Abstract
Fueled by the rapid pace of discovery, humankind's ability to understand the ultimate causes of preventable common disease burdens and to identify solutions is now reaching a revolutionary tipping point. Achieving optimal health and well-being for all members of society lies as much in the understanding of the factors identified by the behavioral, social, and public health sciences as by the biological ones. Accumulating advances in mathematical modeling, informatics, imaging, sensor technology, and communication tools have stimulated several converging trends in science: an emerging understanding of epigenomic regulation; dramatic successes in achieving population health-behavior changes; and improved scientific rigor in behavioral, social, and economic sciences. Fostering stronger interdisciplinary partnerships to bring together the behavioral–social–ecologic models of multilevel “causes of the causes” and the molecular, cellular, and, ultimately, physiological bases of health and disease will facilitate breakthroughs to improve the public's health.
The strategic vision of the Office of Behavioral and Social Sciences Research (OBSSR) at the National Institutes of Health (NIH) is rooted in a collaborative approach to addressing the complex and multidimensional issues that challenge the public's health. This paper describes OBSSR's four key programmatic directions (next-generation basic science, interdisciplinary research, systems science, and a problem-based focus for population impact) to illustrate how interdisciplinary and transdisciplinary perspectives can foster the vertical integration of research among biological, behavioral, social, and population levels of analysis over the lifespan and across generations. Interdisciplinary and multilevel approaches are critical both to the OBSSR's mission of integrating behavioral and social sciences more fully into the NIH scientific enterprise and to the overall NIH mission of utilizing science in the pursuit of fundamental knowledge about the nature and behavior of living systems and the application of that knowledge to extend healthy life and reduce the burdens of illness and disability.
Introduction
The vision of the National Institutes of Health (NIH) Office of Behavioral and Social Sciences Research (OBSSR) presented here provides an overview of the increasing role that transdisciplinary science and systems science methods are playing in transforming the understanding of the causality of health and disease in order to improve population-wide well-being. OBSSR, situated in the Office of the Director of the NIH, is mandated to stimulate, integrate, and increase support for behavioral and social sciences research across the 27 institutes and centers that constitute the NIH. OBSSR's other responsibilities include disseminating behavioral and social sciences research findings and providing advice to and communicating with the NIH Director, the legislature, other government agencies, the research community, and the general public on matters regarding behavioral and social sciences research. OBSSR serves as the nexus for cross-cutting research on the role that behavioral and social factors play in the etiology, treatment, and prevention of disease and in the promotion of health and improved quality of life. Additional information about OBSSR can be found at the Office's homepage (obssr.od.nih.gov).
There is growing recognition that the solutions to the most vexing public health problems are likely to be those that embrace the behavioral and social sciences as key players. To address this recognition, in 2007 OBSSR adopted a new strategic prospectus1 to guide future priorities in the behavioral and social sciences at NIH. At the core of OBSSR's vision is a vertical integration across the levels of scientific analysis, that is, a transdisciplinary integration of the biomedical paradigms of molecular and physiological causal mechanisms with the ecologic paradigms of multilevel (individual, group, community, societal, and global) “causes of the causes” of health and disease.2,3
A note on terminology: As described by Stokols et al.,4
Interdisciplinarity is a more robust approach to scientific integration in the sense that team members not only combine or juxtapose concepts and methods drawn from their own different fields, but also work more intensively to integrate their divergent perspectives, even while remaining anchored in their own respective fields. Transdisciplinarity is a process in which team members representing different fields work together over extended periods to develop shared conceptual and methodologic frameworks that not only integrate but also transcend their respective disciplinary perspectives.
Rosenfield5 suggests that the term interdisciplinary lies between multidisciplinary and transdisciplinary science, implying a continuum along which the terms lie. However, the terms interdisciplinary and transdisciplinary science are sometimes used interchangeably, both within and outside the NIH. In the short term, because much of the work described here by OBSSR involves moving from multidisciplinary to interdisciplinary science, the term interdisciplinary is used throughout most of this document. Interdisciplinary is also the most common term used in the NIH Roadmap for Medical Research.6 A long-term goal of OBSSR is to facilitate a process for moving from interdisciplinary analyses to the deeper conceptual synthesis and transformative momentum promised by transdisciplinary science.
The Value of Behavioral and Social Sciences Research Knowledge and Practice for Improving Public Health
A great deal is known about the basic science of how to change individual and population behavior. The application of findings from behavioral and social sciences research already plays a significant role in safeguarding and improving the public's health. The following selected examples provide a starting point to illustrate the tremendous power of psychosocial factors alone and the value of basic and applied behavioral and social sciences research in informing and improving the public's health.
Population and biological sciences identified tobacco-use behavior as the primary cause of most lung cancers and a leading cause of many other diseases, including cardiovascular disease. Behavioral and social sciences research informed the smoking interventions (individual, community, and policy level) that have spurred a dramatic reduction in U.S. tobacco use since its peak in the 1960s. In fact, the past decade witnessed a decline in overall cancer death rates for the first time in a century,7 driven largely by the dramatic reduction in male smoking rates, from 54.1% at their peak in 19658 to 23.9% today.9 Within the relatively short time span of 40 years, more than 45.7 million Americans have stopped smoking.9 This is arguably one of the most successful public health interventions in recorded history,10,11 and it has reduced the burden of many other diseases and excess societal expense as well. Behavioral and social sciences research can take much of the credit for this. Such research also has been at the center of understanding the multiple determinants of smoking initiation and cessation. Findings from behavioral and social sciences research have informed a broad spectrum of approaches (e.g., policy, cessation and prevention programs, communication of the risks associated with tobacco use). Of these, policy interventions (e.g., smoking bans, cigarette taxes) have been found to be among the most effective strategies for reducing smoking prevalence. (For in-depth treatment of this topic, see Ending the Tobacco Problem: A Blueprint for the Nation.12) Because of behavioral and social sciences research, tobacco use has been changed on a massive scale despite the highly addictive nature of nicotine.
Another achievement of behavioral and social sciences research is the landmark NIH Diabetes Prevention Program (DPP), which showed that lifestyle changes (i.e., alterations in dietary intake and physical activity that led to a reduction in body weight) were nearly twice as effective as a common medication in reducing the risk of developing type 2 diabetes.13 An interdisciplinary effort to harness the power of the DPP intervention trial, together with lessons learned from tobacco control (especially around policy interventions), could help reverse the obesity and type 2 diabetes epidemics sweeping the developed world, and perhaps do so in less time than it took to cut smoking prevalence in half.
Research in the behavioral and social sciences has also spawned great progress in the development of effective treatments for the mental illnesses and disorders that are the leading contributors to disability. Meta-analyses show that cognitive–behavioral therapy is effective for unipolar depression, generalized anxiety disorder, panic disorder with or without agoraphobia, social phobia, posttraumatic stress disorder, childhood depressive and anxiety disorders, marital distress, anger, childhood somatic disorders, and chronic pain.14 Moreover, cognitive–behavioral therapy is superior to antidepressants in the treatment of adult depression.14 Finally, while a combination of cognitive–behavioral therapy and fluoxetine has been shown to be equal to fluoxetine alone in alleviating moderate-to-severe depression in adolescents, adding cognitive–behavioral therapy improves the safety of the medication by reducing suicidal ideation and events.15
Another major public health success to which behavioral and social sciences research on decision making, drug abuse, and sexual behaviors has made a significant contribution is the mitigation of the spread of HIV/AIDS.16,17 As people have reduced their frequency of risky behaviors and new medications have become available, new AIDS cases in the U.S. have been cut almost in half, from a peak in 1992 of over 78,000 to approximately 40,000/year since 1998.18 The contributions from behavioral and social sciences research along with the development of effective pharmacotherapies have changed HIV from an imminent death sentence to a treatable, chronic disease. But for medications to be successful, they must be taken on a regular basis, and behavioral and social sciences research has contributed to significant, albeit modest, improvements in adherence.19 An effective partnership between the behavioral and social sciences and the biomedical sciences is at the core of the progress being made in the fight against HIV/AIDS worldwide.
Given the powerful discoveries and successes of basic and applied behavioral and social sciences research—largely achieved within single disciplinary silos without the scientific breakthroughs of recent times—OBSSR's vision is cautiously optimistic. It reflects a recognition that a new era is dawning in the 21st Century, an era for prevention and for re-engineering the lifestyles and environments that have been created previously. Lifestyle behaviors, social and physical environments, and policy and economic incentives can indeed be changed. Advances in biology, especially emergent work on epigenomics; dramatic successes in achieving population behavior changes; and improved rigor in behavioral, social, economic and population sciences are continuing apace, due in part to advances in mathematical modeling, informatics, imaging, sensor technology, spatial coding, cyber-infrastructure, and communication tools. These trends facilitate the understanding of the causes of preventable chronic, common diseases and poor health outcomes, and enable the development of targeted solutions. Changes are in order in the behavioral, social, chemical, and physical environments that are much more user-friendly to the fixed-DNA sequences of human beings. The new tools and technologies and the potential for interdisciplinary and, ultimately, transdisciplinary vertical synthesis from cells to society (e.g., Glass and McAtee20) set the stage for OBSSR's strategic vision for the future of both basic and applied behavioral and social sciences research at NIH and elsewhere.
Overview of OBSSR's Strategic Vision at NIH
The vision of OBSSR, as articulated in the strategic prospectus, is to mobilize the biomedical, behavioral, social, and population science research communities as partners to solve the most pressing health challenges faced by society.1 Such a transdisciplinary approach is called for because there is increasing awareness that the most daunting and intractable problems in public health are so because of their complexity, and that the failure to appreciate and adequately address this complexity is thwarting attempts to tackle these problems.21 Indeed, the health and well-being of the whole population may be best conceptualized as a “systems” problem, occurring on a continuum over the human lifespan as well as across a variety of levels of analysis, ranging from the cellular and molecular to individual and interpersonal behaviors, to the community and society and to macro-socioeconomic and global levels (Figure 1).22
Figure 1.
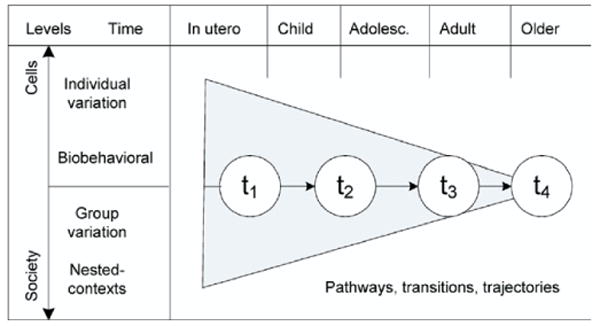
Transdisciplinary integration: from cells to society over time and across lifespan developmental phases
Reprinted with permission from Abrams22
The OBSSR at NIH has historically embraced a biopsychosocial perspective on the causes and correlates of health and illness.23,24 Extending the biopsychosocial model, Glass and McAtee20 provide an even stronger rationale for OBSSR's taking an interdisicplinary and systems science perspective to improve understanding of the forces that determine optimal health promotion and prevention, reduced disease burden, and improved chronic disease management across the human lifespan and across generations.
Consistent with the Glass and McAtee model of problem conceptualization,20 the OBSSR staff recognize that the health problems of the 21st Century are complex. Solving these problems not only demands a movement from interdisciplinarity to transdisciplinarity synthesis, but also dictates the methods needed for addressing them.25,26 OBSSR's emphasis on systems science reflects this awareness.
The OBSSR's Strategic Prospectus
The strategic prospectus recently published by OBSSR1 articulates four new programmatic directions, summarized below:
Next-generation basic science: OBSSR will facilitate the next generation of basic behavioral and social sciences research informed by breakthroughs in complementary areas such as genetics, informatics, computer science, measures, methods, and multilevel analyses.
Interdisciplinary research: OBSSR will facilitate collaborative research across the full range of disciplines and stakeholders necessary to fully elucidate the complex determinants of health and health-systems challenges. Such collaborations will yield new conceptual frameworks, methods, measures, and technologies that will speed the improvement of population health.
Systems science approaches to health: OBSSR will stimulate research that integrates multiple levels of analysis in problem conceptualization and recognizes the complex and dynamic relationships among components of the system. These approaches are required to understand the ways in which individual, contextual, and organizational factors interact to determine health status.
Population impact: OBSSR will work with its NIH partners to identify key issues in population health toward which scientists, practitioners, and decision makers can work together to accelerate the translation, dissemination, and implementation of the findings of BSSR in the service of improved health. This programmatic direction emphasizes a research agenda that is problem-focused and outcomes-oriented. It begins with a complex but clearly defined health problem and works backwards from the problem to identify the multiple causal pathways and feedback loops that will lead to development of the most powerful and efficient set of interventions to address the problem.
Interdisciplinarity is an explicit, programmatic theme within the OBSSR strategic prospectus that, in fact, pervades all other themes. A number of other cross-cutting themes also underlie OBSSR's programmatic directions. These themes include: (1) the elimination of health disparities22; (2) the strengthening of the science of dissemination (the quest for scientific evidence to determine the most effective ways to translate findings from basic research and clinical trials performed under ideal conditions to the successful widespread adoption and implementation by all target audiences and in national health policy)27,28; (3) capitalizing on recent advances in informatics, communications, imaging, sensor technology, and data-visualization techniques that aid data analysis and interpretation29; and (4) investigating commonality among theories and mechanisms of behavior change and sustained maintenance of change. Another goal of OBSSR is to enhance the interdisciplinary training of the current and next generation of behavioral and social scientists.
A critical milestone for enhancing interdisciplinary science and systems science is the rapid deployment of various components of cyber-infrastructure, making connectivity possible from the local to the global scale.29,30 The National Science Foundation's landmark Atkins report30 enumerates the potential and the critical base technologies underlying cyber-infrastructure, including the integrated electro-optical components of computation, storage, and communication that continue to advance in raw capacity at exponential rates. Above the cyber-infrastructure layer are the software programs, services, instruments, data, information, knowledge, and social practices applicable to specific projects, disciplines, and communities of practice. Between these two layers is the cyber-infrastructure layer of enabling hardware, algorithms, software, communications, institutions, and personnel. This layer should provide an effective and efficient platform for the empowerment of specific communities of researchers to innovate and eventually revolutionize what they do, how they do it, and who participates.
The next section elaborates on the programmatic directions outlined above, and includes specific research examples.
Programmatic Direction #1. Next-Generation Basic Science
Basic biomedical, behavioral, and social sciences research has produced enormous advances in understanding the factors that contribute to the risk of disease and to optimal health. Genetic studies in the 20th Century revealed mutations in individual genes responsible for a relatively small number of rare diseases, like Duchenne muscular dystrophy, cystic fibrosis, and sickle cell disease. The sequencing of the human genome and the completion of the HapMap have opened the door to genomewide association studies that will accelerate the identification of genetic contributions to health and disease. Simultaneously, advances in molecular and cellular biology, bioinformatics, and imaging are providing a rich, systems-biology view of cellular, organ, and organismal physiology, all of which will improve understanding of the etiology of disease and the ability to manage it.
At the same time, OBSSR recognizes that behavioral factors and social conditions have profound effects on the development and progression of common chronic diseases, premature disability, and mortality. Humans are both agents of change and affected by the process of change over time. This reciprocal determinism31 is a dynamic process and is often nonlinear, multi-determined, and multilevel in nature. Patterns of behavior, exposures to pathogens, and the social and physical built environments are rapidly changing as a result of human agency. For example, tobacco use, diet, physical activity, obesity, and HIV/AIDS have all changed dramatically within the relatively short period of 1 or 2 decades during the 20th Century. Many changes in lifestyle and living conditions have had large impacts on subgroups of the population and on the absolute rates of disease burden within the whole population. On the positive side, from 1900 to 2004, the U.S. population witnessed a dramatic increase in life expectancy, from 47.3 years to 77.8 years, due primarily to changes in life circumstances and, more recently, due to improvements in health care.32 On the negative side, between 1976–1980 and 2003–2004, the prevalence of obesity—a risk factor for type 2 diabetes, heart disease, cancer, and other serious health problems—rose dramatically. Obesity more than doubled in adults (from 15% to 34%), while overweight in children also more than doubled during this period (from 7% to 19% in ages 6–11), and overweight more than tripled in adolescents (from 5% to 17% in ages 12–19).32 Moreover, persistent problems like tobacco use and disparities in health remain as leading causes of preventable disease burden, disability, and death.
An enormous scientific challenge now presents itself: What are the best ways to understand, prevent, and treat common, chronic diseases like heart disease, cancer, addiction, and mental illness when it is apparent that they are the result of interactions between individuals—in all their biological complexity—and their ever-changing physical, behavioral, and social environments? To maximally improve population health, the individual's genome and biology must be viewed in its much broader environment. Human genetic sequences are static, but the functional expression of that DNA sequence is influenced by the environment. To begin unraveling this complexity, NIH launched its Genes, Environment and Health initiative33 and the Genetic Association Information Network.34 These trans-NIH efforts seek to identify how gene–environment interactions contribute to common diseases by supporting genomewide association studies to link particular genetic variants to specific diseases and the development of environmental and biomarker-sensor technologies to measure behavioral and chemical exposures.
These activities are an excellent start, but significant challenges remain. The massive amounts of genetic and exposure data that will be collected will make sense only with improved basic behavioral and social sciences research, which can address questions such as these: How should statistical power calculations and the interpretation of significant versus spurious associations be handled when so many variables can now be explored simultaneously? What is the best way to measure human phenotypes and the intermediate phenotypes that underlie complex clinical disease categories? What are the health-relevant physical, behavioral, and social environments, and how should these environmental exposures be measured over an entire lifespan? How can true gene–environment interactions be captured, and what are the mechanisms underlying these interactions?35How might environments be changed so that they foster, instead of assail, health?
The above considerations, as well as others, have led OBSSR to the following research priority areas in next-generation basic behavioral and social sciences research:
Gene–environment interactions
How do genetic endowment and early-life experiences interact to determine physical and mental health later in life? How do behavioral, social, chemical, and physical environments cause epigenomic changes that, in turn, influence gene expression?
Environmental effects on physiology
How is psychosocial stress transduced into a biological signal that influences physiology? Can these findings be used to understand group behavior in the context of trauma such as natural or man-made disasters? Or can they be used to elucidate mechanisms underlying the deleterious effects of impoverished environments on health? How do large-scale societal structures (e.g., racial segregation, immigration and acculturation patterns, economic discrimination) affect physiology and, ultimately, health?
Technology, measurement, and methodology
How can the rapid establishment of cyber-infrastructure, grid computing, and recent advancements in computer sciences, informatics, imaging, networking, and knowledge management be harnessed to improve data collection and analysis? How can the development of new tools and methodologies be improved so that they measure more precisely and directly behavior and social environments in real time (e.g., ecologic momentary assessment, personal sensors, geospatial coding methods) and decipher multilevel pathways linking biology, behavior, environment, and societal trends?
Social integration and social capital
How do advances in technology and mobility affect neighborhood social networks and mechanisms such as resilience and connectedness? What is the impact of these advances on health behaviors?
Complex adaptive systems
How can the growing understanding of complex adaptive systems be used to better understand the process of decision making in health at the personal and systems levels?
Social movements and policy change
How do social movements related to health take shape and permit things like tobacco taxes, smoke-free workplace policies, and school lunch program changes to occur? How and why must public opinion change before legislative, regulatory, or other legal action is possible? What science will enable researchers to frame messages in ways that maximize the chances for motivating and sustaining positive, health-related change?
Investigators are beginning to address these questions. For example, Caspi and Moffitt36 have been at the forefront of studies linking gene–environment interactions to psychiatric disorders in humans. Using data from the longitudinal Dunedin cohort study, they demonstrated that a particular, functional polymorphism in the promoter region of the serotonin transporter gene moderates the depressogenic influence of stressful life events during childhood. They reported that childhood maltreatment predicted adult depression only among individuals carrying the short allele genotype, but not among individuals carrying two copies of the long allele. Notably, the genotype did not predict adult depression.37 These data illustrate that the social environment during childhood interacts with genetics to influence adult behavior and disease.
The biological pathways underlying gene–social environment interactions are being explored as well. Meaney, Szyf, and colleagues38,39 have completed an elegant series of studies elucidating the mechanisms underlying the long-term effects of rat maternal behavior on the behavioral and neuroendocrine stress responses of their offspring. They have reported that a particular style of maternal behavior (low maternal rat-pup licking and arched-back nursing) during the first week of postnatal life leads to increased and prolonged reactivity of the hypothalamic–pituitary–adrenal (HPA) axis in the offspring. These changes are associated with reduced glucocorticoid receptor-gene expression in the hippocampi of the offspring, which appears to be due to epigenetic changes (increased DNA methylation, altered histone acetylation) in the promoter region of the glucocorticoid receptor gene. Central infusion of the histone deacetylase inhibitor, trichostatin A, to the offspring during adulthood reverses the previously defined differences in histone acetylation, DNA methylation, glucocorticoid-receptor expression, and HPA axis responses to stress, thus suggesting a causal relationship between patterns of maternal care and the epigenomic state, glucocorticoid-receptor expression, and stress responses in the offspring. While the extent to which these findings might generalize to other instances of behavioral and environmental programming remains to be determined, these findings do suggest that an epigenetic mechanism may underlie the transmission of intergenerational effects of a behavioral stimulus—one that is potentially reversible but can have dramatic downstream consequences (heightened neuroendocrine response to stress) across the offspring's lifetime.
Thus, there is enormous potential for greater understanding of gene–environment interactions and health through interdisciplinary partnerships among the behavioral and social sciences and the biomedical sciences as the field of epigenetics/epigenomics emerges. To support work at this leading edge of discovery, NIH has recently launched its NIH Roadmap Epigenomics Program40 as part of the NIH Roadmap. Among the goals of the NIH Roadmap Epigenomics Program are the following: (1) to coordinate and develop a series of reference epigenome maps, analogous to genome maps, which will be publicly available to facilitate research in human health and disease; (2) to evaluate the epigenetic mechanisms in aging, development, environmental exposure (including physical and chemical exposures), behavioral and social environments, and modifiers of stress; and (3) to develop new technologies for the epigenetic analysis of single cells and the imaging of epigenetic activity in living organisms.
Programmatic Direction #2. Interdisciplinary Research
The staff at OBSSR recognize that solving the most pressing health problems will require a greater understanding of the full range of factors that determine health—biological, behavioral, social, and environmental—and of their complex interrelationships. In some instances, a single research discipline is best suited to tackle specific health problems. However, most common, serious, health problems cannot be adequately addressed solely within a single discipline, instead requiring a more comprehensive approach. New discoveries and innovative solutions may become possible when researchers in different disciplines meet at the interfaces and frontiers of those disciplines to pool their diverse bodies of knowledge. Interdisciplinary research and education are inspired by the drive to solve complex questions and problems, whether generated by scientific curiosity or by pressing social need. Over time, collaboration among diverse scientists may shift from multidisciplinary and interdisciplinary work to a full transdisciplinary synthesis that has the potential to produce new disciplines, as in psychoneuroimmunology, cognitive and social neurosciences, and behavioral genetics.
Research on stress and cancer is an excellent example of interdisciplinary research involving the behavioral and biomedical sciences. Antoni et al.41 recently integrated a number of biomedical, behavioral, and clinical studies into a proposed mechanistic cascade underlying the links among behavior, biology, and cancer. Evidence is accumulating to suggest that stress, depression, and lack of social support influence the risk of cancer. For example, the breakup of a marriage has been associated with a twofold increase in the risk of breast cancer,42 and long-term chronic depression appears to increase general cancer risks.43,44 Basic research in physiology established a long time ago that the stress response is characterized by the activation of the sympatho-adrenal system, which releases the catecholamines, epinephrine, and norepinephrine, and the HPA axis, which releases glucocorticoids. More recently, animal models have shown that catecholamines, glucocorticoids, and other stress hormones influence multiple aspects of the tumor microenvironment, including: (1) the alteration of numerous aspects of immune function, (2) the promotion of tumor cell growth, (3) the migration and invasive capacity of cancer cells, (4) the stimulation of angiogenesis by the induction of pro-angiogenic cytokine production, and (5) the activation of oncogenic viruses (Figure 2).41
Figure 2.
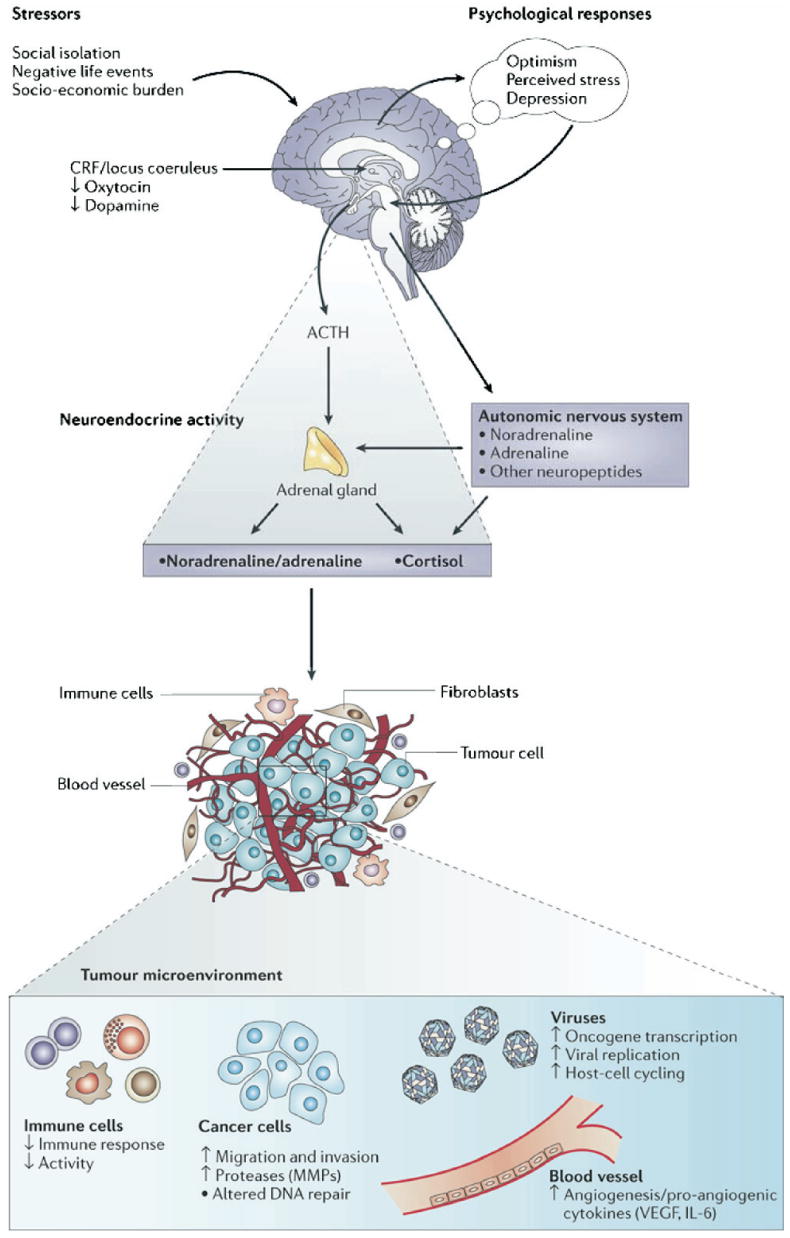
Effects of stress-associated factors on the tumor microenvironment
Reprinted with permission from Antoni et al.41
Moreover, recent studies have shown that the pharmacologic blockade of noradrenergic β receptors prevents the exacerbation of cancer that is otherwise observed following immobilization stress in mice, an indication that β-adrenergic signaling is critical in mediating the effects of stress on tumor growth in this model.45 Some comparable data in humans are beginning to emerge. For example, it has been demonstrated that norepinephrine upregulates vascular endothelial growth factor, which, in turn, stimulates angiogenesis in two human ovarian cancer cell lines.46 This catecholamine also increases human colon cancer–cell migration, and both epinephrine and norepinephrine promote the invasion of ovarian cancer cells in vitro. Taken together, data such as these indicate that a complex matrix of psychological, social, and biological factors in cancer, ranging from social isolation to viral infection, affects known physiological processes that influence cancer progression. Continued research in this area may yield targeted interventions to influence behavior, biology, or both to reduce the burden of cancer.
Programmatic Direction #3. Systems Science and Health
The term systems science is used here to refer to bringing to problem solving a perspective in which the problem space is conceptualized as a system of interrelated component parts (i.e., the “big picture”). This term was chosen in lieu of several others that may be synonymous, such as systems thinking or complexity, because some terms are associated with a particular “brand” of thought, and the authors feel that systems science is neutral while also inclusive. The system is viewed as a coherent whole, while the relationships among the components are also recognized and seen as critical to the system, for they give rise to the emergent properties of the system. Emergent properties are those properties that can only be seen at the system level and are not attributes of the individual components themselves (e.g., a flock emerges when a group of birds flies together; it is a property of the system, not of any individual bird). Systems science offers insights into the nature of the whole system that often cannot be gained by studying the component parts in isolation. Moreover, in a systems approach, there is recognition that embedded in the system are feedback loops, stocks and flows, that change over time (i.e., dynamic, nonlinear, complexity of the system).
The advantages of utilizing systems science as a complementary method for addressing complex problems include the fact that nonlinear relationships, the unintended effects of intervening in the system, and time-delayed effects are often missed with traditional reductionist approaches, whereas systems approaches excel at detecting these. The common conceptual orientation that defines a systems approach can be summarized as follows:
a paradigm or perspective that considers connections among different components, plans for the implications of their interaction, and requires transdisciplinary thinking as well as active engagement of those who have a stake in the outcome to govern the course of change.25
Systems science is not a single discipline; rather, it is a linkage of disciplines to bring about problem understanding and solving under the paradigm described above.
Systems science does not refer to a single methodology; rather, it encompasses a wide range of methods and tools (e.g., system dynamics simulation, agent-based modeling, network analysis, Markov modeling, soft-systems analysis, discrete-event modeling). While technology is used to maximize the effectiveness of systems approaches, systems science is not a technology. For an in-depth introduction to this topic, readers are encouraged to view webcasts of the 2007 Symposia Series on Systems Science and Health.47
By embracing systems science, the research community will be better equipped to handle the policy-resistant problems that abound in public health. Policy resistance refers to the “tendency for interventions to be defeated by the system's response to the intervention itself.” 21 In the last decades of the 20th Century, almost in parallel to the developments that spawned systems biology, the social–ecologic model emerged as a dominant world view in searching for explanations of the broader population-level causes of the very same common, chronic diseases that are the focus of biomedicine today.48–51
Other troubling causes of poor health and shortened life expectancy, such as access to care and disparities and inequality in healthcare delivery, have also been studied. The population, behavioral, and social sciences advanced beyond single discipline and simple causal views toward another valid systems view of understanding health and disease. In this world view, human behavior can be broadly defined as hierarchically organized along levels of complexity, from individual behavior to collective behavioral patterns within groups to higher levels of the clustering of patterns of behavior that are embodied in neighborhoods, worksites, schools, communities, cultural, ethnic, or religious affiliations, to even broader patterns determined by societal norms, financial incentives, and policies. These higher-order levels of factors interact in complex, dynamic, and multifactorial ways to produce the so-called “causes of the causes” of the complex common, chronic diseases.2 In this ecologic perspective, the view of the ultimate “causes of the causes” lies as much in the behavioral–social–ecologic environment as it does in the proximal biological environment evident through reductionist approaches.
The implication of these disparate world views of causation (biomedical and ecologic) calls for a broader integration of the disciplines than has occurred to date. OBSSR's view is that there should be a “macro” integration of the three broad disciplinary domains: the largely biomedical sciences, the largely individual behavioral sciences, and the largely group or population-level sciences of the ecologic world view.
Recently there has been a call for a new integrative vision among the behavioral, social, and public health sciences that might loosely be termed systems socio-behavioral science, systems medicine, or, as one author has put it, populomics.52 This is being called vertical integration, that is, integration across rather than within the three broad domains (i.e., the biomedical; the individual behavioral [intra-individual variation]; and the population [inter-individual or cluster variation] levels) of systems structure.20 The hope is that this type of vertical synthesis across varying levels of analysis will lead to a next generation of science enabling further breakthroughs in the understanding and reduction of the burden and suffering of the major common, chronic diseases that afflict the U.S., other developed nations, and, increasingly, the developing nations. OBSSR's call for systems science is a call for an increasingly global perspective on the interaction, connectivity, and relationships within and across nations. The specific objectives for OBSSR with regard to systems science are:
To facilitate the development and application of the conceptual frameworks and tools needed for the application of systems methodologies to problems of health and its determinants;
To promote and support the development of informatics tools to facilitate the collaboration and dissemination of data relevant to the behavioral, population, and social sciences (e.g., longitudinal epigenetic, biomarker, social, and behavioral data related to health);
To contribute to the development of analytical frameworks, methods, and algorithms capable of integrating, analyzing, and interpreting highly diverse data with varying metrics from research on genomic sequences, molecules, behavior, and social systems;
To collaborate in the development of the curricula, modules, and materials required to train health scientists in the application of systems science; and
To encourage the application of systems-organizing principles among stakeholder organizations in behavioral and social sciences research, and to promote the development of systems-organizing expertise among leaders, policymakers, and researchers.
Bringing systems science to bear on public health problems has the potential to explain how small changes at the individual level accumulate at the population level to reveal significant shifts in the absolute causes of disease.2,3 System dynamics modeling and agent-based models are methods that can simulate the complex relationships among the components of a system and emergent behavior—that is, behavior that is observed at the bird's-eye vantage point of the system emerging from the behavior of the individual components of the system (e.g., blood clotting and scab formation emerge at the systems level from the behavior of individual cells). Because of its unique ability to consider simultaneously both the whole system and its individual parts, systems science is capable of producing solutions that take into account a broad range of factors pertinent to the problem under consideration; for instance, genetic-to-environmental–, cellular-to-behavioral–, and biological-to-social–systems approaches have proven extremely valuable when applied to problems identified in a variety of disciplines, including defense,53 business,54 and cellular biology.55,56 Systems science shows promise for unlocking the secrets of complex, multidimensional health issues and for transforming this knowledge into effective interventions that can fundamentally change population health.57
An example of applying systems science to public health problems is illustrated by Jones et al.,58 who used system dynamics simulation modeling to explain type 2 diabetes prevalence since 1980 and to predict possible futures through 2050. The conceptual model (Figure 3) divided the U.S. population into those who do not have diabetes (normal glycemic levels); those at high risk for developing type 2 diabetes (i.e., people with prediabetes, divided into diagnosed and undiagnosed); and those who meet diagnostic criteria for type 2 diabetes (diagnosed and undiagnosed, subdivided into with and without medical complications from diabetes). The conceptual model included births (entry into the system); deaths (exit from the system); and individual members' movements among the diagnostic categories over time (stocks and flows), as well as numerous factors contributing to diabetes outcomes (e.g., clinical management of diabetes, self-monitoring, healthy-lifestyle adoption, and medication use).
Figure 3.
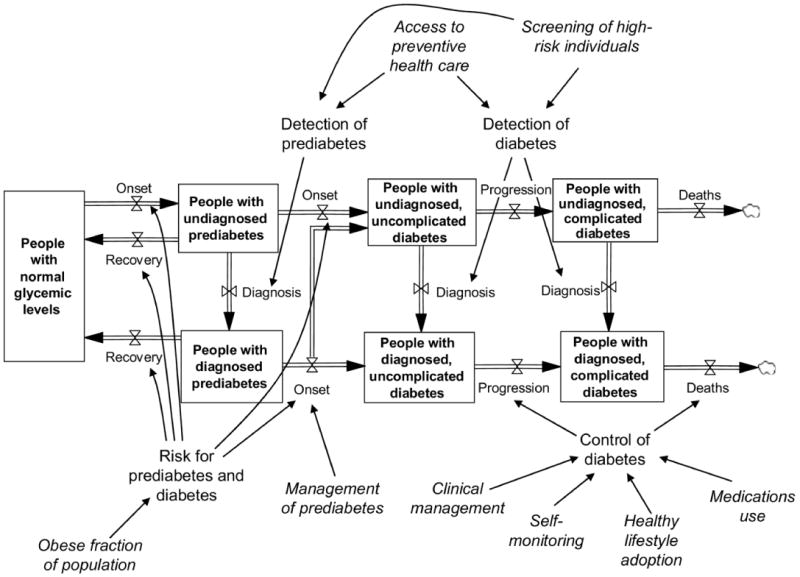
Diabetes conceptual model
Reprinted with permission from the American Public Health Association58
The relationships among all of these variables were quantified and the model was calibrated and validated in an iterative process using historical data from a variety of sources (e.g., the U.S. Census Bureau, the National Health Interview Survey, the National Health and Nutrition Examination Survey, and the Behavioral Risk Factor Surveillance System).
Simulations were then generated according to a variety of assumptions that were programmed into the model via algorithms. Figure 4 shows the results of the simulated population burden of diabetes (i.e., deaths) under various scenarios where an intervention is introduced that is designed to: (1) improve the clinical management of those diagnosed with diabetes; (2) improve pre-diabetes management; and (3) prevent diabetes (through the prevention of obesity). These three hypothetical scenarios are compared to “baseline,” a predictive model in which the status quo of diabetes clinical practices and prevention activities is maintained at baseline levels.
Figure 4.
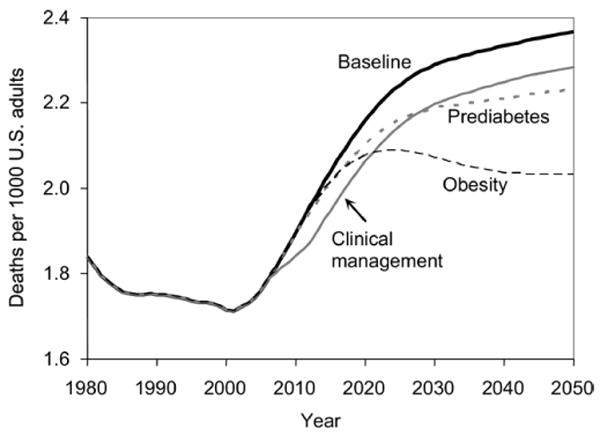
Model output for three intervention scenarios compared with the baseline scenario for diabetes complication-related deaths
Reprinted with permission from the American Public Health Association59
The following outcomes were predicted under each of the three scenarios:
The improved clinical management of diabetes leads to short-term improvements in diabetes control, complications, and associated deaths. However, following these improvements in the first few years, there is a rapid rise in complication deaths. Improvements in complications are rapidly overtaken by the growth in diabetes prevalence because nothing has been done to reduce diabetes onset.
Efforts to manage persons with prediabetes would lead to reductions in the onset of diabetes initially, and ultimately would reduce deaths from diabetes complications. But without prediabetes prevention efforts, the amount of reduction in deaths is less than optimal.
Finally, the primary prevention of diabetes shows the most drastic and lasting reductions in deaths.
However, even this powerful step alone (i.e., reducing rates of obesity without concurrent changes in prediabetes management or clinical diabetes management) would not reduce the overall burden of diabetes in terms of both the number of unhealthy days (not pictured) and the number of deaths due to diabetes right away (Figure 4). In fact, the number of deaths attributable to diabetes would actually rise through at least the year 2020, although during subsequent decades, a significant decrease in diabetes prevalence and deaths would occur. Thus, the time perspective is vital to determining the value of a strategy—that is, disease management works in the short term, but primary prevention is more effective in the long term. This example illustrates the potential of systems science to inform healthcare and policy decisions to improve population health.
In another example of adopting a systems approach to improving the understanding of a public health problem, Levy and colleagues developed SimSmoke,59 a simulation model for guiding policy to make a population impact on reducing smoking prevalence. SimSmoke uses historical and current data to model the multiple sources and complex interrelationships that determine tobacco-use prevalence and its health effects. A discrete-time dynamic model was developed that simulated smoking prevalence and tobacco-related deaths over a 40-year period. The model employed a first-order Markov process that modeled population growth and age-based rates of tobacco initiation, cessation, and relapse. This model simulated the impact of five policy-level interventions on smoking prevalence: taxes, clean indoor-air laws, strategies to reduce youth access to cigarettes, strategies to promote cessation treatments, and mass-media policies. Researchers used empirical and predicted data for the effects of each of these areas on model parameters. SimSmoke showed the relative contributions made by a variety of different policy interventions (i.e., increasing cigarette prices, introducing smoking bans, introducing media campaigns to encourage cessation and prevention, implementing additional restrictions on youth access to tobacco, and introducing proactive quitlines) toward the desired outcomes (i.e., reduction in smoking prevalence and reduction in deaths attributable to tobacco). Such models can be used to inform decisions about how best to allocate financial resources and formulate policies to optimize a desired public health impact. The focus is on making an efficient population impact to address a complex societal problem (tobacco-use behavior) with an emphasis on outcomes and on multiple causal pathways, feedback loops, and control-systems dynamics that underlie the way the tobacco industry and the public health constituencies vie for their respective goals.
The above examples illustrate the potential for systems science to radically transform the behavioral, social, and population sciences to a degree similar in magnitude to the transformation that systems biology and bioinformatics are now bringing about in biology. This sentiment is captured in the broad vision for cyber-infrastructure outlined in the Atkins report of the National Science Foundation30:
The opportunity is here to create cyberinfrastructure that enables more ubiquitous, comprehensive knowledge environments that become functionally complete for specific research communities in terms of people, data, information, tools, and instruments and that include unprecedented capacity for computational, storage, and communication…. They can serve individuals, teams and organizations in ways that revolutionize what they can do, how they do it, and who participates.
Programmatic Direction #4. Population Impact
The North Karelia Project60 underscores the value of a multimodal, problem-based approach to a major public health issue. In the 1960s, Finnish men had the world's highest rate of heart disease mortality. The death rate was especially high in the province of North Karelia, a rural area in the eastern part of Finland. In 1972 officials in North Karelia began a community-based initiative to reduce cardiovascular disease and mortality. The North Karelia project included: (1) cultural interventions addressing traditional Finnish dietary norms to reduce fat intake and to double the consumption of fruits and vegetables; (2) media outreach, including health-related news features, educational content, and a national “quit and win” contest; (3) the training of healthcare providers to provide cardiovascular risk-factor assessment and counseling for all patients; (4) the engagement of community leaders and workplaces to spearhead health-promotional activities; and (5) policy interventions that included public smoking bans, the elimination of tobacco advertising, and taxes earmarked for tobacco control programs.
A variety of research disciplines, including social psychology, nutrition science, marketing, education, primary care medicine, policy, and tobacco control were brought together to design this multilevel intervention. The results were impressive: By the early 2000s, the number of deaths of working-age Finnish men from coronary heart disease had plummeted 75%. In North Karelia, the effects were even more pronounced (an 82% reduction in deaths), and life expectancy for men increased 7 years. Much of this reduction in mortality came from reductions in risk factors like high blood pressure, high cholesterol, and smoking, because of nutritional changes and smoking cessation. Today, this project continues to sustain itself with a modest level of public resources.
Another problem with tremendous population impact is that of health disparities. If this problem were widely addressed, enormous benefit could be conferred on those affected by these inequalities. Transdisciplinary and systems science perspectives may be valuable approaches for addressing health disparities and inequality.22 These approaches permit researchers in the field to step back and consider the ways that their science has been framed by historical, disciplinary perspectives (i.e., a focus on intra-individual, molecular, genetic “causes” within biomedical frames of reference versus a focus on the socioeconomic forces and the levels of socio-environmental context, such as social position and poverty, as the “causes of the causes” within ecologic frameworks). For example, a recent study used county-level geospatial and racial-group coding to categorize into clusters the population of the U.S. according to expected longevity; these clusters are called the “Eight Americas.”61 An incredible gap of 35 years of life expectancy was reported between the highest and lowest life-expectancy ranks among the eight clusters. The lowest cluster is grouped among nations of the world with the lowest life expectancy (sub-Saharan Africa and Russia) and can be viewed as excluded from the gains made in average life expectancy in the U.S. during the entire 20th Century. Life expectancy in the cluster at the high end of the Eight Americas exceeds that of nations whose life expectancy is the highest in the world (3 years better than Japan for females and 4 years better than Iceland for males).
Abrams22 suggests a new framework for integrating historically disparate frames of reference from individual and population sciences into a new synthesis. This framework would embrace a model of genes and the social and physical environments in a complex, nonlinear, reciprocal interaction of risk and protective factors, over the lifespan and across generations.2,20,39,62 Interdisciplinary research and systems science can perhaps clarify the extent to which gene–environment interactions account for racial and ethnic health disparities and improve the development of effective interventions and policies to eliminate those disparities.63
These brief examples are but a few of an increasing number of approaches that use a problem-focused, outcomes-oriented goal to strengthen the science of dissemination, implementation, and policy research. The hope is that a deeper understanding of the basic mechanisms in complex adaptive systems will help to improve the design of the next generation of interventions and lead to better (i.e., informed by science) health policies. Such approaches use the tools of basic and applied interdisciplinary science; systems science; and problem-focused, outcomes-oriented strategies to maximize their public health impact.
New Directions at NIH in Support of Interdisciplinary, Translational, and Systems Sciences
Although OBSSR does not have grant-making authority, it partners with NIH institutes and centers to develop research initiatives, alternately playing a lead or participatory role. Since 2003, OBSSR has led the development of a number of trans-NIH initiatives under the auspices of the NIH Roadmap. The three themes of the NIH Roadmap are New Pathways to Discovery, Research Teams of the Future, and Re-Engineering the Clinical Research Enterprise.
Interdisciplinary research, one of the components of the Research Teams of the Future theme, has included several initiatives specifically targeting the behavioral and social sciences. The OBSSR-led initiatives Supplements for Methodological Innovations in the Behavioral and Social Sciences (RFA RM-04-013)64 and Meetings and Networks for Methodological Development in Interdisciplinary Research (RFA RM-04-014)65 supported research on dietary intake, physical activity, child development, stress–immune interactions, environmental exposures, treatment decision making, patient quality of life, gene–environment interactions, pain, and aging. Seven postdoctoral institutional-training grants were awarded under another NIH Roadmap initiative, Interdisciplinary Health Research Training: Behavior, Environment and Biology (RFA RM-05-010).66 These programs provide formal coursework and research training in a new interdisciplinary field for individuals holding advanced degrees in a different discipline. The Exploratory Centers for Interdisciplinary Research (RFA RM-04-004)67 program is supporting the centers that are investigating cognition, elder self-neglect, or youth vulnerability to sexually transmitted infections and unintended pregnancies. Another center focuses on the pathways through which the environment, genetic, and psychosocial domains jointly shape child health and well-being. A 2007 initiative, Facilitating Interdisciplinary Research via Methodological and Technological Innovation in the Behavioral and Social Sciences (RFA RM-07-004),68 supports the development of new and innovative measures, methods, and technologies that underlie the interdisciplinary integration of human social science, behavioral science, or both, with other disciplines across varying levels of analysis. Links to descriptions of the projects funded under these and other interdisciplinary NIH Roadmap initiatives can be found on the NIH Roadmap website (www.nihroadmap.nih.gov/interdisciplinary/fundedresearch.asp).
Finally, one of the initiatives developed under the Re-Engineering the Clinical Research Enterprise theme is the Institutional Clinical and Translational Science Award (CTSA; RFA RM-08-002).69 CTSAs are cooperative agreements to provide resources and develop methodologies to overcome blocks at both the discovery (translation between bench and bedside) and implementation (translation between bedside and practice and community) steps. Translational research has two components: (1) applying discoveries generated during research in the laboratory and in preclinical studies to the development of trials and other human studies, and (2) research aimed at enhancing the adoption of best practices in the community. This second component of translation, that is, the science of dissemination and implementation of best practices, requires strong behavioral and social sciences research.
Framework for the Future: Office of Portfolio Analysis and Strategic Initiatives (OPASI)
The NIH Roadmap is now administered by the Office of Portfolio Analysis and Strategic Initiatives70 (OPASI), a new office within the Office of the Director of NIH. OPASI has several related missions, including the development of methods to help the agency analyze and manage its portfolio; the gathering and analysis of data on the public health burden to help set priorities; and the evaluation of the outcomes of NIH-funded activities. A major purpose of OPASI is to provide an incubator space, in the form of NIH Roadmap initiatives, to accelerate critical research efforts that address major, cross-cutting NIH priorities. The general intent of OPASI is consistent with the concept of systems science across NIH and the identification of new opportunities that cut across disciplines and across different levels (from cells to society) as well as the fostering of research that will reduce the public health burden—all of which is also consistent with the mission and vision of OBSSR.
Conclusion
The sciences concerned with optimal health, well-being, and disease management have revealed just how broad the future world view needs to be. At the end of the day, the simple, single-cause, single-discipline, and now, even single-level-of-analysis models—whether predominantly biomedical or predominantly behavioral or social–ecologic—are increasingly viewed as necessary but insufficient. This is especially true for the common, most preventable, and most expensive chronic diseases that afflict the vast majority of populations in the developed nations of the world and that cry out for research to provide a more timely understanding of basic mechanisms, better interventions, and more science-informed health policy. The biomedical, reductionist world view of the causes of disease and the behavioral, social–ecologic world view of the “causes of the causes” of disease are really two sides of the same coin that must be merged to develop a new synthesis and a more complete and useful heuristic framework to guide future research.
Systems science, cyber-infrastructure, and new technology may well provide the foundation stones to facilitate OBSSR's strategic vision: an integration of next-generation basic science with its applications to clinical practice, community dissemination, and health policy; a vertical integration from cells to society and a progression from interdisciplinary science to a deeper set of transdisciplinary conceptual syntheses; and an ability to examine nonlinear causal loops and solutions using backward engineering of the complex causal pathways, starting from a defined problem or pressing public health challenge (like eliminating health disparities; reversing the epidemics of obesity, sedentary lifestyle, and type 2 diabetes; and further reducing tobacco use and the incidence HIV/AIDS). In the final analysis, the mission of basic and applied science at OBSSR and across the NIH embraces a problem-focused, outcomes-oriented set of goals to make a timely and cost-efficient impact on improving the nation's health and reducing the absolute burden of disease and disability at the individual and population levels.
Acknowledgments
The authors would like to thank Bobby Milstein, PhD, at the CDC for his inspiration and education on systems science, which is reflected in this work. They are grateful for his unwavering support and partnership with OBSSR on systems science initiatives.
The authors would also like to thank the reviewers of the manuscript for this paper. While the reviewers are unknown, the authors believe the reveiwers' feedback helped strengthen this paper.
Footnotes
Publisher's Disclaimer: This PDF receipt will only be used as the basis for generating PubMed Central (PMC) documents. PMC documents will be made available for review after conversion (approx. 2-3 weeks time). Any corrections that need to be made will be done at that time. No materials will be released to PMC without the approval of an author. Only the PMC documents will appear on PubMed Central -- this PDF Receipt will not appear on PubMed Central.
No financial disclosures were reported by the authors of this paper.
References
- 1.The Office of Behavioral and Social Sciences Research, NIH. The contributions of behavioral and social sciences research to improving the health of the nation: a prospectus for the future. 2007 http://obssr.od.nih.gov/Content/Strategic_Planning/Strategic+Plan_2007/ObssrIndex.htm.
- 2.McKinlay JB, Marceau LD. To boldly go…. Am J Public Health. 2000;90:25–33. doi: 10.2105/ajph.90.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rose G. The strategy of preventive medicine. New York: Oxford University Press; 1992. [Google Scholar]
- 4.Stokols D, Hall KL, Taylor BK, Moser RP. The science of team science: overview of the field and introduction to the supplement. Am J Prev Med. 2008;35(2S):S77–S89. doi: 10.1016/j.amepre.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Rosenfield PL. The potential of transdisciplinary research for sustaining and extending linkages between the health and social sciences. Soc Sci Med. 1992;35:1343–57. doi: 10.1016/0277-9536(92)90038-r. [DOI] [PubMed] [Google Scholar]
- 6.NIH. NIH roadmap for medical research. www.nihroadmap.nih.gov.
- 7.Thun MJ, Jemal A. How much of the decrease in cancer death rates in the U.S is attributable to reductions in tobacco smoking? Tob Control. 2006;15:345–7. doi: 10.1136/tc.2006.017749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Centers for Health Statistics. National Health Interview Survey (NHIS) Hyattsville MD: CDC; 1965. [Google Scholar]
- 9.CDC. Cigarette smoking among adults—U.S., 2006. MMWR Morb Mortal Wkly Rep. 2007;56:1157–61. [PubMed] [Google Scholar]
- 10.Warner KE. Effects of the antismoking campaign: an update. Am J Public Health. 1989;79:144–51. doi: 10.2105/ajph.79.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Warner KE. Tobacco policy research: insights and contributions to public health policy. In: Warner KE, editor. Tobacco control policy. San Francisco: Jossey-Bass; 2006. [Google Scholar]
- 12.IOM. Ending the tobacco problem: a blueprint for the nation. Washington DC: National Academies Press; 2007. [Google Scholar]
- 13.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 15.March JS, Silva S, Petrycki S, et al. The treatment for adolescents with depression study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64:1132–43. doi: 10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]; Arch Gen Psychiatry. 2008;65:101. Erratum. [Google Scholar]
- 16.CDC. Twenty-five years of HIV/AIDS—U.S., 1981–2006. MMWR Morb Mortal Wkly Rep. 2006;55:585–9. [PubMed] [Google Scholar]
- 17.CDC. Evolution of HIV/AIDS prevention programs—U.S., 1981–2006. MMWR Morb Mortal Wkly Rep. 2006;55:597–603. [PubMed] [Google Scholar]
- 18.CDC. Epidemiology of HIV/AIDS—United States, 1981–2005. MMWR Morb Mortal Wkly Rep. 2006;55:589–92. [PubMed] [Google Scholar]
- 19.Haynes RB, Yao X, Degani A, Kripalani S, Garg A, McDonald HP. Interventions to enhance medication adherence. Cochrane Database Syst Rev. 2005;(4):CD000011. doi: 10.1002/14651858.CD000011.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62:1650–71. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 21.Sterman J. Learning from evidence in a complex world. Am J Public Health. 2006;96:505–14. doi: 10.2105/AJPH.2005.066043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abrams DB. Applying transdisciplinary research strategies to understanding and eliminating health disparities. Health Educ Behav. 2006;33:515–31. doi: 10.1177/1090198106287732. [DOI] [PubMed] [Google Scholar]
- 23.Anderson NB. Levels of analysis in health science: a framework for integrating sociobehavioral and biomedical research. In: McCann S, Lipton JM, editors. Annals of the New York Academy of Sciences. Vol. 840. New York: New York Academy of Sciences; 1998. [DOI] [PubMed] [Google Scholar]
- 24.Kessel F, Rosenfield PL, Anderson NB, editors. Expanding the boundaries of health and social science. New York: Oxford University Press; 2003. [Google Scholar]
- 25.Leischow S, Milstein B. Systems thinking and modeling for public health practice. Am J Public Health. 2006;96:403–4. doi: 10.2105/AJPH.2005.082842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Homer JB, Hirsch GB. System dynamics modeling for public health: background and opportunities. Am J Public Health. 2006;96:452–8. doi: 10.2105/AJPH.2005.062059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glasgow R, Green L, Klesges L, et al. External validity: we need to do more. Ann Behav Med. 2006;31:105–8. doi: 10.1207/s15324796abm3102_1. [DOI] [PubMed] [Google Scholar]
- 28.Kerner J, Rimer B, Emmons K. Introduction to the special section on dissemination: dissemination research and research dissemination: how can we close the gap? Health Psychol. 2005;24:443–6. doi: 10.1037/0278-6133.24.5.443. [DOI] [PubMed] [Google Scholar]
- 29.Bertenthal B. Cyberinfrastructure for the social and behavioral sciences. Psychological Science Agenda. 2005;19:2–4. [Google Scholar]
- 30.Atkins DE, Droegemeier KK, Feldman SI, et al. Revolutionizing science and engineering through cyberinfrastructure: report of the National Science Foundation Blue-Ribbon Advisory Panel on Cyberinfrastructure. Washington DC: National Science Foundation; 2003. [Google Scholar]
- 31.Bandura A. Social foundations of thought and action: a social-cognitive theory. Upper Saddle River NJ: Prentice-Hall; 1986. [Google Scholar]
- 32.National Center for Health Statistics. Health, US, 2006 With chartbook on trends in the health of Americans. Hyattsville MD: The Center; 2006. [PubMed] [Google Scholar]
- 33.NIH. The genes, environment and health initiative (GEI) www.gei.nih.gov/index.asp.
- 34.NIH. Genetic association information network (GAIN) www.genome.gov/19518664.
- 35.Committee on Assessing Interactions Among Social, Behavioral, and Genetic Factors in Health. Genes, behavior, and the social environment: moving beyond the nature/nurture debate. In: Hernandez LM, Blazer DG, editors. Washington DC: National Academies Press; 2006. www.nap.edu/catalog/11693.html. [PubMed] [Google Scholar]
- 36.Caspi A, Moffitt TE. Gene-environment interactions in psychiatry: joining forces with neuroscience. Nat Rev Neurosci. 2006;7:583–90. doi: 10.1038/nrn1925. [DOI] [PubMed] [Google Scholar]
- 37.Caspi A, Sugden K, Moffitt TE. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–9. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 38.Meaney MJ, Szyf M. Environmental programming of stress responses through DNA methylation: life at the interface between a dynamic environment and a fixed genome. Dialogues Clin Neurosci. 2005;7:103–23. doi: 10.31887/DCNS.2005.7.2/mmeaney. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Szyf M, Weaver IC, Champagne FA, Diorio J, Meaney MJ. Maternal programming of steroid receptor expression and phenotype through DNA methylation in the rat. Front Neuroendocrinol. 2005;26(3–4):139–62. doi: 10.1016/j.yfrne.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 40.NIH. NIH roadmap for medical research: epigenomics: an overview. nihroadmap.nih.gov/epigenomics.
- 41.Antoni MH, Lutgendorf SK, Cole SW, et al. The influence of bio-behavioural factors on tumour biology: pathways and mechanisms. Nature. 2006;6:240–8. doi: 10.1038/nrc1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lillberg K, Verkasalo PK, Kaprio J, Teppo L, Helenius H, Koskenvuo M. Stressful life events and risk of breast cancer in 10,808 women: a cohort study. Am J Epidemiol. 2003;157:415–23. doi: 10.1093/aje/kwg002. [DOI] [PubMed] [Google Scholar]
- 43.Reiche EM, Nunes SO, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncology. 2004;5:617–25. doi: 10.1016/S1470-2045(04)01597-9. [DOI] [PubMed] [Google Scholar]
- 44.Spiegel D, Giese-Davis J. Depression and cancer: mechanisms and disease progression. Biol Psychiatry. 2003;54:269–82. doi: 10.1016/s0006-3223(03)00566-3. [DOI] [PubMed] [Google Scholar]
- 45.Thaker PH, Han LY, Kamat AA, et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nature Medicine. 2006;12:939–44. doi: 10.1038/nm1447. [DOI] [PubMed] [Google Scholar]
- 46.Lutgendorf SK, Cole S, Costanzo E, et al. Stress-related mediators stimulate vascular endothelial growth factor secretion by two ovarian cancer cell lines. Clin Cancer Res. 2003;9:4514–21. [PubMed] [Google Scholar]
- 47.NIH. Office of Behavioral and Social Sciences Research. 2007 symposia series on systems science and health. obssr.od.nih.gov/Content/Lectures+and+Seminars/Systems_Symposia_Series/SEMINARS.htm.
- 48.Cohen DA, Scribner RA, Farley TA. A structural model of health behavior: a pragmatic approach to explain and influence health behaviors at the population level. Prev Med. 2000;30:146–54. doi: 10.1006/pmed.1999.0609. [DOI] [PubMed] [Google Scholar]
- 49.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 50.Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. Am Psychol. 1992;47:6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 51.Green LW, Richard L, Potvin L. Ecological foundations of health promotion. Am J Health Promot. 1996;10:270–81. doi: 10.4278/0890-1171-10.4.270. [DOI] [PubMed] [Google Scholar]
- 52.Gibbons MC. A historical overview of health disparities and the potential of eHealth solutions. J Med Internet Res. 2005;7:e50. doi: 10.2196/jmir.7.5.e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Krygiel AJ. Behind the wizard's curtain: an integration environment for a system of systems. Washington DC: National Defense University Press; 1999. [Google Scholar]
- 54.Senge PM. The fifth discipline: the art and practice of the learning organization. New York: Doubleday Dell Publishing Group, Inc.; 1994. [Google Scholar]
- 55.Weston AD, Hood L. Systems biology, proteomics, and the future of health care: toward predictive, preventative, and personalized medicine. J Proteome Res. 2004;3:179–96. doi: 10.1021/pr0499693. [DOI] [PubMed] [Google Scholar]
- 56.Grimm V, Revilla E, Berger U, et al. Pattern-oriented modeling of agent-based complex systems: lessons from ecology. Science. 2005;310:987–91. doi: 10.1126/science.1116681. [DOI] [PubMed] [Google Scholar]
- 57.Trochim WM, Cabrera DA, Milstein B, Gallagher RS, Leischow SJ. Practical challenges of systems thinking and modeling in public health. Am J Public Health. 2006;96:538–46. doi: 10.2105/AJPH.2005.066001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jones AP, Homer JB, Murphy DL, Essien JD, Milstein B, Seville DA. Understanding diabetes population dynamics through simulation modeling and experimentation. Am J Public Health. 2006;96:488–94. doi: 10.2105/AJPH.2005.063529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Levy DT, Ross H, Powell L, Bauer JE, Lee HR. The role of public policies in reducing smoking prevalence and deaths caused by smoking in Arizona: results from the Arizona tobacco policy simulation model. Public Health Manag Pract. 2007;13:59–67. doi: 10.1097/00124784-200701000-00010. [DOI] [PubMed] [Google Scholar]
- 60.Puska P. The North Karelia Project: 20 year results and experiences. Helsinki: National Public Health Institute; 1995. [Google Scholar]
- 61.Murray CJL, Kulkarni SC, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the U.S. PLoS Med. 2006;3:e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of U.S. socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95:312–23. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Anderson NB, Nickerson KJ. Genes, race, and psychology in the genome era: an introduction. Am Psychol. 2005;60:5–8. doi: 10.1037/0003-066X.60.1.5. [DOI] [PubMed] [Google Scholar]
- 64.NIH. Supplements for methodological innovations in the behavioral and social sciences (RFA RM-04-013) grants.nih.gov/grants/guide/rfa-files/RFA-RM-04-013.html.
- 65.NIH. Meetings and networks for methodological development in interdisciplinary research (RFA RM-04-014) grants.nih.gov/grants/guide/rfa-files/RFA-RM-04-014.html.
- 66.NIH. Interdisciplinary health research training: behavior, environment and biology (RFA RM-05-010) grants.nih.gov/grants/guide/rfa-files/RFA-RM-05-010.html.
- 67.NIH. Exploratory centers for interdisciplinary research (RFA RM-04-004) grants.nih.gov/grants/guide/rfa-files/RFA-RM-04-004.html.
- 68.NIH. Facilitating interdisciplinary research via methodological and technological innovation in the behavioral and social sciences (RFA RM-07-004) grants.nih.gov/grants/guide/rfa-files/RFA-RM-07-004.html.
- 69.NIH. Institutional Clinical and Translational Science Award (CTSA; RFA RM-08-002) grants.nih.gov/grants/guide/rfa-files/RFA-RM-08-002.html.
- 70.Office of Portfolio Analysis and Strategic Initiatives. 2007 http://opasi.nih.gov.


