Abstract
Background
High blood pressure in middle age is a well-established risk factor for cardiovascular disease, but the consequences of low-level elevations during young adulthood are unknown.
Objective
To measure the association between prehypertension exposure before age 35 and coronary calcium later in life
Design
Prospective cohort study
Setting
Four U.S. communities
Participants
Black and white men and women recruited at age 18–30 for the Coronary Artery Risk Development in Young Adults (CARDIA) Study in 1985–6, and without hypertension before age 35
Measurements
We estimated blood pressure trajectories for each participant using measurements from 7 examinations over the course of 20 years. Cumulative exposure to blood pressure in the prehypertension range (systolic 120–139 and/or diastolic 80–89 mmHg) from age 20–35 was calculated in units of “mmHg-years” (similar to “pack-years” of tobacco exposure) and related to presence of coronary calcium measured at each participant’s last examination (age 44±4).
Results
Among 3560 participants, the 635 (18%) who developed prehypertension before age 35 were more often black, male, overweight and of lower socioeconomic status. Exposure to prehypertension before age 35, especially systolic prehypertension, showed a graded association with coronary calcium later in life (coronary calcium prevalence 15%, 24% and 38% for 0, 1–30, and >30 mmHg-years of exposure, respectively, p<.001). This association remained strong after adjusting for blood pressure elevation after age 35 and other coronary risk factors and participant characteristics.
Limitations
Coronary calcium, though a strong predictor of future coronary heart disease, is not a clinical outcome.
Conclusions
Prehypertension during young adulthood is common and associated with coronary atherosclerosis 20 years later. Keeping systolic pressure below 120 mmHg before age 35 may provide important health benefits later in life.
INTRODUCTION
High blood pressure in middle-aged and older populations is a strong risk factor for cardiovascular disease(1). Among adults aged 40 and older, each 20 mmHg increase in systolic blood pressure is associated with an approximate doubling in the short-term risk (within 5 years) of a cardiovascular disease event(2, 3). Clinical trials show that lowering blood pressure with antihypertensive medications lowers this short term risk(4), but damage from blood pressure elevation appears to accumulate over time, such that damage from prior exposure may not be completely reversible with treatment later in life. Cohort studies in the elderly show that blood pressure elevation even 20–30 years in the past is associated with cardiovascular events(5, 6) and atherosclerosis(7) independent of current blood pressure.
Less is known about the effects of blood pressure elevation during young adulthood. Though frank hypertension (systolic >140 and/or diastolic >90 mmHg) is rare before age 40, “prehypertension” (systolic 120–139 mmHg or diastolic 80–89 mmHg(1)) is more common(8, 9). Current guidelines recommend lifestyle modification without pharmacotherapy for persons with prehypertension in order to reduce the risk of developing hypertension(1, 10), but it is unclear whether prehypertension itself during young adulthood may cause vascular damage that persists later in life. In practice, sub-optimal blood pressure levels that remain below 140/90 mmHg are often ignored in young adults(8).
The Coronary Artery Risk Development in Young Adults (CARDIA) Study provides a unique opportunity to evaluate the consequences of prehypertension during young adulthood. Using CARDIA’s repeated measures of blood pressure starting at the outset of adulthood and continuing over 20 years of follow-up, we identified participants exposed to prehypertension between age 20 and 35, estimated cumulative exposure in “mmHg-years” (similar to “pack-years” of tobacco exposure), and observed associations with coronary calcium measured later in life.
METHODS
Study Design and Sample
CARDIA is a longitudinal cohort of 5115 black and white women and men recruited from 4 U.S. cities, aged 18–30 years and healthy at the time of enrollment in 1985(11, 12). Participants underwent a baseline examination and follow-up examinations at Years 2, 5, 7, 10, 15, and 20. For this investigation, we identified all CARDIA participants who received a cardiac computed tomography scan for coronary calcium in either the Year 15 or 20 follow-up examinations, and excluded participants who developed hypertension (systolic = 140 mmHg or diastolic = 90 mmHg or taking a blood pressure medication) before the age of 35.
Blood pressure
At each CARDIA examination, right arm blood pressure was measured three times after the participant had been sitting in a quiet room for five minutes. We used the average of the second and third readings. Measurements were made using a Hawksley (Hawksley; Sussex, United Kingdom) random zero sphygmomanometer until the last examination at Year 20, when concerns about mercury contained in the apparatus required a switch to the OmROn (Omron Corporation; Kyoto, Japan) HEM907XL sphygmomanometer. Dual measurement on a subgroup of participants was used to calibrate the new measurements and assure comparability.
Estimating systolic blood pressure trajectories and cumulative exposure
We used mixed models to estimate a blood pressure trajectory (systolic and diastolic) for each participant from age 20 up to the time of his or her coronary calcium measurement. We assumed that the trajectory for each participant had a constant slope within each decade of life (age 20–30, 30–40, 40–50), so we allowed each participant a different random intercept and 3 random slopes, modeled as deviations from race- and gender-specific mean trajectories (see Appendix for details).
Using these individual blood pressure trajectories, we then calculated an integrated, cumulative measure of years of exposure to blood pressure elevation for each participant, measured in “mmHg-years” (analogous to “pack-years” of cumulative tobacco smoke exposure), by calculating the area under the trajectory for each participant in the blood pressure range of interest. The area under the blood pressure trajectory before the age of 35 and in the prehypertension range (120–139 mmHg systolic and 80–89 mmHg diastolic) was considered the primary predictor for this analysis: Cumulative exposure to prehypertension during young adulthood. The area under the blood pressure trajectory after age 35 was used as a covariate in the multivariable analysis.
Coronary calcium
Consenting CARDIA participants underwent cardiac computed tomography scanning at Year 15 and Year 20 to measure coronary calcium, which represents calcified plaque in the coronary arteries(13), with an electron beam or multi-detector electrocardiographically-gated cardiac computed tomography scanner(14). Two sequential coronary calcium scans were obtained using a standard phantom with known concentrations of calcium hydroxy-apatite. Imaging was performed using prospective gating in late diastole, a slice thickness of 2.5–3.0 mm, reconstruction into a 35 cm field-of-view, and with a temporal resolution of 100–520 (Year 15 exam) and 100–250 milliseconds (Year 20 exam). Experienced image analysts blinded to participant information and the paired scan measured calcified plaque in the epicardial coronary arteries and calculated a total coronary calcium score using a modified Agatston method to account for slice thickness(15), a minimum lesion size of 4 adjacent pixels (an area of at least 1.87 mm2), and a density greater than 130 Hounsfield units. An expert physician in cardiovascular imaging reviewed all scans that were discordant (one with and without coronary calcium), had a score>200, a change in calcium status between Year 15 and Year 20, a possible surgical intervention (pacemaker, valve replacement, coronary stent or bypass surgery) or a concern identified by the reader. The accuracy, comparability, reproducibility, and robustness of the calcium score using electron beam, helical and multi-detector computed tomography systems using these methods has been published(16, 17). For this analysis, we used the last non-missing coronary calcium measurement (i.e., the scan from Year 20, if available; otherwise the scan from Year 15).
Other measurements
Gender, ethnicity, date of birth, serum cotinine levels, and family history of premature coronary heart disease, defined by a mother or father with myocardial infarction before age 60, were ascertained at baseline. Fasting plasma levels of glucose (and diabetes status), low-density and high-density lipoprotein cholesterol (LDL and HDL) and triglycerides, as well as smoking habits from all CARDIA examinations were used. Other covariates, including educational grade attained and income (self-report), body mass index and waist circumference (directly measured), and physical activity (self-reported on a scale of 1–5) were taken from the time of the coronary calcium scan(18). Cumulative exposure to LDL, HDL, triglycerides and fasting glucose (without partition by age or level) were estimated using the same method as was used for blood pressure.
Statistical analysis
We described persons with and without prehypertension (systolic or diastolic) before age 35, and compared characteristics using t-tests (for continuous variables) and chi-square tests (for dichotomous variables). To estimate independent cross-sectional associations of various demographic factors with prehypertension before age 35, we constructed a multivariable logistic model regressing prehypertension before age 35 on age, sex, and all income-education combinations (three education and four income categories for a total of 12 combined income-education categories).
Cumulative blood pressure exposure variables, including the primary predictor, were right-skewed with most participants having zero exposure, and the relationships between these continuous cumulative exposure measures and coronary calcium prevalence were closer to linear after log-transformation of the cumulative exposure measure (adding one mmHg-year unit before the log-transformation). Our main adjusted results are presented, therefore, using these log-transformed cumulative exposure measures as continuous predictors. Results are also presented using categorized cumulative exposure measures. Trends across categories and trend interactions are calculated using adjusted Wald tests of linear combinations of regression coefficients.
We used logistic regression to analyze the association between blood pressure elevation and presence/absence of coronary calcium. We first analyzed the association of coronary calcium with categories of systolic and diastolic prehypertension, with simple adjustment and/or stratification for age, sex and race, and current blood pressure. We then fit models for our primary predictor (cumulative exposure to prehypertension before age 35) adjusting for a-priori specified potential confounders flexibly modeled using linear spline knots where suggested by linearity plots. These included demographics (age, sex, race, income and education), standard coronary risk factors (current blood pressure, diabetes, LDL, HDL and triglycerides, family history of premature coronary heart disease and pack-years of tobacco exposure), baseline serum cotinine, alcohol consumption, body mass index, waist circumference and physical activity, as well as cumulative exposure measurements for LDL, HDL, triglycerides, fasting glucose, and systolic blood pressure elevation after age 35. We also fit adjusted models after excluding all participants who met criteria for hypertension at any age. Hosmer-Lemeshow chi-squared statistics are reported to describe goodness-of-fit for each model. Sensitivity analyses were performed stratifying by baseline age, using diastolic blood pressure instead of systolic, using systolic prehypertension exposure in lower exposure ranges (120–129 and <120 mmHg), and using ordinal logistic regression with coronary calcium score categories of 0, 1–10, 11–100, and >100 as the outcome.
Role of the Funding Source
The CARDIA Study is funded by the National Heart, Lung and Blood Institute, which oversees conduct of the study and reviews manuscripts. The study, and our analysis of the data, has been approved by all relevant institutional review boards.
RESULTS
Of 5115 CARDIA participants enrolled in 1985–6, 3549 CARDIA participants attended the Year 20 examination, and 3138 CARDIA participants received a coronary calcium scan at that time. An additional 558 participants who received a coronary calcium scan only at Year 15 were also eligible. Of these 3696 participants, 136 with hypertension before age 35 were excluded, leaving 3560 participants in the study sample. Blood pressure measurements were missing at one or more examinations for 24% (842) of participants, but mixed modeling yielded trajectory estimates for all 3560 participants (see Methods). About half of participants were black (46%), half were female (56%), and the average age was 44 years at the time of the index coronary calcium scan (at Year 20, if available; otherwise at Year 15). Coronary calcium was present in 17% of participants, and scores were mostly low; only 3% of participants had extensive calcification with a calcium score greater than 100.
Nearly one fifth of this cohort (635 participants) developed prehypertension before age 35. These participants were more likely to be black, male, and to have lower levels of education and income (Table 1). Multivariable logistic analysis demonstrated independent, cross-sectional associations between presence of prehypertension before age 35 and black race/ethnicity (adjusted odds ratio 2.0; 95% confidence interval 1.6–2.4) and male sex (4.2; 3.4–5.1), as well as a strong socioeconomic status gradient: participants with low income (<$25,000/year) and no college education were about twice as likely to have had early prehypertension (adjusted odds ratio 2.3; 95% confidence interval 1.5–3.6) as participants with post-graduate education and an annual income over $100,000. Prehypertension before age 35 was also associated with overweight, diabetes, low HDL levels, and higher exposure to blood pressure elevation later in life (Table 1).
Table 1.
Characteristics of participants with and without prehypertension before age 35
| Prehypertension† before age 35
|
|||
|---|---|---|---|
| Characteristics at the time of the coronary calcium measurement* | Absent n = 2925 | Present n = 635 | P-value |
| Age, years, mean (SD) | 44.5 (4.1) | 44.1 (4.1) | .009 |
| Sex, % male | 38% | 70% | <.001 |
| Race/ethnicity, % black | 43% | 61% | <.001 |
| Never went to college, % | 22% | 33% | <.001 |
| Income < $25,000/year, % | 14% | 21% | <.001 |
| Family history of premature coronary disease, % | 12% | 13% | .28 |
| Ever smoked, % | 44% | 43% | .45 |
| Low self-reported physical activity‡, % | 21% | 24% | .117 |
| Body mass index ≥ 30 kg/m2, % | 33% | 53% | <.001 |
| Glucose intolerance, % | 7% | 12% | <.001 |
| Low-density lipoprotein cholesterol, mmol/L§, mean (SD) | 2.85 (.80) | 2.93 (.91) | .162 |
| High-density lipoprotein cholesterol, mmol/L§, mean (SD) | 1.42 (.44) | 1.27 (.36) | <.001 |
| Current blood pressure, mmHg, mean (SD) | 113 (12) | 130 (15) | <.001 |
| Cumulative exposure to systolic blood pressure elevation before age 35||, mmHg-years, mean (SD) | 0 (0) | 25 (38) | <.001 |
| Cumulative exposure to systolic blood pressure elevation after age 35||, mmHg-years, mean (SD) | 5 (19) | 65 (77) | <.001 |
| Duration of prehypertension, years, mean (SD) | 1 (2) | 12 (10) | <.001 |
- Characteristics measured at the time of the coronary calcium scan (Year 20, or Year 15 if a scan at Year 20 is not available). Some participants were missing information on education (n = 72), income (n = 124), or lipid measurements (n = 247).
- Prehypertension is defined by a systolic blood pressure of 120–139 mmHg and/or a diastolic of 80–89 mmHg
- Low self-reported physical activity is defined by an answer of 1 or 2 on a scale of 1–5, where 3 is “moderately active”.
- Convert cholesterol measurements from mmol/L to mg/dl by multiplying by 38.61
Cumulative exposure to systolic blood pressure elevation is measured in mmHg-years (analogous to “pack-years” of tobacco exposure), measured by calculating the area under the systolic blood pressure trajectory above 120 mmHg. For example, a person with a flat systolic blood pressure trajectory of 130 from age 20 to age 45 would accumulate 150 mmHg-years ((130-120 mmHg)*(35-20 years)) before age 35 and 100 mmHg-years ((130-120 mmHg)*(45-35 years)) after age 35. Before age 35, cumulative exposure occurs completely in the prehypertension range (120–139 mmHg) since all participants any value over 140 mmHg before the age of 35 are excluded. Trajectories are estimated using mixed models.
SD – Standard deviation
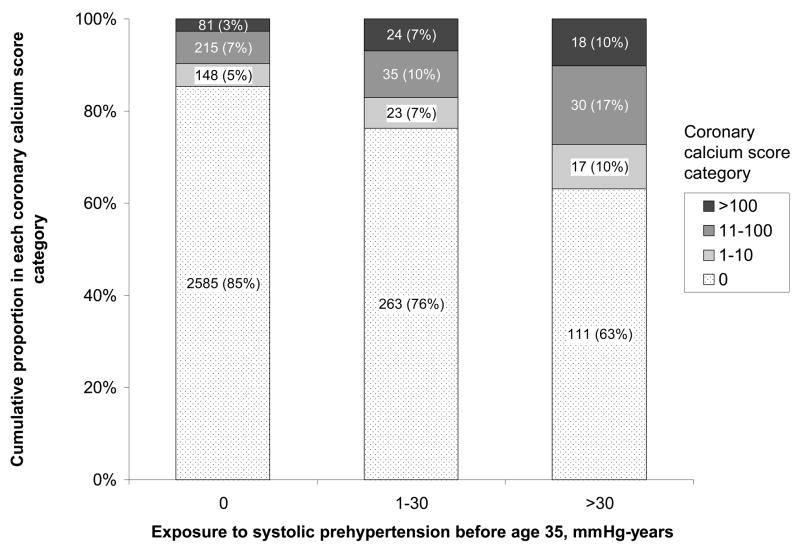
Increasing exposure to systolic prehypertension during young adulthood was strongly associated with presence and extent of coronary calcium later in life (Figure 1). Participants with exposure greater than 30 mmHg-years were two to three times as likely to have any coronary calcium (38% vs. 15%, p<.001), a coronary calcium score greater than 10 (27% vs. 10%, p<.001), and extensive calcification with a score greater than 100 (10% vs. 3%, p<.001) than persons without any exposure to systolic prehypertension during young adulthood. Diastolic prehypertension was less strongly associated with age- and sex-adjusted prevalence of coronary calcium than systolic prehypertension, and the prevalence of coronary calcium among participants with isolated diastolic prehypertension (without systolic prehypertension) was no higher than it was among participants without any prehypertension exposure (Table 2).
Figure 1. Coronary Calcium Score Distribution in Middle Age with Increasing Exposure to Systolic Prehypertension Before Age 35.
Cumulative exposure to systolic prehypertension is measured by calculating the area under the systolic blood pressure trajectory in mmHg-years (analogous to “pack-years” of tobacco exposure, see Methods). The association with coronary calcium score category is statistically significant (p<.001). Numbers (%) inside bars refer to the number of participants (percent of group total); ten persons with a positive coronary calcium scan but an unknown coronary calcium score were excluded from this analysis.
Table 2.
Prehypertension exposure during young adulthood and coronary calcium
| Prevalence of coronary calcium (95% CI)
|
||||
|---|---|---|---|---|
| Exposure categories* | N | Unadjusted | Adjusted for age, sex and race† | p-value‡ |
| Overall | 3560 | .17 (.16–.18) | .17 (.15–.18) | N/A |
| Prehypertension before age 35 | ||||
| None | 2925 | .15 (.14–.16) | .15 (.14–.17) | |
| Any prehypertension before age 35 | 635 | .26 (.23–.30) | .23 (.20–.27) | <.001 |
| Systolic prehypertension only | 274 | .29 (.24–.35) | .24 (.19–.29) | .002 |
| Diastolic prehypertension only | 111 | .15 (.09–.23) | .13 (.08–.21) | .28 |
| Systolic and diastolic prehypertension | 250 | .28 (.23–.34) | .27 (.21–.33) | <.001 |
| Exposure to systolic prehypertension before age 35, mmHg-years§ | ||||
| 0 | 3036 | .15 (.14–.16) | .15 (.14–.17) | <.001 |
| 1–30 | 346 | .24 (.20–.29) | .21 (.17–.26) | |
| >30 | 178 | .38 (.31–.45) | .35 (.28–.43) | |
| Exposure to diastolic prehypertension before age 35, mmHg-years§ | ||||
| 0 | 3199 | .16 (.15–.17) | .16 (.15–.18) | .007 |
| 1–20 | 285 | .23 (.18–.28) | .22 (.17–.27) | |
| >20 | 76 | .28 (.18–.39) | .24 (.16–.35) | |
- Prehypertension before age 35 is defined by systolic 120–139 or diastolic 80–89 mmHg.
- Adjusted prevalence estimates are derived from a logistic model in which sex and race are held constant (at average values) and age is held constant at 46 years (this age chosen so that the overall adjusted prevalence would match the unadjusted prevalence).
- P-values refer to an adjusted comparison of the proportion with coronary calcium in the given categories of prehypertension versus the “None” category, or to adjusted Wald tests of linear combinations of regression coefficients for tests of trend.
- Cumulative exposure to prehypertension is measured in mmHg-years (analogous to “pack-years” of tobacco exposure), measured by calculating the area under the blood pressure trajectory. For example, a person with a flat systolic blood pressure trajectory of 130 from age 20 to age 35 would accumulate 150 mmHg-years ((130-120 mmHg)*(35-20 years)). Cumulative exposure is estimated for systolic blood pressure (in the 120–139 mmHg range) and diastolic blood pressure (in the 80–89 mmHg range) separately, and categorized using round-number thresholds that provide sample sizes in each category that are of adequate size for stable prevalence estimation. Trajectories are estimated using mixed models.
Prehypertension exposure before age 35 was moderately correlated with blood pressure later in life (Spearman rho = .42 for rank correlation between cumulative exposure to systolic prehypertension before age 35 and systolic blood pressure measured at the time of the coronary calcium scan). The association between prehypertension before age 35 and coronary calcium, however, appears to be independent of blood pressure elevation later in life, showing consistent trends among subgroups of participants stratified by current blood pressure (Table 3). Current blood pressure, in contrast, was not associated with coronary calcium among persons with any exposure to systolic prehypertension before age 35 (p = .27). When we examined the prehypertension-coronary calcium association in the different race/sex subgroups in our sample, we found no evidence of an interaction (p = .23, Table 3).
Table 3.
Adjusted Prevalence of Coronary Calcium By Category of Systolic Prehypertension Exposure and By Sex and Race
| Strata | N | Adjusted* prevalence (95% confidence interval) of coronary calcium by prehypertension exposure category, mmHg-years† |
p-value‡ |
|||
|---|---|---|---|---|---|---|
| 0 | 1–30 | >30 | trend | interaction | ||
| Overall | .15 (.14–.17) | .19 (.15–.24) | .31 (.24–.40) | <.001 | -- | |
| Current blood pressure, mmHg | ||||||
| <120 | 2336 | .14 (.12–.15) | .19 (.12–.28) | .42 (.23–.63) | <.001 | .27 |
| 120–139 | 914 | .18 (.15–.22) | .21 (.15–.27) | .31 (.22–.41) | .005 | |
| ≥140 | 196 | .26 (.17–.36) | .26 (.16–.38) | .43 (.29–.59) | .053 | |
| Sex/Race | ||||||
| White men | 895 | .30 (.26–.33) | .34 (.26–.44) | .42 (.29–.55) | .068 | .23 |
| White women | 1027 | .09 (.07–.11) | .23 (.10–.44) | .28 (.04–.80) | .26 | |
| Black men | 675 | .21 (.17–.25) | .27 (.18–.37) | .44 (.32–.56) | <.001 | |
| Black women | 963 | .10 (.08–.13) | .09 (.04–.17) | .35 (.19–.55) | <.001 | |
- All adjusted prevalence estimates come from models in which age is set to 46 years (chosen so that the overall adjusted prevalence would match the unadjusted prevalence), and current systolic blood pressure, race and sex are either set to average values (116 mmHg for blood pressure) or categorized and used to stratify the analysis.
- Cumulative exposure to systolic blood pressure elevation is measured in mmHg-years (analogous to “pack-years” of tobacco exposure), measured by calculating the area under the systolic blood pressure trajectory above 120 mmHg. For example, a person with a flat systolic blood pressure trajectory of 130 from age 20 to age 45 would accumulate 150 mmHg-years ((130-120 mmHg)*(35-20 years)) before age 35. Trajectories are estimated using mixed models. Cumulative exposure is categorized using round-number thresholds that provide sample sizes in each category that are of adequate size for stable prevalence estimation.
- P-values for trend and interaction calculated using adjusted Wald tests of linear combinations of regression coefficients.
Multivariable analyses adjusting for other coronary heart disease risk factors, and for cumulative exposure to prehypertension and frank hypertension after age 35 show that prehypertension before age 35 remains a strong, independent risk factor for coronary calcium (Table 4). Each 1 log increase in cumulative exposure to prehypertension before age 35 is associated with a fully adjusted odds ratio of 1.14 (95% CI: 1.03–1.27) among all participants, or 1.22 (95% CI: 1.05–1.42) after excluding those with hypertension. The Hosmer-Lemeshow chi-squared statistic provides evidence for lack of fit in the first model (X2(8) = 20.6, p = .008), but not in the second (X2(8) = 8.5, p = .39). Results are similar for minimally adjusted models (including only age, sex, race and blood pressure exposure later in life, analogous odds ratio 1.14; 95% CI: 1.03–1.26), for fully adjusted ordinal logistic regression with coronary calcium score categories of 0, 1–10, 11–100 and >100 as the outcome (odds ratio 1.15; 95% CI: 1.04–1.28), and when stratified by baseline age (odds ratio = 1.22; 95% CI: 1.03–1.46 for baseline age<26 and 1.09; 95% CI: 0.94–1.26 for baseline age≥26). Diastolic prehypertension showed a non-statistically-significant association in the same direction (1.07, 95%CI: .89–1.29).
Table 4.
Adjusted associations between non-optimal systolic blood pressure (>120 mmHg) before and after age 35 with coronary calcium
| Adjusted odds ratios† (95% confidence interval) for coronary calcium
|
||
|---|---|---|
| Exposure to elevation in systolic blood pressure, per ln(mmHg-years+1)* | Full sample‡ | Excluding hypertensives§ |
| Before age 35 | 1.14 (1.03–1.27) | 1.22 (1.05–1.42) |
| After age 35 | 1.05 (.97–1.13) | 1.00 (0.89–1.11) |
- Cumulative exposure to systolic blood pressure elevation is measured in mmHg-years (analogous to “pack-years” of tobacco exposure), measured by calculating the area under the systolic blood pressure trajectory above 120 mmHg. For example, a person with a flat systolic blood pressure trajectory of 130 from age 20 to age 45 would accumulate 150 mmHg-years ((130-120 mmHg)*(35-20 years)) before age 35 and 100 mmHg-years ((130-120 mmHg)*(45-35 years)) after age 35. Before age 35, cumulative exposure occurs completely in the prehypertension range (120–139 mmHg) since all participants with hypertensive-range elevation (>140 mmHg) before the age of 35 are excluded. Trajectories are estimated using mixed models. Cumulative exposure measures are log-transformed (after adding 1) for linearity.
- All analyses are mutually adjusted for exposure to blood pressure elevation before and after age 35, as well as age, sex, race, income, education, body mass index, waist circumference, self-reported physical activity, alcohol consumption, baseline serum cotinine, family history of premature coronary heart disease, and coronary heart disease risk factors including current and cumulative measures of low-density and high-density lipoprotein cholesterol levels (LDL and HDL), triglycerides, fasting glucose (and glucose intolerance), and tobacco exposure. Note that an odds ratio of 1.14 is equivalent to a risk or prevalence ratio of 1.11 when the proportion with the outcome is 17% (equal to the prevalence of coronary calcium in the study sample).
- The full multivariable analysis sample (n = 3375) excludes participants missing data on LDL (n = 249), HDL (n = 209), fasting glucose (n = 217), alcohol consumption (n = 74), baseline serum cotinine (n = 28), body mass index (94), waist circumference (n = 7), or physical activity (n = 64, n = 340 total exclusions).
- Hypertensive participants (n = 587) are defined by a blood pressure = 140 mmHg systolic or = 90 mmHg diastolic or who reported taking antihypertensive medications at any examination. All such participants developed hypertension after age 35 since we excluded those developing hypertension before age 35
When we focused our analysis on exposure to systolic blood pressure elevation in the range of 120–129 mmHg, excluding those with systolic blood pressure trajectories = 130 mmHg before age 35 and adjusting for blood pressure elevation after age 35 and other risk factors, the association was undiminished in size (adjusted odds ratio 1.13, 95%CI: 1.00–1.27). Even levels of systolic blood pressure under 120 mmHg before age 35 (after excluding persons with prehypertension before age 35 and adjusting for blood pressure exposure after age 35) were associated with coronary calcium later in life (adjusted odds ratio 1.26 per 100 mmHg-years exposure, 95%CI: 1.02–1.55).
DISCUSSION
Prehypertension exposure before age 35 is common and strongly associated with coronary calcium later in life. This relationship is independent of other coronary heart disease risk factors, independent of exposure to prehypertension or frank hypertension after age 35, and consistent across race/sex subgroups. Systolic prehypertension is more strongly associated with coronary calcium than diastolic prehypertension, and it is more common in blacks, men, and those with low socioeconomic status or obesity. Even systolic pressures in the 120–129 mmHg range are associated with subsequent coronary calcium.
As an illustration of effect size, consider a person with a flat systolic blood pressure trajectory of 130 mmHg from the age of 20 to 35 years. This person would accumulate 150 mmHg-years ((130–120 mmHg)*(35–20 years)) of exposure to prehypertension during young adulthood. Our models estimate that the relative likelihood of having coronary calcium later in life would be 70% higher (converted from an odds ratio of 1.94) than someone whose systolic blood pressure remains below 120 until the age of 35, independent of blood pressure elevation later in life and other risk factors.
Our new finding – that prehypertension in young adults is associated with coronary calcium later in life – suggests the possibility that prehypertension itself is harmful, and not just because it is associated with subsequent hypertension. This finding extends previous findings in middle-aged and older adults showing associations between prehypertension and cardiovascular disease(1–3, 19–27), and findings in children or young adults that have demonstrated cross-sectional associations between blood pressure levels and atherosclerosis(28, 29) and left ventricular hypertrophy(30), and longitudinal associations with arterial stiffness(31–33), endothelial dysfunction(34), microalbuminuria(35) and renal function(36), carotid intima-media thickness(37–40), and coronary calcium(41, 42). Our study is unique in size (overall and for the four race-gender subgroups), in the two decades of follow-up before measuring coronary calcium during middle age, and in the specific isolation of the association with sub-optimal blood pressure during young adulthood with control of confounding from other risk factors including blood pressure elevation later in life.
We also found that blood pressure levels during young adulthood were more strongly associated with middle-age coronary calcium than blood pressure measured at the time of the coronary calcium scan. This suggests the possibility that young adulthood is a critical period in life when exposure to suboptimal blood pressure is particularly important. Calcification of a damaged vessel may occur many years after the actual insult(43), and represents a stage of the disease process that would not be expected to reverse with antihypertensive treatment. Conversely, damage occurring from high blood pressure during middle age may have had an insufficient latency period to calcify to a measurable size by the time of the coronary calcium scan. Consistent with previous studies of blood pressure and atherosclerosis, we would expect damage from untreated prehypertension or hypertensive-level elevations in blood pressure to continue to accumulate at older ages(7).
Our finding that prehypertension during young adulthood is more common in blacks, men, and participants with lower income and education is consistent with previous reports(44–46). The discovery that these disparities occur early in adulthood has important implications for targeting of blood pressure control efforts. Our findings also suggest that racial and socioeconomic disparities in cardiovascular event rates may be partially explained by more adverse risk factor trajectories (including for blood pressure and also possibly other risk factors) starting early in life.
Several limitations are worth noting. Despite standardized approaches to measuring blood pressure at seven examinations over 20 years, our findings are susceptible to error from measurement and from variation in blood pressure between examinations. Our mixed modeling approach should minimize these problems, but random error could result in underestimation of true associations with coronary calcium (regression dilution bias(47)). We rely on a subclinical endpoint (coronary calcium) because our cohort is still too young to have suffered enough cardiovascular events to validate our findings using a clinical endpoint; coronary calcium, however, is a strong, independent predictor of future events(48–50). As with any observational study, residual confounding could have influenced our findings.
Our findings support efforts to optimize blood pressure early in adulthood. In 2003, the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC7) defined prehypertension, describing it as “not a disease category” but “a designation chosen to identify individuals at high risk of developing hypertension”, and recommended that lifestyle modification (e.g. regular physical activity, healthy eating and weight control) be implemented with the goal of lowering blood pressure to less than120/80 mmHg and preventing progression to hypertension(1). The British Hypertension Society considers systolic blood pressures of 120–129 mmHg “normal”, and 130–139 “high normal”; and neither this Society nor the World Health Organization recommend treatment at these levels(10, 51). None of the three guidelines specifically addresses young adults. Our findings add a new basis for the relatively low blood pressure goal advocated by JNC7, and emphasize the importance of addressing prehypertension, at least with lifestyle modification, during young adulthood in particular. While our findings raise the possibility that treatment of prehypertension during young adulthood with blood pressure lowering medications could also be beneficial, these benefits have not been confirmed by a randomized trial in this population, and would have to be weighed against the lack of expected benefits in the short term, the potential for side effects from very long-term medication exposure, and the costs.
Optimizing blood pressure in young adults will be a major challenge. Even treatment of frank hypertension in young adults is difficult. Hypertensive adults under age 40 surveyed in the National Health and Nutrition Examination Survey 1999–2000 were less aware of their high blood pressure(8), less likely to take medicine if they were aware(8), and less likely to be adequately treated than older hypertensive adults(8, 52). Regardless of whether these age discrepancies in blood pressure control represent reluctance of physicians or resistance of patients to treatment, aggressive control of prehypertension in young adults is likely to meet similar obstacles. Our results suggest, however, that a concerted effort to attain optimal blood pressure in early adulthood may yield substantial health benefits for individuals and reduce population rates of clinical cardiovascular disease during middle-age and beyond.
Supplementary Material
Acknowledgments
The CARDIA study is supported by contracts N01-HC-48047, N01-HC-48048, N01-HC-48049, N01-HC-48050, and N01-HC-95095 from the National Heart, Lung, and Blood Institute, which reviewed the manuscript. Dr. Pletcher had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis
Funding sources and financial interests: The Coronary Artery Risk Development in Young Adults Study is supported by contracts N01-HC-48047, N01-HC-48048, N01-HC-48049, N01-HC-48050, and N01-HC-95095 from the National Heart, Lung, and Blood Institute
Footnotes
REPRODUCIBLE RESEARCH STATEMENTS
CARDIA Protocol/Methods: Available at http://www.cardia.dopm.uab.edu/
Statistical Code: Available to interested readers by contacting Dr. Pletcher (mpletcher@epi.ucsf.edu)
Data: A limited access dataset is available through NHLBI at http://www.nhlbi.nih.gov/resources/deca/descriptions/cardia.htm
AUTHOR INFORMATION Mark J. Pletcher, MD, MPH (for reprint requests), 185 Berry Street, Suite 5700 San Francisco, CA 94107
Kirsten Bibbins-Domingo, PhD, MD, Box 1364, SFGH Bldg 10, WD 13 1313, University of California, San Francisco, San Francisco, CA 94143-1364
Cora E. Lewis, MD, 1717 11th Avenue South, STE 614, Birmingham, AL 35205
Gina S. Wei, MD, MPH, 6701 Rockledge Drive, Suite 10018, Bethesda, MD 20892-7936
Steve Sidney, MD, MPH, Division of Research, Kaiser Permanente, 2000 Broadway, Oakland, CA 94612
J. Jeffrey Carr, MD, MSCE, 2000 West 1st Street, Two Piedmont Plaza, Suite 618, Winston-Salem, NC 27104-4225
Eric Vittinghoff, PhD, 185 Berry Street, Suite 5700, San Francisco, CA 94107
Charles E. McCulloch, PhD, 185 Berry Street, Suite 5700, San Francisco, CA 94107
Stephen B. Hulley, MD, MPH, 185 Berry Street, Suite 5700, San Francisco, CA 94107
Publisher's Disclaimer: This is the pre-publication, author-produced version of a manuscript accepted for publication in Annals of Internal Medicine. This version does not include post-acceptance editing and formatting. The American College of Physicians, the publisher of Annals of Internal Medicine, is not responsible for the content or presentation of the author-produced accepted version of the manuscript or any version that a third party derives from it. Readers who wish to access the definitive published version of this manuscript and any ancillary material related to this manuscript (correspondence, corrections, editorials, linked articles, etc.) should go to www.annals.org or to the print issue in which the article appears. Those who cite this manuscript should cite the published version, as it is the official version of record.
References
- 1.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345(18):1291–7. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 4.Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists’ Collaboration. Lancet. 2000;356(9246):1955–64. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- 5.Seshadri S, Wolf PA, Beiser A, et al. Elevated midlife blood pressure increases stroke risk in elderly persons: the Framingham Study. Arch Intern Med. 2001;161(19):2343–50. doi: 10.1001/archinte.161.19.2343. [DOI] [PubMed] [Google Scholar]
- 6.Vasan RS, Massaro JM, Wilson PW, et al. Antecedent blood pressure and risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2002;105(1):48–53. doi: 10.1161/hc0102.101774. [DOI] [PubMed] [Google Scholar]
- 7.Wilson PW, Hoeg JM, D’Agostino RB, et al. Cumulative effects of high cholesterol levels, high blood pressure, and cigarette smoking on carotid stenosis. N Engl J Med. 1997;337(8):516–22. doi: 10.1056/NEJM199708213370802. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med. 2004;164(19):2126–34. doi: 10.1001/archinte.164.19.2126. [DOI] [PubMed] [Google Scholar]
- 9.Ostchega Y, Yoon SS, Hughes J, Louis T National Center for Health Statistics. Hypertension awareness, treatment, and control -- continued disparities in adults: United States, 2005–2006. 2008 [PubMed] [Google Scholar]
- 10.Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ. 2004;328(7440):634–40. doi: 10.1136/bmj.328.7440.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hughes GH, Cutter G, Donahue R, et al. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (Cardia) Study. Control Clin Trials. 1987;8(4 Suppl):68S–73S. doi: 10.1016/0197-2456(87)90008-0. [DOI] [PubMed] [Google Scholar]
- 12.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–16. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 13.Budoff MJ, Achenbach S, Blumenthal RS, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114(16):1761–91. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 14.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234(1):35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 15.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 16.Carr JJ, Crouse JR, 3rd, Goff DC, Jr, D’Agostino RB, Jr, Peterson NP, Burke GL. Evaluation of subsecond gated helical CT for quantification of coronary artery calcium and comparison with electron beam CT. AJR Am J Roentgenol. 2000;174(4):915–21. doi: 10.2214/ajr.174.4.1740915. [DOI] [PubMed] [Google Scholar]
- 17.Detrano RC, Anderson M, Nelson J, et al. Coronary calcium measurements: effect of CT scanner type and calcium measure on rescan reproducibility--MESA study. Radiology. 2005;236(2):477–84. doi: 10.1148/radiol.2362040513. [DOI] [PubMed] [Google Scholar]
- 18.Bild DE, Jacobs DR, Liu K, et al. Seven-year trends in plasma low-density-lipoprotein-cholesterol in young adults: the CARDIA Study. Ann Epidemiol. 1996;6(3):235–45. doi: 10.1016/1047-2797(96)00005-1. [DOI] [PubMed] [Google Scholar]
- 19.Qureshi AI, Suri MF, Mohammad Y, Guterman LR, Hopkins LN. Isolated and borderline isolated systolic hypertension relative to long-term risk and type of stroke: a 20-year follow-up of the national health and nutrition survey. Stroke. 2002;33(12):2781–8. doi: 10.1161/01.str.0000039402.05613.0f. [DOI] [PubMed] [Google Scholar]
- 20.Mainous AG, 3rd, Everett CJ, Liszka H, King DE, Egan BM. Prehypertension and mortality in a nationally representative cohort. Am J Cardiol. 2004;94(12):1496–500. doi: 10.1016/j.amjcard.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 21.Liszka HA, Mainous AG, 3rd, King DE, Everett CJ, Egan BM. Prehypertension and cardiovascular morbidity. Ann Fam Med. 2005;3(4):294–9. doi: 10.1370/afm.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qureshi AI, Suri MF, Kirmani JF, Divani AA, Mohammad Y. Is prehypertension a risk factor for cardiovascular diseases? Stroke. 2005;36(9):1859–63. doi: 10.1161/01.STR.0000177495.45580.f1. [DOI] [PubMed] [Google Scholar]
- 23.Psaty BM, Arnold AM, Olson J, et al. Association between levels of blood pressure and measures of subclinical disease multi-ethnic study of atherosclerosis. Am J Hypertens. 2006;19(11):1110–7. doi: 10.1016/j.amjhyper.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Lee ET, Devereux RB, et al. Prehypertension, diabetes, and cardiovascular disease risk in a population-based sample: the Strong Heart Study. Hypertension. 2006;47(3):410–4. doi: 10.1161/01.HYP.0000205119.19804.08. [DOI] [PubMed] [Google Scholar]
- 25.Kshirsagar AV, Carpenter M, Bang H, Wyatt SB, Colindres RE. Blood pressure usually considered normal is associated with an elevated risk of cardiovascular disease. Am J Med. 2006;119(2):133–41. doi: 10.1016/j.amjmed.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 26.Conen D, Ridker PM, Buring JE, Glynn RJ. Risk of cardiovascular events among women with high normal blood pressure or blood pressure progression: prospective cohort study. BMJ. 2007;335(7617):432. doi: 10.1136/bmj.39269.672188.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reynolds K, Gu D, Muntner P, et al. A population-based, prospective study of blood pressure and risk for end-stage renal disease in China. J Am Soc Nephrol. 2007;18(6):1928–35. doi: 10.1681/ASN.2006111199. [DOI] [PubMed] [Google Scholar]
- 28.Berenson GS, Srinivasan SR, Bao W, Newman WPr, Tracey RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338(23):1650–6. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 29.McMahan CA, Gidding SS, Fayad ZA, et al. Risk scores predict atherosclerotic lesions in young people. Arch Intern Med. 2005;165(8):883–90. doi: 10.1001/archinte.165.8.883. [DOI] [PubMed] [Google Scholar]
- 30.Drukteinis JS, Roman MJ, Fabsitz RR, et al. Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the Strong Heart Study. Circulation. 2007;115(2):221–7. doi: 10.1161/CIRCULATIONAHA.106.668921. [DOI] [PubMed] [Google Scholar]
- 31.Li S, Chen W, Srinivasan SR, Berenson GS. Childhood blood pressure as a predictor of arterial stiffness in young adults: the Bogalusa Heart Study. Hypertension. 2004;43(3):541–6. doi: 10.1161/01.HYP.0000115922.98155.23. [DOI] [PubMed] [Google Scholar]
- 32.Urbina EM, Srinivasan SR, Kieltyka RL, et al. Correlates of carotid artery stiffness in young adults: The Bogalusa Heart Study. Atherosclerosis. 2004;176(1):157–64. doi: 10.1016/j.atherosclerosis.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 33.Juonala M, Jarvisalo MJ, Maki-Torkko N, Kahonen M, Viikari JS, Raitakari OT. Risk factors identified in childhood and decreased carotid artery elasticity in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation. 2005;112(10):1486–93. doi: 10.1161/CIRCULATIONAHA.104.502161. [DOI] [PubMed] [Google Scholar]
- 34.Juonala M, Viikari JS, Ronnemaa T, Helenius H, Taittonen L, Raitakari OT. Elevated blood pressure in adolescent boys predicts endothelial dysfunction: the cardiovascular risk in young Finns study. Hypertension. 2006;48(3):424–30. doi: 10.1161/01.HYP.0000237666.78217.47. [DOI] [PubMed] [Google Scholar]
- 35.Hoq S, Chen W, Srinivasan SR, Berenson GS. Childhood blood pressure predicts adult microalbuminuria in African Americans, but not in whites: the Bogalusa Heart Study. Am J Hypertens. 2002;15(12):1036–41. doi: 10.1016/s0895-7061(02)03066-2. [DOI] [PubMed] [Google Scholar]
- 36.Youssef AA, Srinivasan SR, Elkasabany A, Cruickshank JK, Berenson GS. Temporal relation between blood pressure and serum creatinine in young adults from a biracial community: the Bogalusa Heart Study. Am J Hypertens. 2000;13(7):770–5. doi: 10.1016/s0895-7061(00)00233-8. [DOI] [PubMed] [Google Scholar]
- 37.Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation. 2001;104(23):2815–9. doi: 10.1161/hc4601.099486. [DOI] [PubMed] [Google Scholar]
- 38.Raitakari OT, Juonala M, Kahonen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290(17):2277–83. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 39.Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290(17):2271–6. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 40.Johnson HM, Douglas PS, Srinivasan SR, et al. Predictors of carotid intima-media thickness progression in young adults: the Bogalusa Heart Study. Stroke. 2007;38(3):900–5. doi: 10.1161/01.STR.0000258003.31194.0a. [DOI] [PubMed] [Google Scholar]
- 41.Mahoney LT, Burns TL, Stanford W, et al. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcificaction in young adults: the Muscatine Study. J Am Coll Cardiol. 1996;27(2):277–84. doi: 10.1016/0735-1097(95)00461-0. [DOI] [PubMed] [Google Scholar]
- 42.Loria CM, Liu K, Lewis CE, et al. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol. 2007;49(20):2013–20. doi: 10.1016/j.jacc.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 43.Stary HC, Chandler AB, Dinsmore RE, et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler Thromb Vasc Biol. 1995;15(9):1512–31. doi: 10.1161/01.atv.15.9.1512. [DOI] [PubMed] [Google Scholar]
- 44.Marmot MG, Smith GD, Stansfeld S, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337(8754):1387–93. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- 45.Iribarren C, Luepker RV, McGovern PG, Arnett DK, Blackburn H. Twelve-year trends in cardiovascular disease risk factors in the Minnesota Heart Survey. Are socioeconomic differences widening? Arch Intern Med. 1997;157(8):873–81. [PubMed] [Google Scholar]
- 46.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165(18):2098–104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 47.MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335(8692):765–74. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- 48.Pletcher MJ, Tice JA, Pignone M, Browner WS. Using the coronary artery calcium score to predict coronary heart disease events: a systematic review and meta-analysis. Arch Intern Med. 2004;164(12):1285–92. doi: 10.1001/archinte.164.12.1285. [DOI] [PubMed] [Google Scholar]
- 49.Greenland P, Bonow RO, Brundage BH, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) Circulation. 2007;115(3):402–26. doi: 10.1161/CIRCULATIONAHA..107.181425. [DOI] [PubMed] [Google Scholar]
- 50.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358(13):1336–45. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 51.Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21(11):1983–92. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 52.Gu Q, Paulose-Ram R, Dillon C, Burt V. Antihypertensive medication use among US adults with hypertension. Circulation. 2006;113(2):213–21. doi: 10.1161/CIRCULATIONAHA.105.542290. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.