Abstract
The purpose of this study was to develop and conduct preliminary psychometric assessment of instruments measuring knowledge and self-care practices regarding behaviors needed for blood pressure (BP) control among African Americans. Items were empirically derived and scored on a 7-point, bipolar scale. The instruments were evaluated in a sample of 306 community-dwelling African Americans. Results revealed acceptable reliability and validity of the BP Knowledge Scale. Results for the BP Self-Care Scale were mixed. A structural equation model of these scales, recorded BP, and covariates fit well. There was an unexpected positive correlation between self-care and BP suggesting a potential bi-directional relationship. The scales demonstrated acceptable psychometric properties and, with minor revisions, may have clinical utility as measures of BP knowledge and self-care.
Keywords: Blood pressure, hypertension, African American, self-care, instrument development
Hypertension is a major public health problem affecting over 50 million Americans. Thirty percent of adults have the condition but are unaware of its presence, 40% of persons with hypertension are not being treated, and only one-third of those being treated have their blood pressure (BP) controlled to <140/90 (Chobanian et al., 2003). The risk of death from ischemic heart disease and stroke increases linearly and progressively from BP levels as low as 115 mmHg systolic and 75 mmHg diastolic (Lewington, Clarke, Qizilbash, Peto, & Collins, 2002), and the lifetime risk of developing hypertension is 90% for men and women who are normotensive at age 55 (Vasan et al., 2002). Given these data, it is imperative that efforts be directed at preventing and controlling BP disease. The need for hypertension prevention and control is greatest among African Americans, as their prevalence of hypertension is higher than any other racial or ethnic group in the United States (Centers for Disease Control [CDC,] 2005). Yet, little is known about African Americans’ knowledge and practice of the self-care behaviors necessary to prevent and control high BP. Therefore, the purpose of this study was to test the psychometric properties of instruments designed to measure both knowledge and frequency of engaging in the self-care behaviors necessary to control BP in a sample of African American adults.
The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7; Chobanian et al. 2003) identified a number of causal factors for hypertension, including: reduced physical activity, excess body weight, excess dietary sodium intake, inadequate intake of fruits and vegetables, and excessive alcohol intake. These causal factors can be mitigated through self-care strategies for lifestyle modification (Campbell et al., 1999; Chobanian et al.; Douglas et al., 2003).
Many of the disparities noted in the prevalence, morbidity, and mortality of hypertension in African Americans may be attributed to disparities in the presence of the identified causal risk factors (Douglas et al.). Racial disparities are noted in levels of physical activity. African American men and women are nearly two times as likely to be physically inactive as their Caucasian counterparts (Crespo, Smith, Andersen, Carter-Pokras, & Ainsworth, 2000), with two-thirds of African American women being physically inactive (Kruger, Yore, Solera, & Moeti, 2007). Disparities in weight also are noted, with the prevalence of both obesity and extreme obesity higher for African Americans than non-Hispanic Whites, and extreme obesity almost 2.5 times greater for African Americans (Ogden et al., 2006).
Dietary patterns also may put African Americans at increased risk of high BP. In addition to diets high in caloric intake, African Americans generally have diets that contain sodium in excess of physiological requirements (Jen, Brogan, Washington, Flack, & Artinian, 2007). This is an important risk factor, as habitual ingestion of high levels of dietary salt is associated with increased blood pressures (Cooper et al., 1997; Stamler, 1997). Salt-sensitivity, or greater BP variability in relation to sodium ingestion, is an important factor in the development of hypertension, and 73% of hypertensive African Americans are considered to be salt-sensitive (Svetkey, Chen, McKeown, Preis, & Wilson, 1997). Researchers have demonstrated dramatic declines in BP for both normotensive and hypertensive persons who reduced their dietary salt, with African Americans demonstrating the greatest reduction in BP (Sacks et al, 2001). Research results also provide evidence that an eating plan that emphasizes fruits and vegetables will reduce BP, yet, three-quarters of African American men and women do not eat the recommended five fruits and vegetable servings per day (Kruger et al., 2007). Although similar to other racial groups, 22% of African Americans smoke (CDC, 2006) and 13% are considered to be moderate to heavy drinkers, thereby increasing their risk of elevated BP and other cardiovascular problems (Schoenborn & Adams, 2002).
A number of investigators have shown a relationship between stress and elevated BP, but without conclusive evidence for a causal relationship (Chobanian et al., 2003). Although stress reduction is not specified in the JNC 7 guidelines, research conducted with African Americans shows significant decreases in both systolic (SBP) and diastolic blood pressure (DBP) at 3 months after a behavioral stress management intervention (Alexander et al., 1996), with additional evidence that stress reduction techniques can reduce BP for up to 12 months (Spence, Barnett, Linden, Ramsden, & Taenzer, 1999).
Although African Americans have a disproportionately high risk and burden of hypertension, little is known about their knowledge of self-care behaviors that can prevent and control high BP. In addition, no research was found on the pattern of knowledge and self-care of any group regarding the totality of the self-care behaviors necessary to keep BP within normal limits. Therefore, the purpose of this study was to describe the development and initial validation of quantitative instruments to measure participants’ knowledge regarding all of the recognized self-care behaviors necessary for controlling blood pressure, as well as to measure the degree to which all of these self-care behaviors were being performed.
Conceptual Framework
The conceptual framework used for this study was the self-care deficit nursing theory (SCDNT; Orem, 2001). Within the SCDNT, self-care is a human regulatory function, deliberately engaged in by a person in order to maintain structural integrity and human functioning for health and overall well-being (Orem, p. 45). In the current study the regulatory function of interest was blood pressure control. Self-care refers to behaviors that are learned according to the beliefs, habits, and practices that characterize the person’s cultural way of life. The self-care behaviors produced are a result of a person’s self-care agency or ability. Engaging in a self-care behavior starts with the estimative operations of self-care agency. These operations involve persons having sufficient knowledge about the courses of action required to achieve the desired outcome. In addition, estimative operations require the person to have knowledge of themselves and their beliefs about the effectiveness and desirability of those actions (Orem, p. 275). With this knowledge, persons make judgments and decisions (transitional operations) about the course of action they will take. These decisions are reflected in the actual self-care behaviors produced. Consistent with the SCDNT, it was hypothesized that increased knowledge of factors that can control BP will lead to increased BP self-care behaviors resulting in increased BP control (i.e., BP within normal limits).
Development of the Blood Pressure Self-Care and Knowledge Scales
According to the JNC guidelines, seven self-care behaviors are required to control BP. Because no instrument could be found that measured the totality of the behaviors necessary for BP control, a new instrument, the Blood Pressure Self-Care Scale, was developed. This scale assessed the frequency with which participants engaged in all self-care practices recommended for BP control. However, because performance of these behaviors requires prerequisite knowledge, it also was important to measure participants’ comprehension of the behaviors recommended for BP control. Therefore, the Blood Pressure Knowledge Scale was developed to assess the estimative operations of self-care agency.
Item Development
The items for the Blood Pressure Knowledge and Self-Care Scales were derived predominantly from empirical evidence. Because self-care is learned within a cultural context, knowledge and beliefs about BP control may vary among different cultural groups. Therefore, as a prelude to the current study, qualitative work was conducted to obtain the emic view of African Americans related to self-care for BP control (Peters, Aroian, & Flack, 2006). Results from focus group data supported inclusion of each of the JNC 7 recommendations for lifestyle modification. The seven JNC 7 behaviors addressed were those related to diet, weight control, physical activity, and alcohol and tobacco use. Focus group participants suggested additional questions to be included related to stress reduction, perceived need for physician care, and the use of medications to control blood pressure. These questions, although not specifically included in the JNC recommendations, were consistent with other research regarding blood pressure control (Alexander et al, 1999; Douglas et al., 2003; Spence et al., 1999). The final 10 items generated reflect the state-of-the-science regarding self-care behaviors necessary to prevent and control high BP, as well as the cultural perspective of African Americans.
Administration and Scoring of the Scales
The initial Blood Pressure Knowledge Scale and the Blood Pressure Self-Care Scale were both 10-item instruments that took approximately 5 to 10 minutes to complete. Each was created using a 7-point, bipolar format. Items related to BP knowledge synthesized the knowing components of the estimative operations of self-care agency. BP knowledge questions ask respondents to determine the degree to which they thought specific self-care behaviors would control BP, using the anchors of “extremely unlikely” and “extremely likely.” Items on the BP Self-Care Scale ask respondents to determine how often they engage in the specified BP control behavior using the anchors of “never” and “always.” The self-care item related to adherence to BP medications was coded to apply only to those participants with a known diagnosis of hypertension who were receiving pharmacological treatment. Total scores are determined as the average of the scores on each item. Total scores near 7 indicate high level of knowledge that the behaviors are important for BP control and consistent engagement in self-care practices. Using the Flesch-Kincaid method, both scales were at a 7th grade reading level, primarily due to the level of the repeated stem (“keep blood pressure within normal limits”). Prior to implementing the scales with the full sample, both instruments were pre-tested with 10 African American adults using the “Think Aloud” method to establish their comprehension and ease of response (Kucan & Beck, 1997). The five men and five women, who met the larger study inclusion criteria, completed the instruments without difficulty.
Method
Sample
The target population for this study was African American adults between 21 and 65 years of age, reporting general good health, without obvious dementia, psychiatric disorders, or drug use, and able to read/write English. A convenience sample of 306 participants was recruited from multiple community sites such as shopping malls, churches, and community festivals from June 2006 through January 2007. Recruitment sites were chosen to provide a broad representation of African Americans living in a large metropolitan city. The sample was fairly evenly divided by sex, 53% women (n = 161) and 47% men (n = 145). The mean age was 44.4 years (SD = 12.41) with a range of 21 to 65 years. Respondents were well distributed by education with a range of 4 to 20 years (M = 12, SD = 2.35) and annual family income with 26% (n = 78) reporting < $10,000/yr and 24% (n = 75) reporting ≥ $40,000/yr. Respondents included those without a diagnosis of hypertension (62%, n =191), as well as 38% (n = 115) with a known history of the disease.
Procedures
Institutional Human Subjects Investigation Committee approval was obtained prior to any participants being recruited. Data collection was done at the community recruitment sties. After obtaining consent, participants completed the BP Knowledge and BP Self-Care Scales and then had their BP measured. Questionnaires were designed to be self-administered, but a small number of participants (< 5% of sample) requested the instruments be read to them by the African American research assistants. Participants received a $20 gift card to Target stores as compensation for their time.
Blood pressure was measured using the Omron HEM 907 automatic device. The precision (reliability) of the Omron measurement was established by comparison with readings taken with a mercury sphygmomanometer. The BP protocol established by the American Heart Association (Pickering et al., 2005) was used to obtain all BP readings. Two readings were taken 1 minute apart, and the average recorded. Participants with elevated pressures were counseled by master’s or doctorally prepared nurses involved with the study. Assessment of hypertension history and body mass index (BMI; weight [kg]/ (height [m] 2) was based on self-report data.
Results: Reliability and Validity of the Scales
Reliability of the Scales
The Cronbach’s alpha for internal consistency reliability for the 10 items comprising the BP Knowledge Scale was .90. The alpha scores if items were deleted ranged from .87 to .91 indicating that no single item decreased reliability appreciably. However, the item assessing the role of medications in controlling BP had an item-to-total scale correlation much lower than any other item (r = .36). The item stated: “If I have high blood pressure, the only way to keep my blood pressure within normal limits is to take medications (pills) every day as prescribed by my doctor.” Evaluation of the wording suggested that using the term “only way” to control BP may have been confusing, thus a decision was made to drop this item from the knowledge scale. The alpha for the revised 9-item scale was .91, with the corrected item-to-total correlations ranging from .62 to .80 indicating strong correlations with the total score.
Internal consistency reliability for the 10 items comprising the BP Self-Care Scale was α =.71. Evaluation of the item-to-total correlation revealed a negative correlation (r = −.13) for the item regarding alcohol use. Assessment of the item indicated that, despite no problems in pilot testing, the wording of the item could be confusing, and therefore, it was dropped from the scale. Cronbach’s alpha for the revised 9-item scale was .78, with alphas ranging from .73 to .80 if items were deleted. No further adjustments were made to the BP Self-Care Scale based on these data.
Validity
In order to establish the validity of the instruments, a rigorous examination process was undertaken to determine the degree to which the evidence supported the intended interpretation of test scores. Evidence based on content, internal structure, and relationships to other variables was evaluated (American Educational Research Association [AERA], 1999).
Evidence Based on Content
Prior to any participant testing both expert and cultural peer review was conducted to obtain evidence that the scale items were representative of the content domain (AERA, 1999). Expert review included using the JNC 7 expert-panel consensus guidelines to determine the content to be included, as well as having a physician certified as a hypertension specialist and two primary care nurse practitioners review each scale. The reviewers found the items to be relevant and representative of the behaviors necessary to control BP. Cultural peer review occurred with a consultant group of African American research assistants who were familiar with the results of the focus group data (Peters et al., 2006) and could assure that the emic perspective obtained in the qualitative data was captured. Further cultural peer review occurred with the pilot testing of the instruments.
Evidence Based on Internal Structure
Confirmatory factor analysis (CFA) was conducted on the two scales to assess the relationship of test items to the underlying constructs being evaluated. The CFAs were done using structural equation modeling techniques with AMOS 7.0 (Arbuckle, 2006). Evaluation of the CFA output assessed the degree to which the sample data fit, or was consistent with, the theoretical model. Four different types of fit measures were used to evaluate the hypothesized models: chi-square (X2); chi-square divided by degrees of freedom (CMIN/df); Comparative Fit Index (CFI); and the root mean square error of approximation (RMSEA; Kline, 1998). In addition to evaluating overall model fit, we also examined standardized residuals and checked that parameter estimates were in the appropriate range.
A one factor CFA was fit to the 10-item BP Knowledge Scale. Although the fit of this model was marginally acceptable (X2(33) = 92.82, p< .01; CMIN/df = 2.81; CFI =.96; RMSEA =.077), one item, ‘medication use’, had a negative loading. Thus, the CFA confirmed the decision made based on item-to-total correlations to delete the medication item. The single factor CFA with this item omitted achieved a good fit (X2(25) = 59.75, p < .01; CMIN/df = 2.39; CFI = .98; RMSEA = .068). The standardized factor loadings ranged from .63 (alcohol) to .88 (weight control). All were statistically significant at p <.001, and the squared multiple correlations for each item ranged from .40 (alcohol) to .77 (weight control; Figure 1).
Figure 1.
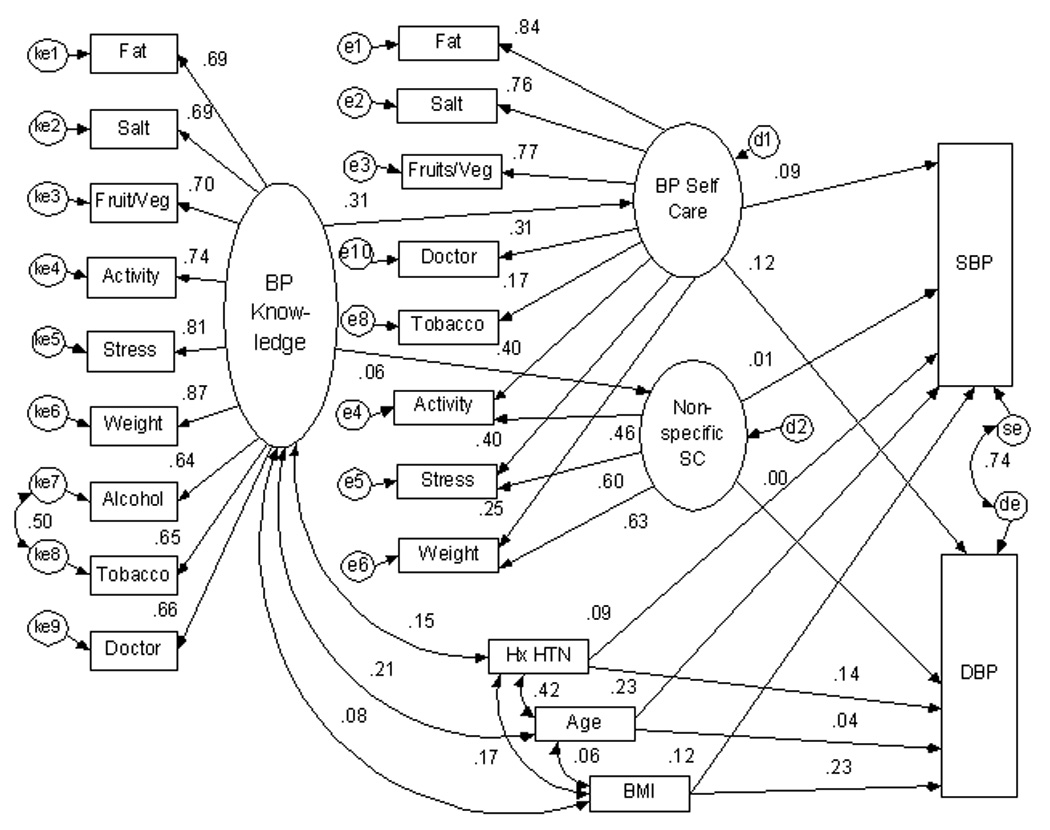
A one- factor CFA was fit to the 10-item BP Self-Care Scale, with poor fit results (X2(35) = 205.39, p< .001; CMIN/df = 5.87; CFI =.74; RMSEA =.126). There was a negative factor loading for the alcohol item, confirming results found with the item-to-total correlation. Thus, that item was dropped. A CFA of the 9-item BP Self-care scale was conducted. The initial fit of this model was poor (X2(22) = 70.84, p <.001; CMIN/df = 3.22; CFI = .94 RMSEA = .085). The fit of the one-factor model was improved by adding four correlated error terms across five items and by omitting one additional item that was relevant only to participants receiving blood pressure medication (X2(16) = 30.56, p = .015; CMIN/df = 1.91; CFI = .98 RMSEA = .055; revised 8-item Cronbach’s alpha .72). However, this kind of correlated error suggests unidentified dimensions. Using CFA in an exploratory way, as is common when the initial model fails to fit adequately (Jörsekog, 1993), we considered several multifactor models and settled on a model consisting of one common BP self-care factor with significant loadings on each of the 8 self-care items, and one smaller, non-specific self-care residual factor loading on three of the 8 items (activity, weight control, and stress management). The fit of this bi-factor model was acceptable (X2(17) = 42.14, p = .001; CMIN/df = 2.48; CFI = .96; RMSEA = .070), and the common factor was congruent with our original conceptualization (Figure 1). All items had significant loadings for the common BP self-care factor, with standardized loadings ranging from .18 (tobacco, p = .005) to .84 (low fat diet, p <.001). The 3-item residual factor had standardized loadings of .45 (activity), .63 (weight control), and .60 (stress management), all of which were significant at p <.001. The common factor (BP Self-care) and the residual factor (non-specific self-care) are uncorrelated; hence each factor explains non-overlapping portions of item variance. However, the smaller non-specific self-care factor does not stand on its own, like the common factor does, as a measure of behaviors necessary to control BP. Instead, the non-specific self-care factor is defined from the residual variance among its three items. As such, the residual factor is a source of systematic variance that may or may not be relevant in defining other dimensions of self-care.
Distribution of scores
Composite scores were computed for both the BP Knowledge and BP Self-Care Scales by summing their items. The overall scale mean for the 9-item BP Knowledge Scale was 5.81 (SD = 1.28). The distribution of knowledge scores was negatively skewed, indicating that participants had a high level of knowledge regarding the effectiveness of the JNC 7 recommended lifestyle behaviors for controlling BP (Table 1). The scores on the 8-item BP Self-care scale were normally disbursed with a mean of 4.42 (SD = 1.17; Table 1), indicating that the scale captured a wide range of actual behaviors. Younger people in this study (< 44 years) reported significantly lower knowledge of self-care for controlling BP than older people (44 – 65 years; t(287) = 3.70, p < .001), and reported significantly fewer BP self-care behaviors (t(288) = 3.73, p < .001). Participants with a history of hypertension had significantly higher knowledge (t(278) = 2.67, p =. 008) and self-care scores (t(303) = 3.47 p < .001) than the normotensive participants.
Table 1.
Scores on the Blood Pressure (BP) Knowledge and Self-care Scales
| Item | BP Knowledge | BP Self-Care Behaviors |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| (scale range 1–7) | (scale range 1–7) | |
| Low fat diet | 5.49 (1.84) | 3.66 (1.74) |
| Low salt diet | 5.76 (1.77) | 3.97 (2.02) |
| Fruits & Vegetables | 5.49 (1.78) | 3.82 (1.99) |
| Exercise | 5.93 (1.59) | 5.02 (1.99) |
| Maintain weight | 6.05 (1.54) | 4.33 (1.91) |
| Control stress | 6.19 (1.44) | 4.21 (1.89) |
| Avoid tobacco | 5.83 (1.83) | 5.35 (2.35) |
| Visit doctor regularly | 5.90 (1.63) | 5.04 (2.22) |
| Avoid alcohol | 5.69 (1.84) | 3.32 (2.58) (not included in final scale) |
| Medication adherence | 4.71 (2.19) (not included in final scale) | 5.84 (1.97) (not included in final scale) |
| Total Score | 5.81 (1.28) | 4.43 (1.17) |
Evidence Based on Relationship to Other Variables
Convergent evidence
Because no other instruments could be found that assessed the combined totality of self-care practices necessary to control BP, it was difficult to obtain convergent evidence in this initial testing of the instruments. Therefore, evidence for convergent validity for the BP Self-care scale was obtained by using items from the stage of change General Health Survey (Nigg et al., 1999). There were significant positive correlations for all items compared. These included items related to eating a low fat diet (r = .39, p < .01), maintaining healthy weight (r = .27, p < .01), physical activity (r = .40, p < .01), tobacco use (r = .74, p < .01), and stress reduction (r = .15, p < .05).
Test-criterion relationship evidence
There were two criterion questions of interest: (1) did knowledge predict self-care, and (2) did knowledge and self-care predict blood pressure? Initial bivariate results revealed that there was a moderately strong, significant relationship between the BP Knowledge and BP Self-Care Scales (r = .31, p <.01). Knowledge was not significantly related to systolic blood pressure (SBP), but was significantly correlated with diastolic blood pressure (DBP) in an unexpected positive direction. Self-care behavior was not significantly correlated with either SBP or DBP (Table 2). Given the lack of correlation with BP, data were examined for potential confounding by other variables known to be associated with high BP. Analysis revealed that there were no significant differences in BP based on sex, level of education, or income. There were, however, significant differences in both the predictor variables (knowledge and self-care) as well as the outcome variables (SBP and DBP) based on age, body mass index (BMI), and previous diagnosis of hypertension. Persons with higher BMI (≥ 30) had lower self-care scores and higher SBP and DBP than those with lower BMI. Persons older in age (≥ 44 years) and those with a previous history of hypertension had higher knowledge and self-care scores, as well as higher SBP and DBP than younger persons.
Table 2.
Correlation Matrix of BP Knowledge and Self-Care with Age, History of Hypertension, Body Mass Index, Systolic and Diastolic Blood Pressure
| Knowledge | Self-care | Age | Hx HTN | BMI | SBP | DBP | |
|---|---|---|---|---|---|---|---|
| BP Knowledge | 1.00 | ||||||
| BP Self-care | .31** | 1.00 | |||||
| Age | .23** | .25** | 1.00 | ||||
| Hx HTN | .14* | .19** | .43* | 1.00 | |||
| BMI | .08 | −.14* | .06 | .18** | 1.00 | ||
| SBP | .06 | .09 | .31** | .23** | .14* | 1.00 | |
| DBP | .12* | .06 | .15* | .22** | .25* | .75** | 1.00 |
| Mean | 5.81 | 4.43 | 44.42 | --- | 29.78 | 129.09 | 80.81 |
| SD | (1.28) | (1.17) | (12.41) | (6.41) | ( 19.06) | (12.87) | |
p <.05
p <.01
BP = blood pressure; Hx = history; HTN = hypertension; BMI = body mass index; SBP = systolic blood pressure; DBP = diastolic blood pressure
To further evaluate the hypothesized relationships, structural equation modeling (SEM) was used to test a simple, complete mediation model controlling for the confounding effects of age, BMI, and history of hypertension. An acceptable fit was achieved (X2(191) = 388.49, p <.001; CMIN/df=2.03; CFI=.92; RMSEA=.058), with the model accounting for 12% of the variance in SBP and 11% in DBP; however, most of the explained variance was due to the covariates (Figure 1). As an additional check, a multi-group SEM analysis was conducted splitting the sample by diagnosis of hypertension. Results revealed a poorer fit than for the model tested with the full sample. Thus, the single group model was accepted as the final model.
Further evaluation of the SEM output was done to evaluate parameter adequacy (Figure 1). The path from the predictor variable (knowledge) to the BP-specific mediating variable (BP self-care factor) was significant and in the predicted direction (β=.31, p <.001). Thus, increased BP knowledge was associated with increased BP self-care. The path from BP knowledge to the non-specific self-care factor was not significant. The path from the non-specific self-care factor was not significant to either outcome variable of SBP or DBP. Additionally, the path from the common factor, BP self-care, to the outcome variable of SBP was not significant. There was an unexpected finding of a significant, positive path coefficient between BP self-care and DBP (β=.12, p = .04), suggesting that increased self-care led to higher BP. Mixed results were seen in the paths between confounders and SBP and DBP. Body mass index was significantly, positively correlated with both outcome variables, (SBP, β=.12, p = .03; DBP, β=.12, p <.01). A positive history of hypertension was significantly correlated only with DBP (β=.14, p = .02), and age was significantly correlated only with SBP (β=.23, p = <.01).
Discussion
The BP Self-Care Scale, developed for this study, is the first instrument to simultaneously measure performance of the combined behaviors necessary to control BP. Similarly, the BP Knowledge scale is the first to simultaneously evaluate participants’ knowledge related to the totality of commonly prescribed BP-control recommendations. The initial testing and validation of the BP Knowledge and BP Self-Care Scales resulted in three key findings. First, there was good support for the validity of the scales based on content, internal structure, and convergent evidence. However, the second key finding was the unexpected results from the test-criterion relationships. Participants reported a high level of knowledge regarding the effectiveness of each lifestyle recommendation for controlling BP, and they reported a moderately high level of actual BP self-care behaviors, but neither knowledge nor self-care were related to recorded BP in the expected direction.
The intriguing finding of a positive relationship of knowledge and self-care with actual recorded BP warrants discussion. One possible theoretical explanation is that the causal relationship may be bi-directional. Although increased self-care usually is assumed to be positively linked to improved health outcomes, in this case lower BP, there is a time dimension that must be considered. Within the self-care deficit nursing theory (Orem, 2001), basic conditioning factors such as health state (e.g., current BP) act as informational inputs, conditioning the amount of self-care needed to ensure physiological integrity and functioning. It is possible that persons with BP levels in the prehypertensive range (120–140 mmHg SBP, 80–90 mmHg DBP) may have been instructed by their primary care provider to increase their self-care practices to prevent the onset of hypertension. Lifestyle modification is the first treatment recommendation for prehypertensive and newly diagnosed patients according to JNC 7 guidelines (Chobanian et al., 2003). In this scenario, the causal pathway is from BP to self-care. As a result, the self-care/blood pressure relationship would be bi-directional. Although reciprocal SEM techniques are available, we did not have data on variables that were linked to BP but not to the predictor variables and thus could not conduct this type of analysis with the current data.
The third finding is the importance of age as another basic conditioning factor that needs to be considered when discussing BP control self-care strategies. Younger people in this study reported significantly lower knowledge of self-care for controlling BP and fewer BP self-care behaviors than older people. Recognizing the increasing risk of hypertension with age, even in persons with near optimal blood pressure, as well as recognizing the lifetime risk of developing the disease (Lewington et al., 2002; Vasan et al., 2002), requires that health care providers give increased emphasis, counseling, and support to younger patients to prevent the onset of hypertension. If further study confirms the reliability, validity, and generalizabilty of these scales, providers might use these instruments to determine if patients have a limitation in their knowledge about lifestyle steps necessary for BP control, a lack of belief in the effectiveness of those steps, and/or a limitation in engaging in the self-care behaviors believed to be effective for BP control.
Both instruments were developed using input from focus groups conducted with African Americans (Peters et al., 2006). Focus group suggestions were highly consistent with JNC 7 recommendations while adding questions related to stress reduction, need for physician care, and use of medications to control BP, which are consistent with other research. Thus, race may have a limited role in determining the items used to measure participants’ knowledge and reported behaviors related to BP control. Race may be more important when evaluating responses to individual items. For example, African American respondents in this study rated controlling stress as the self-care behavior most likely to control BP, yet reported having some difficulty performing this behavior (Table 1). Additionally, cultural influences may be important in determining precursors to behavior (e.g., beliefs and attitudes) rather than indicative of the behavior itself. From a self-care deficit nursing theory perspective (Orem, 2001), cultural factors may affect the transitional (judging/deciding) operations of self-care agency, but the BP Self-care Scale measures only the end result of those decisions. Capturing the decision-making processes regarding BP-control behaviors requires development of a different instrument. The lack of a strong correlation between BP knowledge and BP self-care behavior supports the need for further study regarding the decision-making operations of self-care.
Despite reasonably acceptable psychometric properties of the instruments, additional work is still needed. Future research is suggested to overcome the limitations of the current study, including correcting problems with the alcohol and medication questions. Convergent evidence for the BP Self-care scale may be strengthened by using multiple methods to collect self-care data, such as adding diet diaries, pill counts, salivary cotinine, and adherence to scheduled provider visits. To evaluate the time dimension and assess for bi-directional relationships, a longitudinal design could be used. Alternately, a cross-sectional design specifically planned for reciprocal SEM analysis could be conducted. Additionally, both scales need to be tested with other African Americans to assess their stability, and with other racial and ethnic groups to determine their generalizablity. Future studies also would be needed to evaluate the effectiveness of using the instruments in a clinical intervention.
Conclusion
The initial testing and validation of the Blood Pressure Knowledge and Blood Pressure Self-Care Scales demonstrated acceptable psychometric properties. As measures of knowledge and actual self-care behaviors to control BP, with further testing the scales may have clinical utility. Both scales are easy to administer, providing a quick assessment of a person’s knowledge of the lifestyle recommendations needed to control BP as well as a quick assessment of areas of self-care behaviors that may need more education and support. Additional work is needed to determine the scales’ utility in predicting blood pressure, at the same time recognizing that an alternative causal pathway may exist such that knowledge of BP may predict self-care behaviors.
Acknowledgments
This study was supported by a grant from the National Institute of Nursing Research Grant No. 1 R15 NR008489-01
Contributor Information
Rosalind M. Peters, Adult Health, Wayne State University – College of Nursing, Detroit, MI.
Thomas N. Templin, Research, Wayne State University – College of Nursing, Detroit, Michigan.
References
- Alexander CN, Schneider RH, Staggers F, Sheppard W, Clayborne BM, Rainforth M, et al. Trial of stress reduction for hypertension in older African Americans. II. Sex and risk subgroup analysis. Hypertension. 1996;28:228–237. doi: 10.1161/01.hyp.28.2.228. [DOI] [PubMed] [Google Scholar]
- American Educational Research Association. Standards for educational and psychological testing, American Educational Research Association, American Psychological Association, National Council on Measurement in Education. Washington, D.C.: Author; 1999. [Google Scholar]
- Arbuckle JL. Amos (Version 7.0) [Computer Program] Chicago: SPSS; 2006. [Google Scholar]
- Campbell NRC, Burgess E, Choi BCK, Taylor G, Wilson E, Cléroux J, et al. Lifestyle modifications to prevent and control hypertension. Part 1: Methods and an overview of the Canadian recommendations. Canadian Medical Association Journal. 1999;160(9 Suppl.):S1–S6. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Racial/ethnic disparities in prevalence, treatment, and control of hypertension --- United States, 1999–2002. Morbidity & Mortality Weekly Report - MMWR. 2005;54:7–9. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. State-specific prevalence of current cigarette smoking among adults and secondhand smoke rules and policies in homes and workplaces - United States, 2005. Morbidity & Mortality Weekly Report - MMWR. 2006;55:1148–1168. [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Cooper R, Rotimi C, Ataman S, McGee D, Osotimehin B, Kadiri S, et al. The prevalence of hypertension in seven populations of West African origin. American Journal of Public Health. 1997;87:160–168. doi: 10.2105/ajph.87.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespo CJ, Smith E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: Results from the Third National Health and Nutrition Examination Survey, 1988–1994. American Journal of Preventive Medicine. 2000;18:46–53. doi: 10.1016/s0749-3797(99)00105-1. [DOI] [PubMed] [Google Scholar]
- Douglas JG, Bakris GL, Epstein M, Ferdinand KC, Ferrario C, Flack JM, et al. Management of high blood pressure in African Americans: Consensus statement of the Hypertension in African Americans Working Group of the International Society of Hypertension in Blacks. Archives of Internal Medicine. 2003;163:525–541. doi: 10.1001/archinte.163.5.525. [DOI] [PubMed] [Google Scholar]
- Jen KL, Brogan K, Washington OG, Flack JM, Artinian NT. Poor nutrient intake and high obese rate in an urban African American population with hypertension. Journal of the American College of Nutrition. 2007;26:57–65. doi: 10.1080/07315724.2007.10719586. [DOI] [PubMed] [Google Scholar]
- Jöreskog K. Testing structural equation models. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 294–316. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- Kruger J, Yore MM, Solera M, Moeti R. Prevalence of fruit and vegetable consumption and physical activity by race/ethnicity – United States, 2005. Morbitidy & Mortality Weekly Report - MMWR. 2007;56:301–304. [PubMed] [Google Scholar]
- Kucan L, Beck IL. Think aloud and reading comprehension research: Inquiry, instruction, and social interaction. Review of Educational Research. 1997;67:271–299. [Google Scholar]
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Prospective Studies Collaboration. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- Nigg CR, Burbank P, Padula C, Dufresne R, Rossi JS, Velicer WF, et al. Stages of change across ten health risk behaviors for older adults. The Gerontologist. 1999;39:473–482. doi: 10.1093/geront/39.4.473. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Orem D. Nursing concepts of practice. 6th ed. St. Louis, MO: Mosby; 2001. [Google Scholar]
- Peters RM, Aroian KJ, Flack JM. African American culture and hypertension prevention. Western Journal of Nursing Research. 2006;28:831–854. doi: 10.1177/0193945906289332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals. Part 1: Blood pressure measurement in humans: A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary approaches to Stop Hypertension (DASH) diet. DASH - Sodium Collaborative Research Group. New England Journal of Medicine. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- Schoenborn CA, Adams PF. Alcohol use among adults: United States, 1997–98. Advance Data from Vital and Health Statistics: no.324. 2002:1–20. (revised April 18) [PubMed] [Google Scholar]
- Spence JD, Barnett PA, Linden W, Ramsden V, Taenzer P. Lifestyle modifications to prevent and control hypertension. Part 7: Recommendations on stress management. Canadian Medical Association Journal. 1999;160(9 Suppl.):S46–S50. [PMC free article] [PubMed] [Google Scholar]
- Stamler J. The INTERSALT Study: Background, methods, findings, and implications. American Journal of Clinical Nutrition. 1997;65 Suppl.:626S–642S. doi: 10.1093/ajcn/65.2.626S. [DOI] [PubMed] [Google Scholar]
- Svetkey L, Chen Y, McKeown S, Preis L, Wilson A. Preliminary evidence of linkage of salt-sensitivity in Black Americans at the B2 Adrenergic receptor locus. Hypertension. 1997;29:918–922. doi: 10.1161/01.hyp.29.4.918. [DOI] [PubMed] [Google Scholar]
- Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287:1003–1010. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]


