mice with dominant negative TGF-β type II receptor-transduced bone marrow leads to myeloid expansion and inflammatory disease. J Immunol. 2002;169:3485–91. doi: 10.4049/jimmunol.169.7.3485. [DOI] [PubMed] [Google Scholar]
- 42.Zhang Q, Yang XJ, Kundu SD, et al. Blockade of transforming growth factor-β signaling in tumor-reactive CD8(+) T cells activates the antitumor immune response cycle. Mol Cancer Ther. 2006;5:1733–43. doi: 10.1158/1535-7163.MCT-06-0109. [DOI] [PubMed] [Google Scholar]
- 43.Gorelik L, Flavell RA. Abrogation of TGFβ signaling in T cells leads to spontaneous T cell differentiation and autoimmune disease. Immunity. 2000;12:171–81. doi: 10.1016/s1074-7613(00)80170-3. [DOI] [PubMed] [Google Scholar]
- 44.Kulkarni AB, Huh CG, Becker D, et al. Transforming growth factor β1 null mutation in mice causes excessive inflammatory response and early death. Proc Natl Acad Sci U S A. 1993;90:770–4. doi: 10.1073/pnas.90.2.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li J, Dong X, Xu Z, Jiang X, Jiang H, Krissansen GW, et al. Endostatin gene therapy enhances the efficacy of paclitaxel to suppress breast cancers and metastases in mice. J Biomed Sci. 2008;15:99–105. doi: 10.1007/s11373-007-9201-3. [DOI] [PubMed] [Google Scholar]
- 46.Kano MR, Bae Y, Iwata C, et al. Improvement of cancer-targeting therapy, using nanocarriers for intractable solid tumors by inhibition of TGF-β signaling. Proc Natl Acad Sci U S A. 2007;104:3460–5. doi: 10.1073/pnas.0611660104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Putnam NH, Srivastava M, Hellsten U, et al. Sea anemone genome reveals ancestral eumetazoan gene repertoire and genomic organization. Science. 2007;317:86–94. doi: 10.1126/science.1139158. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.