Abstract
Objective:
While much is now known about depression during school age and adolescence, whether clinical depression can onset even earlier in development during the preschool period remains under explored. The earliest possible identification of depression may be important for the design of prevention and early developmental intervention programs. This study investigated functional impairment associated with depression, symptoms that served as the best markers of depression vs. other disorders, as well as depression severity between two depressed sub-groups and other diagnostic comparison groups.
Method:
Three hundred and five preschoolers between the ages of 3.0 and 6.0 and their primary caregivers were recruited using a depression screening checklist distributed at community sites. The Preschool Age Psychiatric Assessment (PAPA) was used to derive psychiatric diagnoses in the study sample. Multivariate analyses of covariance were used to investigate the effects of depression on independent measures of functional impairment while controlling for the effects of co-morbidities.
Results:
Functional impairment specifically associated with depression was found in multiple domains and contexts, however depressed preschoolers were not developmentally delayed. The symptoms of guilt and extreme fatigue were found to be highly specific for preschool depression. A statistically significant hierarchy of depression severity was found between diagnostic comparison groups, in the expected direction with the highest in a melancholic subgroup.
Conclusions:
Validation for preschool depression with associated functional impairment across contexts was found in preschool children. These findings replicate and extend earlier evidence for validity of MDD diagnosed in the preschool period and highlight the need for clinical attention. The finding that these depressed and impaired preschoolers were not yet developmentally delayed may have important public health significant significance as it suggests a possible window of opportunity for early intervention. Study findings were limited by reliance on parent and teacher informants and a cross-sectional view.
Keywords: Preschool, Depression, Validation, Impairment, Markers
1. Introduction
Contrary to historical developmental theory, recent empirical evidence has suggested that a clinically significant depressive disorder can arise in children as young as 3 years of age (Luby et al., 2002, 2003a,b; Egger and Angold, 2006). Kashani and colleagues were the first to systematically explore the issue of preschool depression and found substantial numbers of preschoolers with numerous “concerning symptoms” but who fell short of meeting formal DSM-III MDD criteria (Kashani and Ray, 1983; Kashani and Carlson, 1985; Kashani et al., 1986). These studies suggested that developmental adjustments to depressive symptom criteria should be explored (Kashani et al., 1997).
Evidence for a specific and stable depressive symptom constellation was subsequently found in a sample of preschoolers recruited from primary care and mental health clinics (Luby et al., 2002). Preschoolers who met all DSM-IV MDD symptom criteria were identified based on parent report on a developmentally appropriate, structured psychiatric interview (Luby et al., 2003a,b). The symptom of anhedonia emerged as a highly specific symptom of depression and as a marker of a more severe and putative “melancholic” subtype, strikingly similar to that known in depressed adults (Luby et al., 2004a,b). While these markers of validity were limited by their basis on parent report of depressive symptoms, objective observational evidence of depressive behaviors during play was also found (Luby et al., 2004a,b). Alterations in stress cortisol reactivity were found, providing evidence for biological correlates of preschool depression, as established in depressed adults (Luby et al., 2003a,b; Carroll et al., 1976). These findings demonstrated that the preschool disorder was characterized by age adjusted clinical features similar to those known in the adult disorder providing empirical evidence for basic continuity of depressive disorders across the lifespan.
While these data provided evidence for clinically significant preschool depression, the need for replication of these findings in larger independent samples as well as an investigation of functional impairment was needed. Impairment was determined to be key to clarifying the nosology of preschool depression based on the fact that impairment (or distress) is a prerequisite to clinical “caseness” defined by the DSM system. However, the measurement of impairment during the preschool period is complicated by the fact that preschoolers do not spend significant amounts of time in structured settings in which “work” or the standard definition of “productivity” is required. Another issue is that preschoolers' functioning is inextricably tied to the child–caregiver relationship and thus to their caregivers' competence (Carter et al., 2004).
Based on the need to address questions raised by the available findings, and the availability of novel, reliable and developmentally appropriate measures of psychopathology and impairment for preschool aged children, an investigation of the characteristics of preschool onset depression in a large sample of 3–6 year old children ascertained from community sites was initiated.
2. Method
2.1. Participants and procedure
Preschoolers between 3 and 6 years of age were recruited from sites throughout the Saint Louis area for participation in a study examining the nosology of preschool depression. Recruitment was done through primary care practices, and preschools/daycares that were accessible to the general community in an effort to increase the socioeconomic and ethnic diversity of the sample. Recruitment sites were chosen at random using a geographically stratified method.
The aim of this sampling technique was to recruit a large group of depressed preschoolers as well as smaller groups of disruptive and healthy preschoolers for comparison. To achieve this goal, a validated screening checklist, The Preschool Feelings Checklist (PFC) (Luby et al., 1999) was completed by caregivers. Previous studies have indicated that a PFC score of >3 maintained high sensitivity and specificity for the diagnosis of depression. In addition to identifying and including children with high symptom sum scores, children with low or no endorsed symptoms were also recruited in order to establish an adequate healthy comparison group.
Approximately 6000 checklists were distributed to sites between May 2003 and March 2005. In daycares and preschools, from which approximately 3/4 of sample was ascertained, checklists were handed out to all parents of children in the target age range. Checklists were made available in waiting areas of primary care settings next to a poster describing a study of early emotion development. Completed checklists were collected by the sites and returned. Using this method, N=1474 checklists were returned and those with scores of 0 (presumed healthy) or >3 (above established cut-off) were sought for participation. Among those returned N=335 were ineligible due to being out of the age range and N=240 had PFC scores out of range. The remaining N=899 met all initial screening and inclusion criteria and were contacted by phone for further screening. Based on phone screening, subjects with chronic illness, marked speech and language delays and/or neurologic or Autistic Spectrum Disorders were excluded. Those without exclusions (N=416) were invited for study participation and N=305 agreed and presented for the assessment. Based on this screening technique, it is not possible to accurately estimate the prevalence rate of preschool depression with these data.
Preschoolers and their caregivers participated in a 3–4 hour laboratory assessment during which primary caregivers (92% biological mothers) were interviewed about their child's behaviors, emotions, psychiatric symptoms and impairments. The child participated in a battery of cognitive, developmental and observational assessments. All study procedures were pre-approved by the institutional review board of Washington University in St. Louis.
2.2. Measures
2.2.1. Diagnostic assessment
All diagnostic modules of the Preschool Age Psychiatric Assessment (PAPA) (Egger et al., 2003) were used to establish DSM-IV diagnoses. The PAPA is an interviewer based diagnostic assessment with empirically established test re-test reliability designed for use in caregivers of children aged 2.0–6.0 (Egger et al., 2006). A trained interviewer administered the PAPA at baseline, which was audio taped for later quality control and group calibration, the established method to maintain inter-rater reliability. The PAPA covers a broad range of psychiatric symptoms and impairment/disability from symptoms. In addition to generating categorical MDD diagnosis (using a DSM-IV computer algorithm), depression severity scores were created by summing all PAPA depression items. This dimensional measure of depression has previously been demonstrated to be a sensitive measure of depression severity (Luby et al., 2004a,b).
2.2.2. Impairment
The Preschool and Early Childhood Functional Assessment Scale (PECFAS) (Hodges, 1994) was used as an independent measure of preschoolers' functional impairment. The PECFAS is an interviewer rated measure with favorable psychometric properties that assesses the psychosocial functioning and impairment of children between the ages of 3.0 and 7.11 (Murphy et al., 1999). All interviewers were certified as reliable in PECFAS administration and coding through training and testing developed by the authors of the measure. The PECFAS measures impairment across the following domains: School/Daycare, Home, Community, Behavior toward others, Moods/Emotions, Self-harmful behavior, and Thinking. The PECFAS aims to assess impairment from symptoms in these domains rather than symptoms themselves and is rated by a certified interviewer based on the parent's description of the child's functioning. Two additional scales rate the caregiver's ability to provide for the child's material and emotional needs, an important source of impairment in a young child.
The Vineland Adaptive Behavior Scale is a widely used, valid and reliable developmental measure with established standardized norms (Sparrow et al., 1987). It was used in this investigation to assess preschoolers' developmental skills/impairments.
The Health and Behavior Questionnaire (HBQ) (Essex et al., 2002) was also used to assess preschoolers' functioning in multiple domains as directly rated by parents (HBQ-P) and preschool teachers or daycare staff (HBQ-T). The HBQ is a reliable and valid dimensional caregiver report symptom assessment with parent and teacher versions designed for young children (Essex et al., 2002). Among several domains the HBQ measures social and school adaptation.
PAPA Disability/Impairment Module
In this module, parents were asked whether their child's symptoms significantly and negatively impact the child's relationships with others. The severity of two types of impairment: “withdrawal” or “discord” was rated by the interviewer based on parental report.
2.2.3. Statistical analysis
Univariate and bivariate methods were used to perform preliminary analyses on demographic characteristics and co-morbidity in the study sample. Chi-square tests were used to compare demographic characteristics between diagnostic groups. Due to high rates of co-morbidity in the sample, multivariate analyses of covariance (MANCOVAs) were conducted to examine associations between depression and 7 functional impairment subscale scores (PECFAS), 2 HBQ-P impairment scores and 4 Vineland subscale scores. A univariate analysis of covariance (ANCOVA) was used for the HBQ-T impairment domain. The effects of age, gender and co-morbidity were controlled in these multivariate analyses.
A series of analyses were conducted to investigate the utility of each symptom of depression as a specific marker of the disorder. To account for the effects of co-morbidity, binary logistic regression analyses were conducted using the 10 core DSM-IV MDD symptoms as outcome variables and dummy coded diagnostic variables as predictor variables. This tested whether having a MDD diagnosis significantly increased the likelihood of having specific MDD symptoms after accounting for co-morbid disruptive disorders (yes/no) and/or anxiety disorders (yes/no). In addition, in order to test the specificity of each symptom as a marker of depression compared to anxiety and/or disruptive disorders, multinomial logistic regressions (MLR) were conducted in non co-morbid sub-groups. The above analyses allowed a contrast of the odds ratio for having a diagnosis of MDD vs. healthy to the odd's ratios of being anxious vs. healthy and disruptive vs. healthy. This method was deemed more appropriate and informative than binary logistic regressions in which each disorder would only be contrasted with the healthy group.
A univariate analysis of variance (ANOVA) and subsequent post hoc tests were conducted to examine differences in depression severity between diagnostic groups. A univariate analysis of covariance (ANCOVA) was then used to examine the association between preschoolers' depression severity scores and their MDD diagnosis after controlling for co-morbidity. SPSS 15.0 was used for all analyses except SAS 9.1 was used to conduct exact logistic regressions.
3. Results
3.1. Diagnostic characteristics of study sample
An ethnically diverse sample, similar to the composition of the St. Louis area was ascertained. From N=305 caregiver–child participants at baseline, n=3 subjects were excluded from the analyses due to excessive missing data. Preschoolers who fell into one of four diagnostic groups of interest, based on application of DSM-IV computer algorithms to parent report on the PAPA, were included in the following analyses. Seventy-five preschoolers who met DSM-IV symptom criteria for MDD were identified. In analyses examining depression severity, the depressed group was divided into two sub-groups, one characterized by the symptom of anhedonia and presumed to have a melancholic subtype n=39 (52% of depressed group) and the other met criteria for MDD without anhedonia n=36 (48%). A group who met criteria for a DSM-IV anxiety disorder n=39 (without co-morbid depression) was identified n=30 Separation Anxiety Disorder (SAD) n =10 Generalized Anxiety Disorder (GAD), n=4 Post Traumatic Stress Disorder (PTSD), n=5 participants had >1 anxiety disorder. Seventy-one preschoolers with anxiety disorders were identified when those with co-morbid depression were included. Preschoolers who met all DSM-IV criteria for Attention Deficit Hyperactivity Disorder (ADHD, n=17), and/or Oppositional Defiant Disorder (ODD, n=27) and/or Conduct Disorder (CD, n=10) were identified and labeled the “disruptive” group (n=40). Healthy preschoolers (n=146) were also included. Two children who met criteria for Bipolar I (BP-1) only were excluded. Results indicated that depressed preschoolers were significantly older than children in the healthy and disruptive groups. No other diagnostic group differences in relation to demographic variables were found.
3.1.1. Co-morbidity
Thirty-five percent of depressed preschoolers had co-morbid ADHD, 51% had co-morbid ODD and 27% had co-morbid CD. Forty-three percent of depressed preschoolers also had at least one co-morbid anxiety disorder. Specifically, 13% of depressed preschoolers met criteria for GAD and 32% met SAD criteria. Thirty-three percent of preschoolers in the anxiety group had a co-morbid disruptive disorder. There were n=32 preschoolers with anxiety disorders (GAD, SAD or PTSD) who also had MDD. There were no differences in the total number of co-morbidities associated with any of the specific disorders studied.
3.2. Functional impairment
A one-way MANCOVA was conducted to examine the effect of MDD on functional impairment when controlling for the effects of age, gender, disruptive, and anxiety disorders. Significant differences were found between preschoolers with and without MDD in all 7 PECFAS impairment domains [Wilks' λ=.808; F(7, 250)=8.50; p<0.001; eta2=.192]. Further, across shared and independent effects, MDD explained approximately 19% of the variance in PECFAS impairment scores. The univariate comparisons showed that with only one exception (thinking/communication domain), preschoolers with MDD had significantly higher impairment scores on all PECFAS domains compared to those without MDD (Table 1).
Table 1.
Preschoolers' PECFAS impairment scores and univariate comparisons
| PECFAS impairment scores |
With MDD (n=66) |
Without MDD (n=196) |
F(1,256) | P-value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| School/Daycare domain | 9.70 | 10.52 | 2.70 | 6.35 | 9.98 | 0.002 |
| Home role performance domain | 14.85 | 8.81 | 7.45 | 7.75 | 8.02 | 0.005 |
| Community role performance domain | 3.33 | 6.64 | 0.36 | 2.35 | 9.53 | 0.002 |
| Behavior toward others domain | 13.79 | 7.80 | 6.99 | 7.55 | 6.89 | 0.009 |
| Moods/Emotions domain | 14.39 | 6.59 | 5.87 | 6.70 | 33.68 | <0.001 |
| Self harming behaviors domain | 4.85 | 8.27 | 0.26 | 1.58 | 30.91 | <0.001 |
| Thinking/Communication domain | 1.82 | 5.24 | 0.36 | 2.12 | 2.36 | 0.126 |
3.2.1. HBQ-P impairment
A one-way MANCOVA was conducted to compare two HBQ-P impairment scores for preschoolers with or without depression. After controlling for age, gender, co-morbid anxiety and/or disruptive disorder(s), significant differences between depressed and non-depressed preschoolers' HBQ-P impairment [Wilks' λ=.941; F(2, 271)=8.48; p>0.001; eta2=.059]. Univariate comparisons showed that preschoolers with MDD had significantly higher impairment scores in both HBQ-P domains (Table 2).
Table 2.
Preschoolers' impairment scores and univariate comparisons from health and behavior questionnaire–parent report
| HBQ impairment scores |
With MDD (n=73) |
Without MDD (n=205) |
F(1,272) | P-value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| ‘Self’ domain | 0.52 | 0.35 | 0.23 | 0.29 | 13.67 | <0.001 |
| ‘Family’ domain | 0.89 | 0.68 | 0.38 | 0.44 | 13.47 | <0.001 |
3.2.2. Daycare/Preschool teacher reported impairment (HBQ-T)
An ANCOVA was conducted to examine HBQ-T impairment score for preschoolers with or without depression. After controlling for age, gender, co-morbid anxiety and/or disruptive disorders, results showed that preschoolers with MDD had significantly higher HBQ-T impairment scores [F(1,196)=5.97; p=0.015; eta2=.030).
3.2.3. Vineland
A one-way MANCOVA was conducted to compare preschoolers' standard scores on the four subscales of the Vineland in relation to MDD vs. non-MDD diagnosis. No significant differences were found on Vineland subscale scores in relation to depression diagnosis.
3.2.4. PAPA impairment
A logistic regression was conducted to compare PAPA impairment scores for depressed vs. non-depressed preschoolers. Results showed that preschoolers with MDD were approximately twice as likely to be impaired compared with preschoolers without MDD after controlling for the presence of co-morbid anxiety and/or disruptive diagnoses [Odds ratio=2.13, 95% CI (1.05, 4.28)].
3.3. Specificity of symptoms as markers of MDD
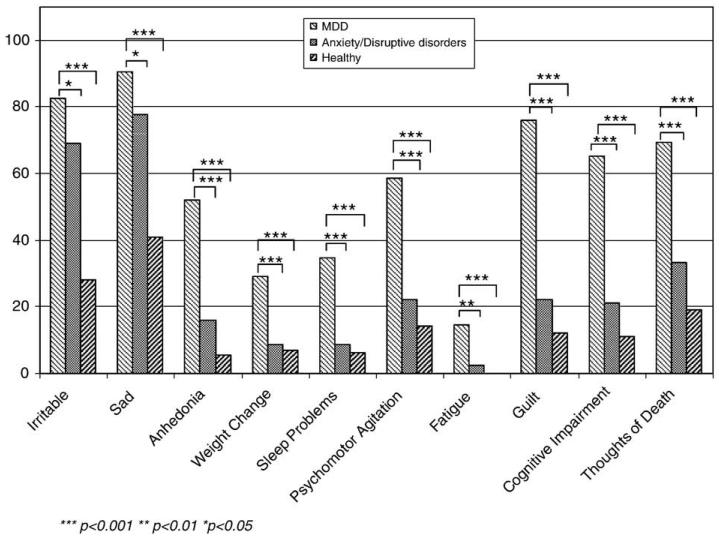
The frequencies of 10 depression symptoms were compared among depressed, disruptive, anxious and healthy preschoolers. As shown in Fig. 1, preschoolers in the MDD group had a significantly greater likelihood of having all MDD symptoms compared to healthy preschoolers as well as those with other psychiatric disorders.
Fig. 1.
Frequency of PAPA MDD symptoms across 3 groups.
To account for the high co-morbidity rates in the current sample, binary logistic regression analyses were conducted using the 10 core DSM-IV MDD symptoms as seen in Fig. 1. Each depression symptom was regressed on three diagnoses (i.e., MDD, disruptive and anxiety). The partial odds ratios for the MDD diagnoses are reported in Table 3. All ten odds ratios for MDD were statistically significant, indicating that each symptom was strongly associated with MDD, even after controlling for depressed preschoolers co-morbid diagnoses.
Table 3.
Odds ratios for MDD diagnosis on MDD symptoms controlling for anxiety, disruptive disorders
| Irritable | Sad and/or tearful |
Anhedonia | Weight change |
Sleep problems |
Psychomotor agitation |
Fatigue | Guilt | Diminished cognitive abilities |
Thoughts of death |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety | 2.36** | 2.52* | 1.76 | 0.89 | 1.50 | 1.08 | 1.38 | 1.55 | 1.27 | 1.31 |
| Disruptive | 3.23*** | 3.39*** | 1.36 | 0.60 | 0.61 | 1.71 | 1.28 | 1.16 | 1.55 | 3.12*** |
| MDD | 4.03*** | 5.22*** | 8.39*** | 6.84*** | 7.56*** | 5.55*** | 15.93*** | 14.95*** | 9.32*** | 4.81*** |
p<0.001
p<0.01
p<0.05.
To further elucidate findings represented in Table 3, MLRs were also conducted on sub-samples of preschoolers without co-morbid disorders. The outcome variable had four categories (pure MDD, pure anxiety, pure disruptive, and healthy). Each MDD symptom was entered as a predictor variable, resulting in 10 total models. Table 4 displays the MLR odds ratios for each depression symptom. Each of these methods provided different but complementary information. For example, Table 3 indicated that if children were diagnosed with anxiety they were not significantly more likely to have anhedonia compared to any other group. However, as seen in Table 4, if children had anhedonia, they were 5 times more likely to be categorized as anxious than as healthy.
Table 4.
Multinomial logistic regressions' Odds ratios for MDD symptoms
| Pure MDD (n=20) vs. Healthy (n=146) |
Pure anxiety (n=26) vs. Healthy (n=146) |
Pure MDD (n=20) vs. Pure anxiety (n=26) |
Pure disruptive (n=38) vs. Healthy (n=146) |
Pure MDD (n=20) vs. Pure disruptive (n=38) |
|
|---|---|---|---|---|---|
| Irritable | 23.06*** | 4.84*** | 4.76 | 5.55*** | 4.15 |
| Sad and/or tearful | 12.90*** | 3.89** | 3.31 | 4.62*** | 2.79 |
| Anhedonia | 17.25*** | 5.18** | 3.33 | 2.61 | 6.60** |
| Weight change | 11.12*** | 2.47 | 4.50* | 0.76 | 14.72** |
| Sleep problems | 10.00*** | 2.73 | 3.67 | 0.41 | 24.68** |
| Psychomotor agitation | 7.28*** | 1.42 | 5.13* | 2.13 | 3.42* |
| Fatigue |
Infinite (Exact OR=30.40**) |
Infinite (Exact OR=5.54) |
4.41 | Infinite (Exact OR=3.79) |
6.53 |
| Guilt | 28.45*** | 2.13 | 13.33*** | 1.61 | 17.71*** |
| Diminished cognitive abilities | 12.18*** | 1.48 | 8.25** | 2.17 | 5.62** |
| Thoughts of death | 4.21** | 1.00 | 4.20* | 2.46* | 1.71 |
p<0.001
p<0.01
p<0.05.
As expected, the odds ratios for the MDD versus healthy group (see column 1) were larger than the odds ratios for MDD versus anxiety (column 3) and MDD versus disruptive (column 5) on most MDD symptoms with the exception of weight change and sleep problems. Odds ratios for the “extreme fatigue” symptom in the MDD versus healthy was infinite, due to the presence of a zero cell in the cross-tabulation (i.e., no healthy children had extreme fatigue). Since this zero is not a structural zero, exact logistic regression was used to obtain a finite estimate. Exact odds ratio for MDD versus healthy was 30.40 (p<.01).
Preschoolers in five diagnostic groups (including two depressed sub-groups as described above) were examined (see Fig. 2). Results indicated a main effect of diagnostic status on depression severity sum scores, F(4, 295)=139.78, p<.001. Post hoc tests using Scheffe corrections revealed that comparisons between diagnostic groups were significantly (p<.001) different from each other in relation to MDD severity with the exception that disruptive and anxious preschoolers did not differ significantly. The “melancholic” depressed subgroup demonstrated the highest depression severity. In addition, an ANCOVA was conducted to examine the association between preschoolers' depression severity scores and their MDD subgroup diagnosis after controlling for age, gender and co-morbidity. Results showed that preschoolers with melancholic MDD had significantly higher depression severity than preschoolers with non-melan-cholic MDD as well as preschoolers without MDD. The non-melancholic depressed subgroup demonstrated significantly higher depression severity than the non-MDD group (melancholic, X̄=10.41, SD=3.84, t=16.97, p<0.001; non-melancholic, X̄=7.11, SD=2.33, t=8.82, p<0.001; non-MDD, X̄=2.11, SD=2.00).
Fig. 2.
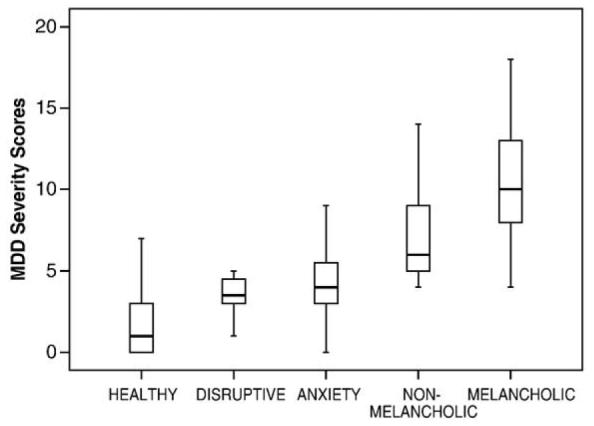
Comparison of MDD severity sum scores among 5 groups.
4. Discussion
These data replicate and extend earlier findings validating preschool depression from an independent study sample (Luby et al., 2002; Luby et al., 2003a,b). The rates of co-morbidity found are similar to those reported in depressed school age children (Angold and Costello, 1993). Findings of impairment in functioning specifically associated with depression in multiple domains and contexts, rated by both parents and teachers, underscores the clinical significance of this early onset syndrome. The fact that impairment was detected using several independent measures emphasizes the robust nature of this finding. Further, the finding of functional impairment without significant delays in basic development on the Vineland demonstrates that depressed and impaired preschoolers are not yet developmentally delayed, suggesting a window of opportunity for early intervention.
Odds ratios derived using MLR addressed the specific risk of each depressive symptom for MDD versus other disorders. Findings demonstrated that all symptoms of depression may serve as clinical markers in the general population, as their occurrence was associated with a four to twenty-eight times greater likelihood of being depressed compared to being healthy. Key symptoms that differentiated depressed from disruptive preschoolers were sleep problems, guilt, weight changes, anhedonia and diminished cognitive abilities. Key symptoms that differentiated depressed from anxious preschoolers were guilt, diminished cognitive abilities, psychomotor agitation and weight changes. Of particular note, extreme fatigue and guilt were highly specific to the depressed group when anxious and disruptive co-morbidities were controlled and therefore may be useful in clinical settings as pathognomonic markers of depression (see Table 3). As expected, the symptom of irritability was not useful to differentiate depression from other disorders. However, unexpected was the finding that sadness was also a relatively non-specific marker of depression compared to other disorders. In addition, anhedonia, while uncommon in anxiety disorders, did not emerge as a marker that could differentiate depression from anxiety.
A melancholic depressed sub-group, characterized by anhedonia, displayed the highest depression severity. This emerged within a statistically significant hierarchy of depression severity when depressed sub-groups were also compared to other disorders. This replicates earlier findings from a smaller independent sample (Luby et al., 2004a,b). The significant differences in depression severity between the depressed and anxiety groups further suggest that this symptom constellation represents a unique mood disorder and not simply more general internalizing phenomena. This stands in contrast to the hypothesis that young children would display more undifferentiated internalizing disorders rather that discrete DSM-IV disorders (Achenbach, 1995; Cole, 1997; Keenan and Wakschlag, 2002).
Findings from this study conducted in a screened sample of preschool children from community sites replicate and extend earlier findings from an independent study sample validating a preschool depressive disorder. Further study in a representative, population-based sample is needed to derive prevalence rates for preschool depression. Early indications that the pre-valence of preschool depression (2%) is comparable to that found in older children have been provided from a representative community sample (Egger and Angold, 2006). Reliance on diagnosis and ratings of impairment based on caregiver report is a limitation of the data presented. Investigations of performance based and/or objective observational measures of functioning are now needed. Another limitation was that the PAPA was not designed to assess BP-II or more subtle symptoms of bipolarity, thus we cannot rule out the possibility that additional subjects in the sample may have also had mixed depression or more subtle bipolar spectrum symptoms (Akiskal, 1995; Disalver et al., 2005).
These findings provide further validation for depression in preschoolers. The clinical significance of this early onset disorder is underscored by the finding of impairment in functioning associated with depression in numerous domains. Further, the finding of symptoms and impairments evident across contexts in a young child has been shown to support clinical significance based on longitudinal data in disruptive disorders (Campbell, 2002). The symptoms of guilt and extreme fatigue emerged as highly specific markers of depression strongly differentiating depressed preschoolers from those with anxiety and disruptive disorders and thus potentially useful as clinical markers. Replication of these findings at independent research sites is a critical next scientific step.
The identification of depression during the preschool period, even as early as 3 years of age could have important public health significance beyond its obvious implications for relieving the suffering of preschoolers and their families. The earliest possible identification and intervention in mental disorders during this period of rapid developmental and neurobiological change may represent a window of opportunity for more effective treatment. While this remains an empirically unexplored issue in the area of depression, the unique efficacy of earlier intervention has been established in other early onset psychiatric disorders (Boggs et al., 2004; Dawson et al., 2000; Eyberg et al., 2001; Faja and Dawson, 2006; Hood and Eyberg, 2003; Webster-Stratton and Reid, 2003). The possibility that earlier intervention could change the trajectory of this chronic and relapsing disorder remains an exciting possibility. Validation of preschool depression and the demonstration of significant associated impairment now provide the necessary evidence for future public attention to this early onset disorder and related testing of early intervention strategies.
Acknowledgments
We are grateful to The Early Emotional Development Program Staff, our preschool participants and their parents, and community recruiting sites whose participation and cooperation made this research possible.
Footnotes
Role of funding source
Funding for the study of preschool depression was provided by the NIMH grant NIMH R01 (MH64769-01) to Dr. Joan Luby, M.D. The NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Conflicts of interest
The authors have no conflicts of interest to disclose. All authors are affiliated with the Washington University School of Medicine in St. Louis.
References
- Achenbach TM. Empirically based assessment and taxonomy: applications to clinical research. Psychol. Assess. 1995;7:261–274. [Google Scholar]
- Akiskal HS. Developmental pathways to bipolarity: are juvenile-onset depressions pre-bipolar? J. Am. Acad. Child Adolesc. Psych. 1995;34:754–763. doi: 10.1097/00004583-199506000-00016. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello E. Depressive comorbidity in children and adolescents: empirical, theoretical and methodological issues. Am. J. Psychiatr. 1993;150:1779–1791. doi: 10.1176/ajp.150.12.1779. [DOI] [PubMed] [Google Scholar]
- Boggs S, Eyberg S, Edwards DL, Arista R, Jacobs J, Bagner D, Hood K. Outcomes of parent–child interaction therapy: a comparison of treatment completers and study dropouts one to three years later. Child Fam. Behav. Ther. 2004;26:1–22. [Google Scholar]
- Campbell S. Behavioral Problems in Preschool Children: Clinical and Developmental Issues. 2nd ed. Guilford Press; NY: 2002. [Google Scholar]
- Carroll BJ, Curtis GC, Mendels J. Neuroendocrine regulation in depression II: discrimination of depressed from non-depressed patients. Arch. Gen. Psychiatry. 1976;33:1051–1058. doi: 10.1001/archpsyc.1976.01770090041003. [DOI] [PubMed] [Google Scholar]
- Carter AS, Briggs-Gowan MJ, Davis N. Assessment of young children's social–emotional development and psychopathology: recent advances and recommendations for practice. J. Child Psychol. Psychiatry. 2004;45:109–134. doi: 10.1046/j.0021-9630.2003.00316.x. [DOI] [PubMed] [Google Scholar]
- Cole DA. Relation between symptoms of anxiety and depression in children: a multitrait–multimethod–multigroup assessment. J. Consult. Clin. Psychol. 1997;65:110–119. doi: 10.1037//0022-006x.65.1.110. [DOI] [PubMed] [Google Scholar]
- Dawson G, Ashman SB, Carver LJ. The role of early experience in shaping behavioral and brain development and its implications for social policy. Dev. Psychopathol. 2000;12:695–712. doi: 10.1017/s0954579400004089. [DOI] [PubMed] [Google Scholar]
- Disalver SC, Benazzi F, Akiskal HS. Mixed states: the most common outpatient presentation of bipolar depressed adolescents? Pschopathology. 2005;38:268–272. doi: 10.1159/000088443. [DOI] [PubMed] [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. J. Child Psychol. Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Egger HL, Ascher B, Angold A. The Preschool Age Psychiatric Assessment: Version 1.4. Center for Developmental Epidemiology, Department of Psychiatry and Behavioral Sciences. Duke University Medical Center; Durham, NC: 2003. [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter B, Angold A. Test–retest reliability of the Preschool Age Psychiatric Assessment (PAPA) J. Am. Acad. Child Adolesc. Psych. 2006;45:538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Essex MJ, Boyce WT, Goldstein LH, Armstrong JM, Kraemer HC, Kupfer DJ. The confluence of mental, physical, social, and academic difficulties in middle childhood II: developing the MacArthur Health and Behavior Questionnaire. J. Am. Acad. Child Adolesc. Psych. 2002;41:588–603. doi: 10.1097/00004583-200205000-00017. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Funderburk BW, Hembree-Kigin TL, McNeil CB, Querido JG, Hood KK. Parent–child interaction therapy with behavior problem children: one and two year maintenance of treatment effects in the family. Child Fam. Behav. Ther. 2001;23:1–20. [Google Scholar]
- Faja S, Dawson G. Early intervention for autism. In: Luby JL, editor. Handbook of Preschool Mental Health. Guilford Press; NY: 2006. pp. 388–416. [Google Scholar]
- Hodges K. The Preschool and Early Childhood Functional Assessment Scale (PECFAS) Department of Psychology, Eastern Michigan University; Ypsilanti, MI: 1994. [Google Scholar]
- Hood KK, Eyberg SM. Outcomes of parent–child interaction therapy: mothers' reports of maintenance three to six years after treatment. J. Clin. Child Adolesc. Psychol. 2003;32:419–429. doi: 10.1207/S15374424JCCP3203_10. [DOI] [PubMed] [Google Scholar]
- Kashani JH, Ray JS. Depressive related symptoms among preschool-age children. Child Psychiatry Hum. Dev. 1983;13:233–238. doi: 10.1007/BF00709557. [DOI] [PubMed] [Google Scholar]
- Kashani JH, Carlson GA. Major depressive disorder in a preschooler. J. Am. Acad. Child Psych. 1985;24:490–494. doi: 10.1016/s0002-7138(09)60570-7. [DOI] [PubMed] [Google Scholar]
- Kashani JH, Holcomb WR, Orvaschel H. Depression and depressive symptoms in preschool children from the general population. Am. J. Psychiatry. 1986;143:1138–1143. doi: 10.1176/ajp.143.9.1138. [DOI] [PubMed] [Google Scholar]
- Kashani J, Allan W, Beck N, Bledsoe Y, Reid J. Dysthymic disorder in clinically referred preschool children. J. Am. Acad. Child Psych. 1997;36:1426–1433. doi: 10.1097/00004583-199710000-00025. [DOI] [PubMed] [Google Scholar]
- Keenan K, Wakschlag LS. Can a valid diagnosis of disruptive behavior disorder be made in preschool children? Am. J. Psychiatr. 2002;159:351–358. doi: 10.1176/appi.ajp.159.3.351. [DOI] [PubMed] [Google Scholar]
- Luby JL, Heffelfinger A, Mrakotsky C, Hildebrand T. Preschool Feelings Checklist. Washington University; St. Louis, MO: 1999. [Google Scholar]
- Luby JL, Heffelfinger A, Mrakeotsky C, Hessler M, Brown K, Hildebrand T. Preschool major depressive disorder: preliminary validation for developmentally modified DSM-IV criteria. J. Am. Acad. Child Adolesc. Psych. 2002;41:928–937. doi: 10.1097/00004583-200208000-00011. [DOI] [PubMed] [Google Scholar]
- Luby JL, Heffelfinger A, Mrakotsky C, Brown K, Hessler M, Spitznagel E. Alterations in stress cortisol reactivity in depressed preschoolers relative to psychiatric and no-disorder comparison groups. Arch. Gen. Psychiatry. 2003a;60:1248–1255. doi: 10.1001/archpsyc.60.12.1248. [DOI] [PubMed] [Google Scholar]
- Luby JL, Heffelfinger AK, Mrakotsky C, Brown KM, Hessler MJ, Wallis JM, Spitznagel EL. The clinical picture of depression in preschool children. J. Am. Acad. Child Adolesc. Psych. 2003b;42:340–348. doi: 10.1097/00004583-200303000-00015. [DOI] [PubMed] [Google Scholar]
- Luby JL, Mrakotsky C, Heffelfinger A, Brown K, Spitznagel E. Characteristics of depressed preschoolers with and without anhedonia: evidence for a melancholic depressive subtype in young children. Am. J. Psychiatr. 2004a;161:1998–2004. doi: 10.1176/appi.ajp.161.11.1998. [DOI] [PubMed] [Google Scholar]
- Luby JL, Sullivan J, Belden A, Stalets M, Blankenship S, Spitznagel E. An observational analysis of behavior in depressed preschoolers: further validation of early onset depression. J. Am. Acad. Child Adolesc. Psych. 2004b;45:203–212. doi: 10.1097/01.chi.0000188894.54713.ee. [DOI] [PubMed] [Google Scholar]
- Murphy MJ, Ramirez A, Anaya Y, Nowlin C, Jellinek MS. Validation of the preschool and early childhood functional assessment. J. Child Fam. Stud. 1999;8:343–356. doi: 10.1023/A:1022071430660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow S, Carter AS, Cicchetti D. Overview, Reliability, Validity, Administration and Scoring. Department of Psychology, Yale University; New Haven, CT: 1987. Vineland Screener. [Google Scholar]
- Webster-Stratton C, Reid MJ. Treating conduct problems and strengthening social and emotional competence in young children: the Dina Dinosaur Treatment Program. J. Emot. Behav. Disord. 2003;11:130–143. [Google Scholar]