Abstract
Two types of blast colonies can be stimulated to develop in semisolid agar cultures of murine bone marrow cells. Typically, these are either multicentric colonies stimulated by stem cell factor (SCF) plus interleukin-6 (IL-6) or dispersed colonies stimulated by Flt3 ligand (FL) plus IL-6. Both types of blast colony-forming cells (BL-CFCs) can generate large numbers of lineage-committed granulocyte-macrophage progenitor cells and exhibit some capacity for self-generation and the formation of eosinophil and megakaryocyte progenitor cells. However, the two populations of BL-CFCs are largely distinct and partially separable by fluorescence-activated cell sorting and are distinguished by differing capacity to form granulocyte-committed progeny. Both types of BL-CFCs can generate dendritic cells and small numbers of lymphocytes but the FL-responsive BL-CFCs have a greater capacity to form both B and T lymphocytes. Both types of blast colonies offer remarkable opportunities to analyze multilineage commitment at a clonal level in vitro.
Keywords: blast colonies, T and B lymphocytes
The existence and functional capacity of hematopoietic stem cells were established from studies using hematopoietic cells transplanted to lethally irradiated mice or severely myelo-depressed patients (1, 2). The major features of this cell class are a capacity for self-renewal, an ability to generate hematopoietic cells in all lineages on a long-term basis and, in normal health, to have a low or noncycling status. Such cells have been reported to segregate by fluorescence-activated cell sorting (FACS) into fractions that are lineage-negative, ScaI+, Kit+ (LSK fractions), and are CD34− and Flt3− (3). A second type of ancestral multipotential hematopoietic cell was identified by its capacity to generate hematopoietic colonies in the spleen of irradiated recipients (CFU-S) (4). CFU-S are regarded as only having a short-term repopulating capacity and to be the early progeny of stem cells (5). FACS analysis indicated that CFU-S are highly enriched in LSK fractions that are CD34+ Flt3− (3). Assays for hematopoietic stem cells and CFU-S depend on analyses in irradiated mice and this does not allow the processes by which they generate lineage-committed progeny to be manipulated or analyzed at a clonal level.
For this reason, it has become important to analyze the processes of cell division and commitment in hematopoietic precursor cells that can be grown clonally in vitro. The most mature hematopoietic precursors able to proliferate clonally in vitro are the lineage-restricted colony-forming cells. These can produce up to 5,000 progeny cells but have no capacity for self-generation (6, 7). However, there is a more ancestral class of hematopoietic cells that is also able to grow clonally in vitro—the blast colony-forming cells. Blast colony-forming cells were studied initially using hematopoietic populations enriched for noncycling immature precursors after pretreatment of mice with 5-fluorouracil and later using cells from mouse fetal liver. Both types of studies documented that blast colonies arose from single cells and were multipotential, able to generate all myeloid lineage cells and probably B lymphocytes (8–12).
In more recent years, two different types of blast colonies have been shown to be formed in semisolid agar cultures by murine adult bone marrow cells responding either to stimulation by stem cell factor plus G-CSF or IL-6 (13) or by Flt3 ligand plus a cytokine using the GP130 receptor (14). In view of the potential value of using blast colony-forming cells to reveal the mechanisms responsible for lineage commitment, it is important to establish whether these two types of blast colony-forming cells are identical or distinct, whether they can self-generate, how they relate to ancestral cells including CFU-S, and the range of lineage-committed progeny that is able to be generated by them.
The present studies have addressed these questions and have indicated that the two types of blast colony-forming cells are largely distinct and that both are multipotential.
Results
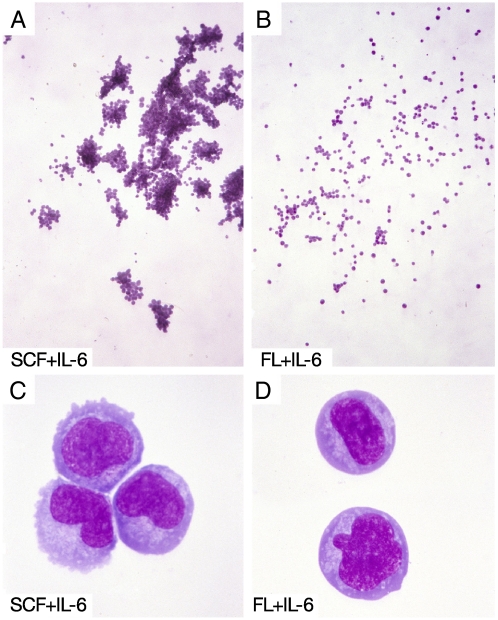
After synergistic stimulation by combinations of regulatory factors, murine bone marrow cells can generate two types of colonies that are composed entirely of blast cells. With stem cell factor (SCF) combined with either G-CSF or IL-6, the predominant blast colonies that develop are multicentric in shape (Fig. 1A) (13). In contrast, blast colonies stimulated to develop by the combination of Flt3-ligand (FL) + IL-6 are more commonly composed of dispersed cells (Fig. 1B) (14). The cells in both types of colonies have similar morphologies of undifferentiated blast cells (Fig. 1 C and D). Analysis showed that with all three paired stimuli, the number of blast colonies forming increased in a linear manner when increasing numbers of marrow cells were cultured (data not shown), and the cultures could therefore be used to enumerate blast colony-forming cells in various tissues.
Fig. 1.
The morphology of the two types of murine blast colonies. (A) A 7-day multicentric blast colony stimulated by SCF+IL-6 and C its constituent blast cells. (B) A 7-day dispersed blast colony stimulated by FL+IL-6 and D its constituent blast cells.
In adult C57BL/6, DBA/1, and BALB/c mice, the frequency of blast colony-forming cells in the marrow was similar (10–25 per 25,000 marrow cells). Small numbers of colony-forming cells (1–5 per 50,000 cells) were present in the spleen but none were detected in mesenteric lymph node, thymus, or peritoneal populations. As shown in Table 1, blast colony-forming cells of both types were present in E14 fetal liver, neonatal marrow, and liver and, at higher frequency, in adult marrow.
Table 1.
Frequency of blast colony forming cells in fetal, neonatal, and adult C57BL/6 tissues
| Organ | Mean number of colonies per 104 cells |
|||
|---|---|---|---|---|
| SCF + G-CSF Blast |
FL + IL-6 Blast |
|||
| Multi | Disp | Multi | Disp | |
| E14 fetal liver (n = 9) | 1.6 ± 0.7 | 0.1 ± 0.2 | 1.1 ± 0.7 | 1.2 ± 1.0 |
| Neonatal liver (n = 8) | 2.0 ± 2.5 | 0.1 ± 0.2 | 0.9 ± 1.1 | 2.4 ± 2.8 |
| Neonatal marrow (n = 8) | 1.4 ± 0.9 | 0.1 ± 0.1 | 1.9 ± 1.2 | 2.3 ± 1.0 |
| Adult marrow (n = 9) | 4.0 ± 0.8 | 1.2 ± 0.2 | 2.0 ± 0.8 | 4.4 ± 1.6 |
Cultures of fetal and neonatal cells contained 10,000 cells/culture. Adult marrow cultures contained 25,000 cells per culture,but the colony numbers have been adjusted to colonies per 10,000 cells. Figures shown are means ± standard deviations. Blast multi = multicentric blast colony; Blast Disp = dispersed blast colony.
In cultures containing the combined stimuli of SCF+IL-6+FL, both morphological types of blast colonies remained clearly evident and the number of blast colonies that developed was higher than with either SCF+IL-6 or FL+IL-6. As reported previously (14), in most experiments, the numbers were approximately additive. This implied that most of the cells forming blast colonies when stimulated by SCF+IL-6 were different from those forming colonies when stimulated by FL+IL-6 but that some overlap was likely between the two populations.
Although certain progenitor cells can probably respond to more than one growth factor and may be counted twice, the frequency of various clonogenic cells in adult mouse marrow can be approximated by determining maximal numbers of each colony type stimulated by the most active growth factor or growth factor combinations. Table 2 lists these estimates for C57BL/6 marrow using the most active stimuli. The data show that the frequency of blast colony-forming cells is not particularly low compared with numbers of lineage-committed progenitors. If blast colony-forming cells were to generate these latter cells, the numbers of cells needing to be produced per blast colony-forming cell would not be high.
Table 2.
Frequency of clonogenic cells in adult C57BL/6 bone marrow
| Colony type | Stimulus | Number of colonies |
|---|---|---|
| Blast-multicentric | SCF + IL-6 | 11 ± 6 |
| FL + IL-6 | 5 ± 3 | |
| Blast-dispersed | SCF + IL-6 | 4 ± 2 |
| FL + IL-6 | 8 ± 4 | |
| Granulocytic | GM-CSF | 26 ± 9 |
| Granulocyte-macrophage | GM-CSF | 12 ± 5 |
| Macrophage | M-CSF | 42 ± 12 |
| Eosinophil | GM-CSF | 4 ± 2 |
| Megakaryocyte | SCF + IL-3 + EPO | 21 ± 6 |
Mean colony numbers ± standard deviations in cultures of 25,000 C57BL/6 marrow cells from five individual mice.
Previous studies have shown that lineage-committed granulocytic, granulocyte-macrophage, and macrophage colonies contain no detectable colony-forming cells when the colony cells are resuspended and recultured in secondary cultures (7). In contrast, blast colonies whether stimulated by SCF+IL-6 or FL+IL-6 contained numerous colony-forming cells (Table 3). In pooled data from SCF plus IL-6-stimulated blast colonies, the overall relative frequencies of various secondary colony types were similar to those in bone marrow using the same stimulus (Fig. 2A). However, it was notable that apparently identical colonies contained widely varying numbers of colony-forming cells in the various lineages as shown in the examples in Fig. 2B and as evidenced by the large standard deviations in the data in Table 3. The number of secondary colonies grown from SCF+IL-6 blast colonies was consistently higher than the number grown from FL+IL-6 blast colonies but this may have been due, at least in part, to the fact that the mean number of cells in SCF+IL-6 blast colonies (4,310 ± 2,410) was also higher than the mean number of cells in FL+IL-6 blast colonies (2,050 ± 940). It was notable in all secondary cultures stimulated by GM-CSF or SCF+IL-3+Epo that there was a consistent relative deficit in the numbers of granulocytic and granulocyte-macrophage progenitor colonies grown from blast colonies stimulated by FL+IL-6 compared with colonies stimulated by SCF+IL-6 (Table 3 and Fig. 2). In secondary cultures of C57BL/6 blast colonies generated using either stimulus, there was an absence of eosinophil colony-forming cells and only a few megakaryocyte colonies developed.
Table 3.
Calculated mean number of progenitor cells per blast colony formed by C57BL/6 marrow cells
| Stimulus (number of colonies analyzed) | Mean number of cells per colony | GM-CSF |
M-CSF |
SCF + IL-3 + EPO |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G | GM | M | Eo | G | GM | M | Blast |
G | GM | M | Eo | Meg | |||
| Multi | Disp | ||||||||||||||
| SCF + IL-6 (n = 35) | 4310 ± 2410 | 137 ± 144 | 118 ± 186 | 249 ± 302 | 0 ± 0 | 11 ± 22 | 28 ± 42 | 609 ± 737 | 2 ± 7 | 0 ± 0 | 170 ± 262 | 144 ± 196 | 126 ± 137 | 0 ± 0 | 4 ± 11 |
| FL + IL-6(n = 25) | 2050 ± 940 | 3 ± 8 | 14 ± 34 | 149 ± 228 | 0 ± 0 | 1 ± 3 | 7 ± 22 | 216 ± 303 | 0 ± 0 | 1 ± 5 | 11 ± 34 | 22 ± 46 | 71 ± 192 | 0 ± 0 | 0 ± 0 |
Progenitor cells may be responsive to more than one growth factor and the numbers of colonies with each stimulus are therefore not necessarily additive. Mean values ± standard deviations. G, granulocyte colony; GM, granulocyte-macrophage colony; M, macrophage colony; Eo, eosinophil colony; M, megakaryocyte colony; Blast Multi, multicentric blast colony; Blast Disp, dispersed blast colony.
Fig. 2.
Blast colonies contain varying numbers of lineage-committed progenitor cells. (A) Pooled data from colonies formed by 10 recultured C57BL/6 blast colonies initiated by SCF+IL-6 or FL+IL-6. Note that the frequencies of granulocytic (G); granulocyte-macrophage (GM); and macrophage (M) colonies in the pooled data from SCF plus IL-6-initiated colonies when then stimulated by GM-CSF or M-CSF resemble the spectrum of colonies formed by C57BL/6 normal bone marrow (NBM) cells with these stimuli. However, a deficit in cells forming granulocyte-containing colonies is evident in blast colonies initiated by FL+IL-6. (B) The data from individual recultured blast colonies initiated by SCF+IL-6 shows the great variation between individual colonies in the number and type of secondary colonies stimulated by GM-CSF (GM) or M-CSF (M).
The numbers of megakaryocyte progenitors detected in these assays on blast colony cells were probably lower than those actually present. In parallel studies, when blast colonies were cultured in serum-free suspension cultures, five of 17 SCF-initiated colonies and two of 17 FL-initiated colonies generated megakaryocyte progeny as identified by morphology and verified as CD41-positive cells by FACS analysis (data not shown). This contrasted with a frequency of only six in 35 SCF-initiated and zero in 25 FL-initiated blast colonies found to contain megakaryocyte progenitor cells in secondary agar cultures.
Of major relevance was whether blast colony-forming cells could exhibit self-generation. With C57BL/6 blast colonies stimulated either by SCF+IL-6 or by FL+IL-6, on average, few progeny blast colony-forming cells were observed. In line with the heterogeneity of blast colony-forming cells, occasional blast colonies contained numerous blast colony-forming cells but the majority did not. No parent-progeny relationship was evident because blast colony-forming cells of both types were noted in colonies initiated either by SCF or FL. In cultures of blast colonies grown from the marrow of mice of other strains, low numbers of blast colonies were again noted (Table 4), supporting the conclusion that blast colony-forming cells have a low but definite capacity for self-generation.
Table 4.
Recloning of blast colony cells (excluding GM colonies)
| Strain | Stimulus (number of colonies analyzed) | Calculated number of colony-forming cells per colony |
|||
|---|---|---|---|---|---|
| Blast Multi | Blasts Disp | Eo | Meg | ||
| C3H HeB | SCF + IL-6 (n = 15) | 2 ± 3 | 3 ± 7 | 1 ± 4 | 1 ± 2 |
| FL + IL-6 (n = 15) | 1 ± 3 | 0 ± 0 | 0 ± 0 | 0 ± 0 | |
| DBA2 | SCF + IL-6 (n = 15) | 5 ± 13 | 0 ± 0 | 0.5 ± 2.1 | 2 ± 4 |
| FL + IL-6 (n = 15) | 5 ± 10 | 0 ± 0 | 0 ± 0 | 0 ± 0 | |
| BALB/c | SCF + IL-6 (n = 15) | 2 ± 6 | 12 ± 28 | 0 ± 0 | 3 ± 6 |
| FL + IL-6 (n = 15) | 0 ± 0 | 0 ± 0 | 0 ± 0 | 0 ± 0 | |
| 129 | SCF + IL-6 (n = 15) | 3 ± 12 | 1 ± 2 | 0 ± 0 | 0 ± 0 |
| FL + IL-6 (n = 15) | 4 ± 10 | 0 ± 0 | 0 ± 0 | 0 ± 0 | |
| CBA | SCF + IL-6 (n = 15) | 0 ± 0 | 0 ± 0 | 1 ± 2 | 0 ± 0 |
| FL + IL-6 (n = 15) | 0 ± 0 | 1 ± 2 | 0 ± 0 | 1 ± 2 | |
Mean colony numbers ± standard deviations. Blast Multi, multicentric blast colony; Blast Disp, dispersed blast colony; Eo, eosinophil colony; Meg, megakaryocyte colony.
Relation of Blast Colony-forming Cells to Other Ancestral Hematopoietic Cells.
When bone marrow cells are fractionated by FACS sorting according to the protocol of Yang et al. (3), lineage− ScaI+ kit+ (LSK) cells can be further fractionated into three fractions: a CD34− Flt3− fraction containing long-term repopulating cells (LTLSK); a CD34+ Flt3− fraction containing CFU-S and short-term repopulating cells (STLSK); and a CD34+ Flt3+ fraction containing multipotential progenitor cells (MPP) with little repopulating capacity.
In eight separate experiments using C57BL/6 marrow cells, when all fractions including rejected fractions were assayed, approximately 50–60% of total blast colony-forming cells were found to be present in the LSK fractions. As shown in Table 5, blast colony-forming cells were present in all three LSK subfractions but the highest frequency of SCF-responsive blast colony-forming cells was present in the CD34+ Flt3− short-term repopulating fractions (STLSK). Conversely, it was notable in all experiments that cells forming dispersed blast colonies when stimulated by FL+IL-6 were relatively enriched in CD34+ Flt3+ (MPP) fractions. Triple FACS sorting of these fractions did not alter this pattern of segregation of blast colony-forming cells. This indicated that many FL+IL-6-responsive cells forming dispersed blast colonies were in fact separable from the cells that responded to SCF+IL-6 by forming multicentric colonies. At least some of the FL-responsive blast colony-forming cells were probably more mature as evidenced both by loss of ScaI and occasionally by the exhibition of lineage markers on these cells (data not shown). This conclusion was supported by the fact that dispersed blast colonies often contained some dying cells.
Table 5.
Distribution of blast colony-forming cells in FACS-fractionated C57BL/6 bone marrow cells
| FACS fraction | Stimulus | Blast colonies per 100 cells |
|
|---|---|---|---|
| Multi | Disp | ||
| LTLSK CD34− Flt3− (n = 8) | SCF + G-CSF | 12 ± 5 | 7 ± 3 |
| FL + IL-6 | 6 ± 4 | 7 ± 5 | |
| STLSK CD34+ Flt3− (n = 8) | SCF + G-CSF | 27 ± 9 | 4 ± 2 |
| FL + IL-6 | 15 ± 3 | 7 ± 3 | |
| MPP CD34+ Flt3+ (n = 8) | SCF + G-CSF | 5 ± 3 | 3 ± 2 |
| FL + IL-6 | 4 ± 3 | 27 ± 9 | |
Mean colony counts ± standard deviations from 8 separate fractionation experiments. In 4 of these experiments, the frequencies of Day 8 CFUs were also determined. Mean values based on colony counts uncorrected for seeding efficiency were for LTLSK 1 in 80 cells, STLSK 1 in 28 cells and for MPP 1 in 800 cells.
The enrichment of multicentric blast colony-forming cells occurred in CD34+ Flt3− fractions reported to be highly enriched for CFU-S (3). This association was confirmed by CFU-S analyses in four of the present experiments (Table 5) and raised the questions of whether multicentric blast colony-forming cells could be CFU-S and form colonies in the spleen of irradiated-recipients or whether such cells could be generated by CFU-S. Analysis of 15, day-11 spleen colonies from C57BL/6 mice injected with marrow cells detected low numbers of blast colony-forming cells of both types (1–2 per 104 cells) in four of the 15 colonies. The significance of this finding is dubious because two of five intercolony areas from the same spleens contained similar low numbers of blast colony-forming cells. In reverse experiments, 15,000 pooled day-7 multicentric or dispersed blast colony cells per mouse were unable to generate day 11 spleen colonies in irradiated recipients. However, this latter experiment merely suggested that the progeny of blast colony-forming cells did not contain CFU-S and was not a test of blast colony-forming cells themselves.
Production of Dendritic Cells and T and B Lymphocytes by Blast Colony-Forming Cells.
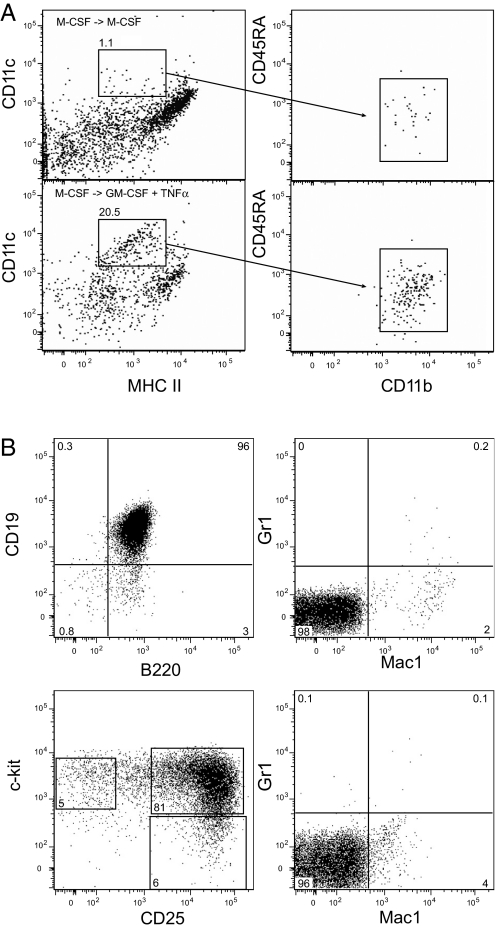
Cells from 7-day multicentric blast colonies that had been initiated by SCF+IL-6 or dispersed colonies that had been stimulated by FL+IL-6 were subcultured in cultures containing M-CSF and the resulting macrophage colonies were then maintained in liquid culture using M-CSF. The cultures were then split and half of each was further cultured with GM-CSF plus TNFα, a procedure used to induce the development of dendritic cells (15). After a further 3 days, analysis showed that when the M-CSF-responsive progeny of both types of blast colony-forming cells was switched to GM-CSF plus TNFα, many cells developed a dendritic cell phenotype (CD11c+ MHCII+ CD11b+, CD45RA−) (16) (Fig. 3A). Cells maintained throughout in M-CSF continued to exhibit the phenotype of macrophage cells.
Fig. 3.
Blast colonies contain cells able to form dendritic cells and T and B lymphocytes. (A) FACS analysis of dendritic cells formed by SCF plus IL-6-initiated blast colonies when grown in the presence of M-CSF (Upper) or GM-CSF and TNFα (Lower). (B) Immature B lymphocytes (Upper) and immature T lymphocytes (Lower) grown from a single day-7 C57BL blast colony initiated by FL+IL-6.
When cells from 7-day SCF- or FL-responsive C57BL/6 blast colonies were grown on underlayers supporting either B lymphocyte (OP9 cells) (17) or T lymphocyte development [OP9 cells expressing (DL-1)] (18), clear examples were observed in which colony cells generated cells with the markers of either B lymphocytes or T lymphocytes (Fig. 3B). Whereas only a small proportion of colonies stimulated by SCF + IL-6 contained cells capable of generating B or T lymphocytes (1/30 and 6/30, respectively), blast colonies stimulated by FL + IL-6 were able to generate B or T lymphocytes with relatively high efficiency (19/30 and 26/40, respectively). In 25 cases in which the same colony was analyzed for both B and T potential, 17 colonies generated both B and T progeny, five generated only T cells, and three generated only B cells. FACS analysis of 7-day blast colony cells failed to detect cells with B or T cell markers (data not shown). Portions of colonies used to generate lymphocytes were also cultured in conventional agar and produced granulocyte and/or macrophage colonies at frequencies similar to those shown in Table 3. These data suggest that the blast colonies formed by FL + IL-6 stimulation retain greater potential for lymphocyte differentiation than blast colonies formed by SCF + IL-6 stimulation.
Discussion
Two types of colonies composed of blast cells can be grown from murine hematopoietic tissues. The multicentric blast colonies, typically stimulated by SCF+IL-6 or G-CSF, contained more cells and more lineage-committed progenitors than the dispersed colonies typically stimulated by FL+IL-6. Both types of colony-forming cells were present in similar numbers in the murine fetal liver, neonatal liver, as well as bone marrow and adult bone marrow, with no clear indication that the appearance of one population of colony-forming cells preceded that of the other, and might therefore be potentially more ancestral.
Although both types of blast colony-forming cells generated large numbers of committed progenitors in the granulocyte-macrophage lineages, the two types were largely distinct populations for several reasons. Dispersed blast colony-forming cells responsive to FL+IL-6 were selectively enriched in CD34+ Flt3+ FACS fractions and had a lower capacity to produce granulocyte-committed progenitor cells than multicentric colony-forming cells stimulated by SCF+IL-6 that, in contrast, were selectively enriched in CD34+ Flt3− fractions. Conversely, FL-initiated dispersed blast colony-forming cells were able to generate both T and B lymphocyte progeny whereas SCF-initiated multicentric blast colony-forming cells had little capacity to produce either B lymphocytes or T lymphocytes. Finally, a combination of relevant stimuli (SCF+FL+IL-6) tended to result in the development of additive numbers of colonies in cultures in which the distinctive morphologies of both colony types were retained. A low capacity for self-generation was shown by both types of blast colony-forming cells but the data did not support the likelihood of a parent-progeny relationship between the two types.
Both types of blast colony-forming cells exhibited notable heterogeneity in their surface markers, responsiveness to proliferative stimuli, and the numbers and types of lineage-committed progeny they generated. This has made it difficult to firmly position these multipotential precursors in a hierarchy of hematopoietic precursor cells. Multicentric blast colony-forming cells were most highly enriched in FACS fractions reported to be enriched for CFU-S (3) but the cells were also present in stem cell fractions and in more mature multipotential cell fractions.
On balance, blast colony-forming cells appear to be located midway between long-term repopulating stem cells and multipotential cells. Their capacity for self-generation and their ability to generate extraordinary numbers of lineage-committed myeloid progenitor cells, each with a substantial capacity to produce hundreds of maturing progeny, was coupled with an ability to generate dendritic cells and T and B lymphocytes. The possible presence of cells in blast colonies able to generate erythroid or NK cells requires further study. However, from the present data, blast colony-forming cells are clearly multipotential and might well be able to sustain a certain level of basal hematopoiesis in multiple lineages in the absence of any cellular input from stem cells.
The observation that B and T lymphoid cells can be generated from blast colonies was somewhat surprising given the cytokines used to stimulate colony formation. It is possible that relevant additional cytokines may have been produced endogenously in the original marrow cultures. From the data, it was not possible to conclude how many cells in the blast colonies retained lymphoid potential; however, an earlier study suggested that the number of cells with B-lymphoid potential was likely to have been quite low (11). Nevertheless, these results indicate that lymphoid progenitors can be maintained in vitro for 7 days without losing their lymphoid potential. The observation that lymphoid potential is higher in blast colonies initiated by FL plus IL-6 is consistent with a role for FL in regulating lymphoid progenitor cells (19, 20). The finding that FL-responsive blast colony-forming cells are enriched in the CD34+ Flt3+ fraction of bone marrow likely reflects the fact that this fraction contains progenitor cells primed for lymphoid development (21, 22).
The multipotentiality of blast colonies, their clonal origin, and their ease of growth and analysis in vitro make them valuable populations for analyzing the mechanisms controlling self-generation and multilineage commitment in ancestral hematopoietic cells from normal or genetically manipulated mice.
Experimental Procedures
Mice.
All mice were produced in the animal facility of The Walter and Eliza Hall Institute and all studies were approved by the Animal Ethics Committee of this Institute.
Culture.
Marrow (25,000) or spleen (50,000) cells were cultured in 35-mm Petri dishes containing 1 ml of Dulbecco's Modified Eagle's Medium (DMEM) plus 20% modified newborn calf serum and 0.3% agar. Blast colony formation was stimulated either by the use of 100 ng per ml murine stem cell factor (SCF) plus 10 ng per ml human granulocyte colony-stimulating factor (G-CSF) or 100 ng per ml murine interleukin-6 (IL-6) or by murine Flt3 ligand (FL) 500 ng per ml plus murine IL-6 100 ng per ml. G-CSF was purchased from Amgen and all other cytokines were produced in this laboratory. After one week of incubation at 37°C in a fully humidified atmosphere of 10% C02 in air, cultures were scored at ×35 magnifications then fixed with 1 ml of 2.5% glutaraldehyde. After 4 h, cultures were floated intact onto glass slides, allowed to dry, and then stained for acetylcholinesterase, Luxol Fast Blue, and hematoxylin. Final colony counts and typing were then performed on the entire cultures at ×50 or ×100 magnifications (23).
Reculture of Blast Colonies.
Individual 7-day blast colonies were removed by using a fine sterile pipette, resuspended in 8 ml of agar-medium, and then cultured in duplicate for a further 7 days using 10 ng per ml murine GM-CSF, 10 ng per ml murine M-CSF, or 100 ng per ml murine SCF plus 10 ng per ml of murine IL-3 and 4 IU erythropoietin. Secondary colonies were processed and scored as above.
For dendritic cell cultures, C57BL/6 macrophage colonies were grown from blast colony cells using 10 ng/ml M-CSF then harvested and cultured for 7–14 days in suspension culture using 10 ng/ml M-CSF. Cultures were then split with one portion remaining with 10 ng/ml M-CSF whereas the other was cultured with 10 ng/ml GM-CSF plus 10 ng/ml TNFα to induce dendritic cell formation (15). After 3 days, cells were harvested, labeled, and analyzed for identifiable dendritic cells as previously described (16).
Lymphocyte Cultures.
OP9 and OP9-DL1 cells were maintained in α-MEM (MEM) supplemented with 20% (vol/vol) FCS, 1 mM l-glutamine, 10 mM Hepes, 1 mM sodium pyruvate, and 50 μM β-mercaptoethanol. For lymphocyte cultures, stromal cells were plated in 24-well plates at an appropriate density. Individual day-7 C57BL/6 blast colonies were removed from agar by using a fine pipette and resuspended in α-MEM modified as above, except containing only 10% (vol/vol) serum and supplemented with 5 ng/ml FL and 2% of the supernatant of an IL-7-producing cell line. Blast cells were plated on OP9 and/or OP9-DL1 stromal cells to generate B and/or T cells, respectively. After 7–14 days, hematopoietic cells were harvested and stained with fluorescently labeled antibodies to B220 (RA3–6B2), CD19 (ID3), Gr1 (RB6–8C5), Mac1 (M1/70), CD25 (7D4), and c-Kit (ACK-2) and analyzed by an LSR-II flow cytometer. Control cultures were prepared by using cell-free agar adjacent to blast colonies to exclude the presence of inconspicuous T or B lymphocyte precursors that might have been incorporated in expanding blast colonies.
Megakaryocyte Cultures.
For suspension culture of megakaryocytes, individual day-7 blast colonies were cultured in Stem Pro-34 medium (Gibco) with the following cytokine concentrations: 25 ng/ml FL, 25 ng/ml SCF, 200 ng/ml TPO, 2.5 U/ml EPO, 10 ng/ml IL-3, 25 ng/ml IL-6, and 25 ng/ml IL-11. Cells were analyzed after 7 days of incubation using FACS analysis for CD41 positivity (CD41 Clone MW Reg 30) together with an analysis of cytocentrifuge preparations.
Purification of LSK Subsets.
Bone marrow was harvested from 7–12 week-old C57BL/6 mice then fractionated by using antibody combinations as described previously (24).
Acknowledgments.
This work was supported by the Carden Fellowship Fund of the Cancer Council, Victoria, the National Health and Medical Research Council, Grant 461219, and National Institutes of Health Grant CA22556. C.A.d.G. and S.J.L. are recipients of Australian Postgraduate Awards, and K.T.G. is the recipient of a Stella Mary Langford Scholarship of the University of Melbourne.
Footnotes
The authors declare no conflict of interest.
References
- 1.Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414:105–111. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- 2.Verfaillie CM. Hematopoietic stem cells for transplantation. Nat Immunol. 2002;3:314–317. doi: 10.1038/ni0402-314. [DOI] [PubMed] [Google Scholar]
- 3.Yang L, Bryder D, Adolfsson J, Nygren J, Mansson R, Sigvardsson M, Jacobsen SEW. Identification of Lin− ScaI+kit+CD34+Flt3− short-term hematopoietic stem cells capable of rapidly reconstituting and rescuing myeloablated transplant recipients. Blood. 2005;105:2717–2723. doi: 10.1182/blood-2004-06-2159. [DOI] [PubMed] [Google Scholar]
- 4.Till JE, McCulloch EA. A direct measurement of the radiation sensitivity of normal mouse bone marrow cells. Radiat Res. 1961;14:213–222. [PubMed] [Google Scholar]
- 5.Weissman IL, Anderson DJ, Gage F. Stem and progenitor cells; origins, phenotypes, lineage commitments, and transdifferentiations. Annu Rev Cell Dev Biol. 2001;17:387–403. doi: 10.1146/annurev.cellbio.17.1.387. [DOI] [PubMed] [Google Scholar]
- 6.Metcalf D, Nicola NA. UK: Cambridge Univ Press; 1995. The hemopoietic colony-stimulating factors: From biology to clinical applications; pp. 1–327. [Google Scholar]
- 7.Metcalf D, Glaser S, Mifsud S, Di Rago L, Robb L. The preleukemic state of mice reconstituted with Mixl1-transduced marrow cells. Proc Natl Acad Sci USA. 2007;104:20013–20018. doi: 10.1073/pnas.0710339104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suda T, Suda J, Ogawa M. Single-cell origin of mouse hemopoietic colonies expressing multiple lineages in variable combinations. Proc Natl Acad Sci USA. 1983;80:6689–6693. doi: 10.1073/pnas.80.21.6689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keller G, Holmes W, Phillips RA. Clonal generation of multipotent and unipotent hemopoietic blast cell colonies in vitro. J Cell Physiol. 1984;120:29–35. doi: 10.1002/jcp.1041200105. [DOI] [PubMed] [Google Scholar]
- 10.Pharr PN, Ogawa M. Fetal liver blast cell colonies: A source of erythroid progenitors. Exp Hematol. 1988;16:748–751. [PubMed] [Google Scholar]
- 11.Ohara A, et al. Generation of B lymphocytes from a single hemopoietic progenitor cell in vitro. Int Immunol. 1991;3:703–709. doi: 10.1093/intimm/3.7.703. [DOI] [PubMed] [Google Scholar]
- 12.Aiba Y, Ogawa M. Development of natural killer cells, B lymphocytes, macrophages, and mast cells from single hematopoietic progenitors in culture of murine fetal liver cells. Blood. 1997;90:3923–3930. [PubMed] [Google Scholar]
- 13.Metcalf D. Lineage commitment of hemopoietic progenitor cells in developing blast cell colonies: Influence of colony-stimulating factors. Proc Natl Acad Sci USA. 1991;88:11310–11314. doi: 10.1073/pnas.88.24.11310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Metcalf D. Murine hematopoietic stem cells committed to macrophage/dendritic cell formation: Stimulation by Flk2-ligand with enhancement by regulators using the gp130 receptor chain. Proc Natl Acad Sci USA. 1997;94:11552–11556. doi: 10.1073/pnas.94.21.11552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caux C, Dezutter-Dambuyant C, Schmitt D, Banchereau J. GM-CSF and TNFα cooperate in the generation of dendritic Langerhans cells. Nature. 1992;360:258–261. doi: 10.1038/360258a0. [DOI] [PubMed] [Google Scholar]
- 16.Vremec D, et al. Production of interferons by dendritic cells, plasmacytoid cells, natural killer cells, and interferon-producing killer dendritic cells. Blood. 2007;109:1165–1173. doi: 10.1182/blood-2006-05-015354. [DOI] [PubMed] [Google Scholar]
- 17.Nakano T, Kodama H, Honjo T. Generation of lymphohematopoietic cells from embryonic stem cells in culture. Science. 1994;265:1098–1101. doi: 10.1126/science.8066449. [DOI] [PubMed] [Google Scholar]
- 18.Schmitt TM, Zuniga-Pflucker JC. Induction of T cell development from hematopoietic progenitor cells by delta-like-1 in vitro. Immunity. 2002;17:749–756. doi: 10.1016/s1074-7613(02)00474-0. [DOI] [PubMed] [Google Scholar]
- 19.McKenna HJ, et al. Mice lacking flt3 ligand have deficient hematopoiesis affecting hematopoietic progenitor cells, dendritic cells, and natural killer cells. Blood. 2000;95:3489–3497. [PubMed] [Google Scholar]
- 20.Sitnicka E, Bryder D, Theilgaard-Monch K, Buza-Vidas N, Adolfsson J, Jacobsen SE. Key role of flt3 ligand in regulation of the common lymphoid progenitor but not in maintenance of the hematopoietic stem cell pool. Immunity. 2002;17:463–472. doi: 10.1016/s1074-7613(02)00419-3. [DOI] [PubMed] [Google Scholar]
- 21.Adolfsson J, et al. Upregulation of Flt3 expression within the bone marrow Lin(-)ScaI(+)c-kit(+) stem cell compartment is accompanied by loss of self-renewal capacity. Immunity. 2001;15:659–669. doi: 10.1016/s1074-7613(01)00220-5. [DOI] [PubMed] [Google Scholar]
- 22.Mansson R, et al. Molecular evidence for hierarchical transcriptional lineage priming in fetal and adult stem cells and multipotent progenitors. Immunity. 2007;26:407–419. doi: 10.1016/j.immuni.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 23.Metcalf D. Ohio: AlphaMed Press, U.S.A; 2005. Blood Lines. An Introduction to Characterizing Blood Diseases of the Post-Genomic Mouse. [Google Scholar]
- 24.Loughran SJ, et al. The transcription factor Erg is essential for definitive hematopoiesis and the function of adult hematopoietic stem cells. Nat Immunol. 2008;9:810–819. doi: 10.1038/ni.1617. [DOI] [PubMed] [Google Scholar]