Abstract
It is a retrospective analytic study of 1,009 transpedicular screws (689 thoracic and 320 lumbosacral), inserted with free-hand technique in neuromuscular scoliosis using postoperative CT scan. The aim of paper was to determine the accuracy and safety of transpedicular screw placement with free-hand technique in neuromuscular scoliosis and to compare the accuracy at different levels in such population. All studies regarding accuracy and safety of pedicle screw in scoliosis represent idiopathic scoliosis using various techniques such as free-hand, navigation, image intensifier, etc., for screw insertion. Anatomies of vertebrae and pedicle are distorted in scoliosis, hence accurate and safe placement of pedicle screw is prerequisite for surgery. Between 2004 and 2006, 37 consecutive patients, average age 20 years (9–44 years), of neuromuscular scoliosis were operated with posterior pedicle screw fixation using free-hand technique. Accuracy of pedicle screws was studied on postoperative CT scan. Placement up to 2 mm medial side and 4 mm lateral side was considered within-safe zone. Of the 1,009 screws, 273 screws were displaced medially, laterally or on the anterior side showing that 73% screws (68% in thoracic and 82.5% in lumbar spine) were accurately placed within pedicle. Considering the safe zone, 93.3% (942/1009, 92.4% in thoracic and 95.3% in lumbar spine) of the screws were within the safe zone. Comparing accuracy according to severity of curve, accuracy was 75% in group 1 (curve <90°) and 69% in group 2 (curve >90°) with a safety of 94.8 and 91.2%, respectively (P = 0.35). Comparing the accuracy at different thoracic levels, it showed 67, 64 and 72% accuracy in upper, middle and lower thoracic levels with safety of 96.6, 89.2 and 93.1%, respectively, exhibiting no statistical significant difference (P = 0.17). Pedicle screw placement in neuromuscular scoliosis with free-hand technique is accurate and safe as other conditions.
Keywords: Neuromuscular scoliosis, Pedicle screw fixation, Free-hand technique, Postoperative CT scan, Accuracy, Safe
Introduction
The use of pedicle screw instrumentation was described by Boucher [5] in 1950s and was popularized by Roy-Camille et al. [34, 35] in 1960s. The initial use of pedicle screws began in the lumbar spine and as surgeons became more comfortable with the complex anatomy required for accurate screw placement, they evolved the use of pedicle instrumentation in thoracolumbar and thoracic spine [23, 24, 31]. Transpedicular screw fixation has many advantages over other spinal instrumentations such as Harrington rod fixation, Luque’s instrumentation, etc., in various pathologies [1, 27, 31, 39, 45]. Pedicle screws also prevent the need to place instrumentation within the spinal canal like sublaminar wiring [6], which creates the risk of neurological injury. When used in scoliosis surgery, transpedicular screws have been reported to enhance the operative correction [21, 39].
Besides the advantages of pedicular screw, its use is not without complications [7, 15, 16], especially when it penetrates in to the spinal canal. Because of its close proximity to spinal canal and surrounding vessels, misplacement of pedicle screw can lead to disastrous complication. So, accurate and safe placement of screw within the pedicle is a crucial step during the surgery. Various methods such as free hand technique, Penfield outside-in technique, under C-arm control, computer assisted navigational surgery and stereotectic surgery, etc., to put the pedicle screw have been described in the literature [20, 22, 29]. The use of intra-operative fluoroscopy for placement of pedicle screws has resulted in prolonged fluro time and radiation exposure to the surgical personnel and patient [32]. However, we have found that free-hand technique is relatively easy to learn and is as accurate [22] as the other methods, which were implemented in our study. There are also various intraoperative methods, such as SSEP, MEP or computer assisted surgery [11, 29], described to detect pedicle violation or neural injury. The literature also showed that accuracy and safety of pedicle screws was around 90–95% in various pathologies on postoperative CT scan, MRI or radiogram [2, 8, 18, 30, 36, 37]. In this study, we used postoperative CT scan to measure the accuracy and safety of the pedicle screw fixation with free-hand technique.
Patients with neuromuscular scoliosis are extremely difficult to control with brace and early operative treatment is mandatory to prevent progression of curve and pulmonary deterioration [6]. The anatomies of vertebrae and pedicle are also distorted in patients with neuromuscular scoliosis like idiopathic scoliosis [28, 43]. Pedicle screw fixation in such patients is difficult, so accurate and safe placement is mandatory to achieve the fixation [33]. The close proximity of the spinal cord and major soft tissue structures including the aorta, esophagus and lung adds a great risk to the procedure [9, 42]. The narrow and inconsistent shape of the thoracic pedicles makes the placement of pedicle screws technically challenging. To our knowledge, no data are available for the accuracy and safety of pedicle screw fixation with free-hand technique in neuromuscular scoliosis. The objective of this paper is to evaluate the accuracy and safety of pedicle screw fixation using postoperative CT scan in neuromuscular scoliosis.
Materials and methods
Between 2004 and 2006, 37 patients (22 male and 15 female) with neuromuscular scoliosis (12 CP, 13 DMD, 6 SMA, 3 Polio, 2 Neurofibromatosis and 1 Posttraumatic paralysis) underwent correction and fusion with transpedicular screw fixation using the free-hand technique. The mean age at the time of operation was 20 years (range 9–44 years) and average preoperative Cobb’s angle was 82° (range 30° to 150°).
In total, 1,009 screws were inserted; 689 screws in thoracic and 320 screws in lumbar spine. All pedicle screws were inserted using free-hand technique, in which anatomic landmarks and specific entry sites [10] were used to guide the surgeon. A spine fellow (HNM) reviewed digitized radiographs and CT scans of all the patients taken pre and postoperatively. All CT scans were digitized and viewed with the PACS system; hence all measurements were done with the help of software at a magnification of 300%. All screws were evaluated for intrapedicular placement and length twice, and their average values were taken for final calculation (r = 0.93, Pearson correlation coefficient). Any penetration of bony cortex was measured in millimeters. We have divided the medial or lateral penetration of the pedicle into grade 0 (fully contained within the pedicle), grade 1 (penetration <2 mm), grade 2 (penetration 2.1–4.0 mm), grade 3 (penetration 4.1–6.0 mm) and grade 4 (penetration >6 mm). The screw penetration anterior to vertebral body also measured the same. The screws displaced medially by <2 mm and laterally by <4 mm were considered as the screws within the safe zone, while the rest of displaced screws were considered as potentially at risk. We also analyzed the placement of screws according to severity of curves between group 1 (curves <90°) and group 2 (curves >90° using Chi-Square test. We also analyzed the thoracic pedicle screws placement according to upper thoracic (T1–T4), middle thoracic (T5–T8) and lower thoracic (T9–T12) levels using Chi-Square test.
Surgical technique
Spine was exposed, up to the tips of the transverse processes subperiosteally on both the sides. For the thoracic spine, facet joints were thoroughly cleaned off the soft tissue to ensure better visualization of bony landmarks. Neutrally rotated and the most distally located vertebra were chosen first for instrumentation. Starting point in all thoracic vertebrae was at the junction of a horizontal line along the inferior border of the facet joint and a vertical line at the junction of the outer third and inner two-thirds of the facet joint [10], which was chosen as ideal entry point for thoracic pedicle. For lumbar spine, the junction of mammillary process, inferior aspect of transverse process, and pars interarticularis (Roy-Camille technique) were chosen as entry point. First, before making the entry with probe in to the pedicle for initial 10–15 mm, the entry point was made rough with rounger to prevent slippage of awl and visualization of cancellous bone. Then, the further passage in the pedicle was made with pathfinder, for first 20 mm curve; directed laterally and then rotated medially for further entry without undue force while inserting.
The ball tip probe, which has a 2-mm blunt round tip and is slightly curved, was used to check the entry point that was already made with the probe the first time before taking pathfinder. The ball tip probe was again used to check the integrity of pedicle when an entry was made up to 20 mm with pathfinder and then was lastly used at final creation of pedicle passage. Initially the pathfinder pointed laterally as a safety measure to avoid medial wall perforation and after a depth of around 20 mm, it is removed and rotated so that the tip faced medially, reinserted and advanced further. The average depth to which the pathfinder can be advanced is usually around 20–25 mm for the upper thoracic region, 25–30 mm in the mid thoracic region, 30–40 mm for the lower thoracic region and 40–45 mm for lumbar region. The pathfinder was removed and a ball tip probe was introduced to feel the intact medial, lateral, superior, inferior and anterior cortices at each step. If all the cortices felt intact, the entry was tapped up to 20–25 mm and again pedicle integrity was checked with ball tip probe. In the absence of any breach, the screw with the appropriate length and diameter was inserted. If we find any breach in the pedicle wall, again the entry was made in different direction. We inserted screws at all levels to increase the rigidity of the instrumentation. Antero posterior and lateral radiographs were taken after placing the first screw to check the level and after that, all the screws were inserted.
After insertion of all the pedicle screws, deformity correction was carried out using rod derotation maneuver and if necessary, in situ bending of the rod [38] was done. As associated procedure, posterior vertebral column resection technique was used only in some cases of stiff curve, usually more than 90°, and thoracoplasty was done if large rib hump was present after the correction maneuver. Then the decortications of all laminae and facet joints were performed and fusion was performed with autologous bone grafts with allograft. The closure was performed in a standard manner over negative suction drain. After the operation, once the patient become hemodynamically stable, postoperative radiogram and CT scan were performed in all the patients.
Results
A total of 1009 screws, 689 in thoracic and 320 in lumbar, were inserted in 37 patients, which averaged 27 screws per patients. The diameter of the screws used ranged from 5.5 to 6.5 mm, 5.0 to 5.5 mm, 4.0 to 5.0 mm and 3.5 to 4.5 mm in lumbar, lower thoracic (T9–T12), middle thoracic (T5–T8), and upper thoracic (T1–T4) pedicles, respectively. Length of screws were 40–45 mm, 35–40 mm, 30–35 mm and 25–30 mm in lumbar, lower thoracic, middle thoracic, and upper thoracic area, respectively. The number of inserted screws and displaced screws that were displaced medially, laterally and anteriorly is summarized in Tables 1, 2, 3, which shows that 27% (273/1009) of inserted screws penetrated either medial or lateral wall comprising 10.7% (108/1009) and 16.3% (165/1009), respectively. Sixty-six screws (6.5%) penetrated the anterior wall by an average of 1.8 mm (range 0.2–10.5 mm). Thus, 73% screws were accurate within the pedicle.
Table 1.
Group 1 (curve <90°) patients' details with pre and postoperative Cobb’s angle and screws inserted at each level
| No. | Age (years) | Sex (m/f) | Disease | Cobb’s angle (°) | Screws inserted | |
|---|---|---|---|---|---|---|
| Preop | Postop | |||||
| 1 | 19 | M | CP | 52 | 6 | 30 |
| 2 | 23 | M | CP | 65 | 8 | 28 |
| 3 | 16 | F | CP | 55 | 19 | 31 |
| 4 | 22 | M | CP | 40 | 17 | 16 |
| 5 | 37 | F | CP | 40 | 11 | 28 |
| 6 | 12 | M | DMD | 66 | 28 | 31 |
| 7 | 16 | M | DMD | 83 | 26 | 30 |
| 8 | 14 | M | DMD | 40 | 9 | 32 |
| 9 | 18 | M | DMD | 30 | 17 | 28 |
| 10 | 17 | M | DMD | 81 | 59 | 32 |
| 11 | 10 | M | DMD | 46 | 13 | 30 |
| 12 | 11 | M | DMD | 41 | 3 | 32 |
| 13 | 12 | M | DMD | 55 | 15 | 32 |
| 14 | 12 | M | DMD | 82 | 18 | 32 |
| 15 | 14 | M | DMD | 63 | 19 | 30 |
| 16 | 13 | F | SMA | 82 | 41 | 32 |
| 17 | 9 | F | SMA | 71 | 5 | 32 |
| 18 | 30 | F | SMA | 63 | 33 | 28 |
| 19 | 11 | F | NF | 59 | 21 | 16 |
| 20 | 14 | M | NF | 68 | 39 | 10 |
| 21 | 26 | F | FRACT | 84 | 38 | 24 |
CP Cerebral palsy, DMD Duchenne muscular dystrophy, SMA spinal muscular atrophy, NF neurofibromatosis, FRACT fracture paralysis
Table 2.
Group 2 (curve >90°) patients' details with pre and postoperative Cobb’s angle and screws inserted at each level
| No. | Age (years) | Sex (m/f) | Disease | Cobb’s angle (°) | Screws inserted | |
|---|---|---|---|---|---|---|
| Preop | Postop | |||||
| 1 | 25 | M | CP | 108 | 76 | 20 |
| 2 | 32 | M | CP | 120 | 78 | 30 |
| 3 | 21 | M | CP | 108 | 39 | 23 |
| 4 | 21 | M | CP | 121 | 47 | 28 |
| 5 | 22 | M | CP | 96 | 50 | 26 |
| 6 | 17 | M | CP | 90 | 39 | 26 |
| 7 | 28 | F | DMD | 150 | 74 | 27 |
| 8 | 15 | M | DMD | 102 | 28 | 28 |
| 9 | 14 | M | DMD | 100 | 38 | 32 |
| 10 | 18 | F | SMA | 108 | 30 | 32 |
| 11 | 13 | F | SMA | 112 | 24 | 31 |
| 12 | 28 | F | SMA | 92 | 55 | 20 |
| 13 | 14 | F | SMA | 130 | 65 | 32 |
| 14 | 34 | M | POLIO | 102 | 76 | 23 |
| 15 | 44 | F | POLIO | 120 | 78 | 15 |
| 16 | 43 | F | POLIO | 93 | 44 | 32 |
CP Cerebral palsy, DMD Duchenne muscular dystrophy, SMA spinal muscular atrophy
Table 3.
Total inserted, displaced and within-safe margin screws at each level
| Level | Medially displaced screws | Laterally displaced screws | Anteriorly displaced screws | Med + Lat displaced | Total inserted | Accuracy % | Within- safe zone | Safety (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | ||||||
| T1 | 1 | 1 | 1 | 2 | 2 | ||||||||||||
| T2 | 1 | 1 | 6 | 7 | 6 | 1 | 15 | 43 | 42 | ||||||||
| T3 | 1 | 1 | 8 | 1 | 1 | 1 | 13 | 47 | 46 | ||||||||
| T4 | 7 | 3 | 6 | 5 | 4 | 21 | 58 | 55 | |||||||||
| A | 10 | 4 | 1 | 20 | 13 | 11 | 2 | 1 | 49 | 150 | 67.3 | 145 | 96.6 | ||||
| T5 | 7 | 7 | 1 | 7 | 5 | 1 | 5 | 28 | 63 | 54 | |||||||
| T6 | 8 | 3 | 5 | 1 | 5 | 1 | 22 | 62 | 54 | ||||||||
| T7 | 3 | 2 | 6 | 4 | 5 | 1 | 20 | 67 | 60 | ||||||||
| T8 | 8 | 1 | 7 | 4 | 3 | 3 | 1 | 23 | 69 | 65 | |||||||
| B | 26 | 13 | 1 | 25 | 14 | 14 | 10 | 1 | 93 | 261 | 64.3 | 233 | 89.2 | ||||
| T9 | 8 | 1 | 1 | 3 | 3 | 2 | 16 | 68 | 64 | ||||||||
| T10 | 8 | 2 | 4 | 4 | 2 | 2 | 1 | 18 | 72 | 68 | |||||||
| T11 | 9 | 1 | 4 | 5 | 1 | 1 | 1 | 20 | 68 | 66 | |||||||
| T12 | 4 | 2 | 1 | 1 | 1 | 8 | 5 | 4 | 3 | 22 | 70 | 61 | |||||
| C | 27 | 6 | 1 | 1 | 10 | 20 | 11 | 9 | 5 | 76 | 278 | 72.6 | 259 | 93.1 | |||
| Thoracic | 63 | 23 | 3 | 1 | 55 | 47 | 25 | 30 | 7 | 2 | 217 | 689 | 68.5 | 637 | 92.4 | ||
| L1 | 1 | 1 | 1 | 8 | 1 | 3 | 2 | 1 | 12 | 67 | 65 | ||||||
| L2 | 2 | 4 | 3 | 2 | 1 | 4 | 1 | 12 | 67 | 64 | |||||||
| L3 | 6 | 2 | 5 | 1 | 3 | 3 | 1 | 17 | 69 | 64 | |||||||
| L4 | 2 | 1 | 2 | 2 | 2 | 4 | 1 | 9 | 70 | 67 | |||||||
| L5 | 1 | 1 | 2 | 2 | 4 | 3 | 6 | 47 | 45 | ||||||||
| Lumbar | 12 | 4 | 2 | 13 | 16 | 7 | 2 | 18 | 5 | 3 | 1 | 56 | 320 | 82.5 | 305 | 95.3 | |
| Total | 75 | 27 | 5 | 1 | 68 | 63 | 32 | 2 | 48 | 12 | 5 | 1 | 273 | 1009 | 72.9 | 942 | 93.3 |
A = T1 + T2 + T3 + T4; B = T5 + T6 + T7 + T8; C = T9 + T10 + T11 + T12
Of the 689 screws placed into the thoracic spine, a total of 217 screws (31.5%) were displaced either medially or laterally, which shows that 68.5% screws were accurately placed within pedicle. Ninety screws (13%) perforated the medial pedicle wall; 127 screws (18%) perforated the lateral pedicle wall and 39 screws (5.6%) perforated anterior wall. Of the 217 misplaced screws, 165 screws (76%) were within the safe zone, comprising 92.4% (637/689) safety of placement.
Of the 320 screws placed into the lumbar spine, a total of 56 screws (18%) were displaced either medially or laterally, which shows that 82% screws were accurately placed within pedicle. Eighteen screws (6%) perforated the medial pedicle wall; 38 screws (12%) perforated the lateral pedicle wall and 27 screws (8%) perforated anterior wall. Of the 56 misplaced screws, 41 screws (73%) were within the safe zone; comprising 95.3% (305/320) safety of placement.
Comparing the screw placement according to severity of curve, 71 and 84% screws were accurately placed within pedicle with overall accuracy of 75% for group 1; and 64 and 80% screws were accurately placed within pedicle with overall accuracy of 69% for group 2. While considering safe placement, 94.8 and 91.2% screws were within the safe zone (P = 0.35, paired t test), respectively, for groups 1 and 2 (Table 1).
Comparing the screw placement in different thoracic regions, 49, 93 and 76 screws were displaced either medially or laterally in the upper, middle and lower thoracic regions with an accuracy of 67, 64 and 72%, respectively (Table 3). Similarly when it was compared in group 1 and group 2, it showed an accuracy of 66, 70 and 71%, respectively, in group 1 (Table 4; P = 0.17), while it was 72, 56 and 68% accurate in upper, middle and lower thoracic levels, respectively, in group 2 (Table 5; P = 0.02). Overall accuracy of pedicle screw placement was 71 and 64% in group I and group 2, respectively, which was statistically not significant (P = 0.13).
Table 4.
Total inserted, displaced and within-safe margin screws at each level in group 1
| Level | Medially displaced screws | Laterally displaced screws | Anteriorly displaced screws | Med + Lat displaced | Total inserted | Accuracy (%) | Within- safe zone | Safety (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | ||||||
| T1 | 0 | 0 | 0 | ||||||||||||||
| T2 | 1 | 5 | 5 | 2 | 1 | 11 | 28 | 28 | |||||||||
| T3 | 1 | 1 | 4 | 1 | 7 | 34 | 33 | ||||||||||
| T4 | 7 | 1 | 4 | 3 | 4 | 15 | 36 | 35 | |||||||||
| A | 9 | 1 | 1 | 13 | 9 | 6 | 1 | 33 | 98 | 66.3 | 96 | 97.9 | |||||
| T5 | 4 | 2 | 3 | 3 | 1 | 4 | 13 | 37 | 34 | ||||||||
| T6 | 1 | 3 | 1 | 2 | 1 | 7 | 36 | 34 | |||||||||
| T7 | 1 | 1 | 3 | 2 | 3 | 1 | 10 | 36 | 32 | ||||||||
| T8 | 3 | 7 | 1 | 2 | 2 | 13 | 37 | 35 | |||||||||
| B | 9 | 3 | 16 | 7 | 8 | 8 | 43 | 146 | 70.5 | 135 | 92.4 | ||||||
| T9 | 4 | 1 | 1 | 1 | 7 | 40 | 38 | ||||||||||
| T10 | 2 | 1 | 2 | 2 | 2 | 1 | 9 | 42 | 39 | ||||||||
| T11 | 5 | 1 | 4 | 2 | 1 | 12 | 42 | 41 | |||||||||
| T12 | 2 | 1 | 5 | 4 | 2 | 1 | 12 | 38 | 33 | ||||||||
| C | 13 | 3 | 1 | 6 | 10 | 7 | 3 | 2 | 40 | 162 | 75.3 | 151 | 93.2 | ||||
| Thoracic | 31 | 7 | 1 | 1 | 35 | 26 | 15 | 17 | 3 | 116 | 406 | 71.4 | 382 | 94 | |||
| L1 | 1 | 1 | 1 | 3 | 1 | 1 | 1 | 6 | 39 | 38 | |||||||
| L2 | 2 | 2 | 1 | 2 | 1 | 1 | 7 | 38 | 36 | ||||||||
| L3 | 2 | 1 | 5 | 2 | 8 | 39 | 38 | ||||||||||
| L4 | 2 | 1 | 2 | 2 | 1 | 5 | 38 | 37 | |||||||||
| L5 | 1 | 1 | 3 | 1 | 2 | 24 | 23 | ||||||||||
| Lumbar | 7 | 2 | 1 | 10 | 5 | 3 | 9 | 3 | 1 | 1 | 28 | 178 | 84.2 | 172 | 96.6 | ||
| Total | 38 | 9 | 2 | 1 | 45 | 31 | 18 | 26 | 6 | 1 | 1 | 144 | 584 | 75.3 | 554 | 94.8 | |
A = T1 + T2 + T3 + T4; B = T5 + T6 + T7 + T8; C = T9 + T10 + T11 + T12
Table 5.
Total inserted, displaced and within-safe margin screws at each level in group 2
| Level | Medially displaced screws | Laterally displaced screws | Anteriorly displaced screws | Med + Lat displaced | Total inserted | Accuracy (%) | Within- safe zone | Safety (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | <2 mm | 2.1–4.0 mm | 4.1–6.0 mm | >6 mm | ||||||
| T1 | 1 | 1 | 1 | 2 | 2 | ||||||||||||
| T2 | 1 | 1 | 2 | 4 | 4 | 15 | 14 | ||||||||||
| T3 | 4 | 1 | 1 | 4 | 15 | 15 | |||||||||||
| T4 | 2 | 2 | 2 | 6 | 22 | 20 | |||||||||||
| A | 1 | 3 | 7 | 4 | 6 | 1 | 15 | 54 | 72.2 | 51 | 94.4 | ||||||
| T5 | 3 | 5 | 1 | 4 | 2 | 1 | 15 | 26 | 20 | ||||||||
| T6 | 7 | 3 | 2 | 3 | 15 | 26 | 20 | ||||||||||
| T7 | 2 | 1 | 3 | 2 | 2 | 10 | 31 | 28 | |||||||||
| T8 | 5 | 1 | 3 | 1 | 1 | 1 | 10 | 32 | 30 | ||||||||
| B | 17 | 10 | 1 | 9 | 7 | 6 | 2 | 1 | 50 | 115 | 56.5 | 98 | 85.2 | ||||
| T9 | 4 | 1 | 2 | 2 | 2 | 9 | 28 | 26 | |||||||||
| T10 | 4 | 1 | 2 | 2 | 1 | 1 | 9 | 30 | 29 | ||||||||
| T11 | 4 | 3 | 1 | 8 | 26 | 25 | |||||||||||
| T12 | 2 | 2 | 1 | 1 | 3 | 1 | 2 | 2 | 10 | 30 | 26 | ||||||
| C | 14 | 3 | 1 | 4 | 10 | 4 | 6 | 3 | 36 | 114 | 68.4 | 106 | 92.9 | ||||
| Thoracic | 32 | 16 | 2 | 20 | 21 | 10 | 14 | 3 | 2 | 101 | 283 | 64.3 | 255 | 90.1 | |||
| L1 | 5 | 1 | 2 | 1 | 6 | 28 | 27 | ||||||||||
| L2 | 2 | 2 | 1 | 3 | 5 | 29 | 28 | ||||||||||
| L3 | 4 | 1 | 1 | 3 | 1 | 1 | 9 | 30 | 26 | ||||||||
| L4 | 1 | 1 | 2 | 2 | 4 | 32 | 30 | ||||||||||
| L5 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 4 | 23 | 22 | |||||||
| Lumbar | 5 | 2 | 1 | 3 | 11 | 4 | 2 | 9 | 3 | 1 | 28 | 142 | 80.2 | 133 | 93.6 | ||
| Total | 37 | 18 | 3 | 23 | 32 | 14 | 2 | 23 | 6 | 3 | 129 | 425 | 69.6 | 388 | 91.2 | ||
A = T1 + T2 + T3 + T4; B = T5 + T6 + T7 + T8; C = T9 + T10 + T11 + T12
The average preoperative and postoperative Cobb’s angle measured was 82° and 34°, respectively, with 58% correction rate. The same in group 1 was 60° and 19° with 68% correction rate and in group 2 was 110° and 53° with 52% correction rate. None of the patient in the study group deteriorated neurologically after the surgery. By comparing the preoperative and postoperative functional status by WHO criteria [44], 20 (54%) patients improved functionally by at least grade one and also exhibited better satisfaction by their caretakers.
Discussion
Transpedicular stabilization has become an established method for instrumentation of the thoracic and lumbar spine because of its immediate rigidity, better coronal and sagittal correction and shorter fusion length in scoliosis surgery when compared to the other instrumentation techniques [1, 39]. Pedicle screw fixation of the thoracic spine is technically difficult with a high risk of potential complications such as neurologic, vascular and visceral injuries, associated with misplaced pedicle screws [7, 8, 12, 15, 16]. It also impairs the pull out strength [43, 46] of the implants and increases the chances of implant failure. Brown et al. [7] suggested there should be a considerable learning curve for using the pedicle screws in scoliosis surgery to avoid the complications. In our present study, we did not include initially the ten patients operated for neuromuscular scoliosis with pedicle screw instrumentation and considered them as learning curve although we were doing the surgery for adolescent idiopathic scoliosis regularly. Many morphometric cadaver studies have been performed to analyze the anatomic variability of the thoracic and lumbar spine [9, 13, 14]. Smallest pedicle diameters have been noted between vertebral bodies T4 and T7 with a minimum of 3.7 mm at T5 level [3]. In our study, we have also determined the diameter of the pedicle screw to put preoperatively on CT scan to put the screw sized 5.5–6.5 mm, 5.0–5.5 mm, 4.0–5.0 mm and 3.5–4.5 mm in lumbar, lower thoracic (T9–T12), middle thoracic (T5–T8) and upper thoracic (T1–T4) pedicles, respectively. Using epidural contrast, Reynolds et al. demonstrated radiographic evidence of more than 2 mm of lateral epidural space from T7 to L4. Gertzbein and Robbins [19] in their study included 71 thoracic screws between T8 and T12 with a 26% incidence of medial cortical penetration of up to 8 mm with only two minor neurologic injuries. They hypothesized a 4-mm safe zone of medial encroachment, which included 2 mm epidural space and 2 mm subarachnoid space. Lateral wall penetration or lateral extrapedicular screw placement of up to 6 mm resulting from the intentional use of the in-out-in technique was also considered acceptable, especially in the upper and middle thoracic spine where pedicle diameters typically measure only 4–5 mm. Considering the narrow margin of error [2, 26] in pedicular screw placement, we considered those screws within the safe zone which were displaced by <2 mm on medial side and by <4 mm on lateral side.
In previous studies, rate of pedicle-wall perforation varied between 1.5 and 43% [2, 8, 11, 18, 20, 22, 29, 30, 36, 37]. Most studies have shown usually rates of misplacement between 28 and 43% and only a few studies have shown rates less than 5% [2]. We have found similar findings (27% pedicle perforations) reported to the literature.
Various techniques are being used to detect pedicle screw misplacement including guide pins into the pedicles, intraoperative C-arm image intensifier; direct visualization of the medial wall after laminotomy, 3D fluoroscopy, CT-based computer assisted navigational systems and advanced intraoperative neurologic monitoring [2, 4, 11, 20, 29]. Image-guided techniques result in high cost, expensive equipment and prolonged operating time. In spite of all these advances, studies using the free-hand pedicle screw insertion technique have also shown the lower rates of pedicle wall perforation in experienced hands [22, 40, 41]. We use this technique in our hospital for surgical correction of scoliosis. Various postoperative investigations such as radiogram, CT scan or MRI have been described to measure the accuracy of pedicle screws, which suggests CT scan as a more reliable method over radiogram [17], so we analyzed our study with postoperative CT scan.
Suk et al. [41] reported only 67 screw malposition (1.5%) in 48 patients treated for idiopathic and congenital scoliosis with a deformity correction of 69% using postoperative radiogram. Brown et al. [7] found a safe placement of 93.8% in thoracic pedicle screw fixation using postoperative CT scan with free-hand technique, mainly in idiopathic scoliosis and Scheurmann kyphosis. Belmont et al. [2] reported 99% accuracy in thoracic pedicle screw fixation within the safe zone and concluded higher accuracy using fluoroscopic guided in-out-in technique, but the rate of breaching the pedicle wall was 43% in his study. In our present study, we found an overall accuracy of 73% within the pedicle and a safety of 93% within the safe zone.
Vaccaro et al. [42] demonstrated a 23% medial cortical perforation with a mean spinal canal compromise of 5 mm in a cadaveric study without the use of fluoroscopy. The percentages of screw misplacement between the various levels in the thoracic spine also did not vary much as expected. The narrowest diameters of pedicles are found between T3 and T7 and a higher percentage of screw misplacement is expected at these levels, but in this study, they did not show figures as expected. In our study, considering the different levels in the thoracic spine, the displacement rate was 33, 36 and 27 with a safety of 96, 89 and 93% in the upper, middle and lower thoracic regions, respectively, which were statistically significant. The probable reason for that might be the narrow pedicle size in mid thoracic level that has been reported in the literature. Kuklo et al. [25] reported 96.3% safety in putting pedicle screws in patients with curves >90° and concluded that even in large magnitude curves, thoracic pedicle screws can be placed safely. We also compared misplacement of pedicle screws depending on the severity of deformity, and did not fiund significant (P = 0.35, Chi-Square test) difference. We think evaluating screw placement in different thoracic levels and according to severity of curve would be a positive part of this study.
In this study, complete neurological examination cannot be done in patients with neuromuscular scoliosis who were either uncooperative as in cerebral palsy or only sensory testing was available as in DMD or SMA. Hence, we could not correlate the radiological findings with clinical findings but there was no gross functional deterioration postoperatively. This might be the criticism for the study; however, this is the first study measuring the accuracy and safety of pedicle screw in neuromuscular scoliosis population which might be helpful for future studies. Recently Bogler et al. [4] reported that electrical conductivity measuring system using Pediguard may provide a simple, safe and sensitive method of detecting pedicle breeches during the procedure, even with free-hand technique. We also feel that use of this system with free-hand pedicle screw instrumentation would definitely be helpful to surgeons and would increase the accuracy and safety of this procedure (Figs. 1, 2, 3, 4, 5, 6, 7).
Fig. 1.
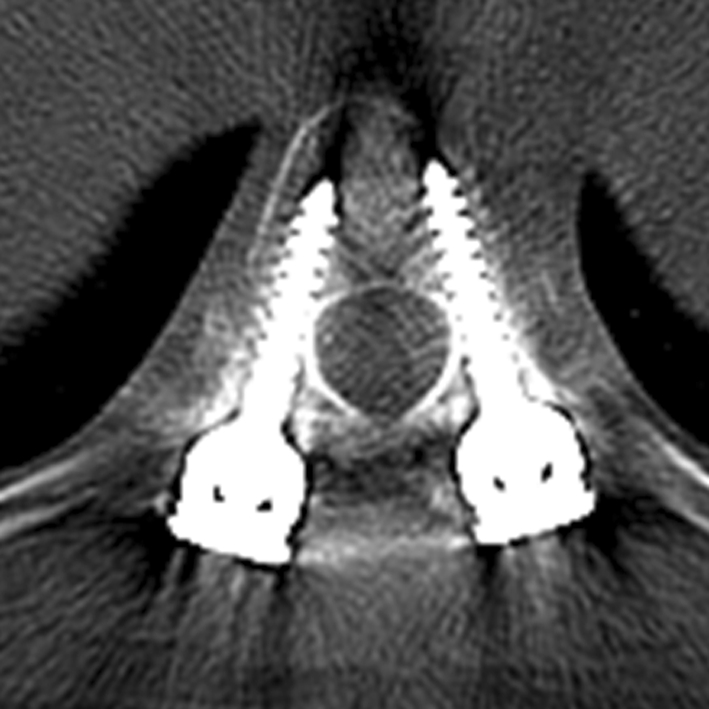
Screws fully contained within the pedicle and body
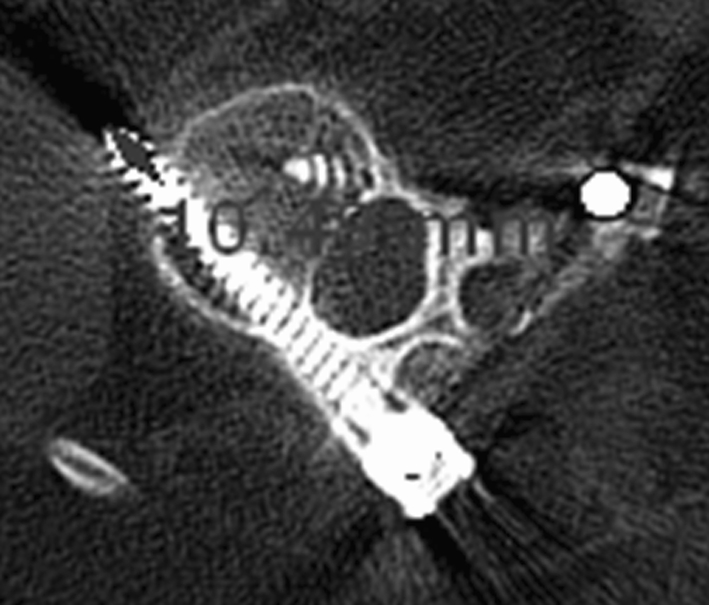
Fig. 2.

Medially displaced screw encroaching the canal by 3.74 mm (considered as potentially at risk)
Fig. 3.

Screw laterally displaced out of the pedicle by 4.27 mm
Fig. 4.

Screws displaced medially and laterally by 2.5 mm
Fig. 5.

Screw penetration of the the anterior cortex by 1.3 mm
Fig. 6.

Screw penetration medially by 1.6 mm (considered in safe zone)
Fig. 7.
Screw penetration anteriorly by 10.4 mm. There were no signs of neurological or vascular injuries and the purchase was good, so it was not removed
Conclusion
Pedicle screw fixation with free-hand technique in neuromuscular scoliosis population appears to be an accurate and safe procedure as in idiopathic scoliosis or other reports in the literature.
Acknowledgments
Conflict of interest statement Each author certifies that he has no commercial associations (e.g., consultancies, stock ownership, equity interests, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Barr CJ, Schuette AM, Emans JB. Lumbar pedicle screw versus hooks. Spine. 1997;22:1369–1379. doi: 10.1097/00007632-199706150-00016. [DOI] [PubMed] [Google Scholar]
- 2.Belmont PJ, Klemme WR, Dhawan A, Polly DW. In vivo accuracy of thoracic pedicle screws. Spine. 2001;26(21):2340–2346. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 3.Berlet GC, Boubez G, Gurr KR, et al. The USS pedicle hook system: a morphometric analysis of its safety in the thoracic spine. J Spinal Disord. 1999;12:234–239. [PubMed] [Google Scholar]
- 4.Bogler C, Kelleher MO, McEvoy L, et al. Electrical conductivity measurement: a new technique to detect iatrogenic initial pedicle perforation. Eur Spine J. 2007;16:1919–1924. doi: 10.1007/s00586-007-0409-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boucher HH. A mehtod of spinal fusion. J Bone Joint Surg Br. 1959;41:248–259. doi: 10.1302/0301-620X.41B2.248. [DOI] [PubMed] [Google Scholar]
- 6.Broom MJ, Banta JV, Renshaw TS. Spinal fusion augmented by luque-rod segmental instrumentation for neuromuscular scoliosis. J Bone Joint Surg Am. 1989;71:32–44. [PubMed] [Google Scholar]
- 7.Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke Kathy RN. Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine. 1998;23(14):1566–1571. doi: 10.1097/00007632-199807150-00012. [DOI] [PubMed] [Google Scholar]
- 8.Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine. 1996;21:1320–1324. doi: 10.1097/00007632-199606010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Cinotti G, Gumina S, Ripani M, et al. Pedicle instrumentation in the thoracic spine. A morphometric and cadaveric study for placement of screws. Spine. 1999;24:654–658. doi: 10.1097/00007632-199904010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Chung KJ, Suh SW, Desai S, Song HR (2007) Ideal entry point for the thoracic pedicle screw during the free hand technique. Int Orhtop Apr 17 (epub ahead of print) [DOI] [PMC free article] [PubMed]
- 11.Danesh-Clough T, Taylor P, Hodgson B, Walton M. The use of evoked EMG in detecting misplaced thoracolumbar pedicle screws. Spine. 2001;26(12):1313–1316. doi: 10.1097/00007632-200106150-00008. [DOI] [PubMed] [Google Scholar]
- 12.Dvorak M, MacDonald S, Gurr KR, Bailey SI, Haddad RG. An anatomic, radiographic and boimechanical assessment of extrapedicular screw fixaiton in thoracic spine. Spine. 1993;18:1689–1694. doi: 10.1097/00007632-199309000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Ebraheim NA, Jabaly G, Xu R, Yeasting RA. Anatomic relations of the thoracic pedicle to adjacent neural structures. Spine. 1997;22:1553–1557. doi: 10.1097/00007632-199707150-00002. [DOI] [PubMed] [Google Scholar]
- 14.Ebraheim NA, Xu R, ahmad M, Yeasting RA. Projection of the thoracic pedicle and its morphometric analysis. Spine. 1997;22:233–238. doi: 10.1097/00007632-199702010-00001. [DOI] [PubMed] [Google Scholar]
- 15.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine. 1993;18:2231–2239. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Faraj AA, Webb JK. Early complications of spinal pedicle screw. Eur Spine J. 1997;6:324–326. doi: 10.1007/BF01142678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferrick MR, Kowalki JM, Simmons ED. Reliability of roentgenogram evaluation of pedicle screw position. Spine. 1997;22(11):1249–1252. doi: 10.1097/00007632-199706010-00016. [DOI] [PubMed] [Google Scholar]
- 18.Fisher CG, Sahajpal V, Keynan O, Boyd M, Graeb D, Baily C, et al. Accuracy and safety of pedicle screw fixation in thoracic spine trauma. J Neurosurg Spine. 2006;5:520–526. doi: 10.3171/spi.2006.5.6.520. [DOI] [PubMed] [Google Scholar]
- 19.Gertzbein SD, Robbins SE. Accuracy of pedicle screw placemment in vivo. Spine. 1990;15:11–15. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Girardi FP, Cammisa FP, Sandhu HS, Alvarez L. The placement of lumbar pedicle screws using computerised steriotactic guidance. J Bone Joint Surg Br. 1999;81-B(5):825–829. doi: 10.1302/0301-620X.81B5.9244. [DOI] [PubMed] [Google Scholar]
- 21.Hamill C, Lenke L, Bridwell K, Chapman M, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine patients with idiopathic scoliosis: Is it warranted? Spine. 1996;21:1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 22.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: Is it safe? Spine. 2004;29(3):333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 23.Krag MH, Weaver DL, Beynnon BD, Haugh LD. Morphometry of the thoracic and lumbar spine related to transpedicular screw placement for surgical spinal fixation. Spine. 1988;13:27–32. doi: 10.1097/00007632-198801000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Krag MH, Beynnon BD, Pope MH, Frymoyer JW, Haugh LD, Weaver DL. An internal fixator for posterior application to short segments of the thoracic, lumbar or lumbosacral spine. Design and testing. Clin Orthop Relat Res. 1986;203:75–98. [PubMed] [Google Scholar]
- 25.Kuklo TR, Lenke LG, O’Brien MF, Lehman RA, Jr, Schroeder TM. Accuracy and efficacy of thoracic pedicle screws in curves more than 90 degrees. Spine. 2005;30:222–226. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 26.Kuntz C, 4th, Maher PC, Levine NB, Kurokawa R. Prospective evaluation of thoracic pedicle screw placement using fluoroscopic imaging. J Spinal Disord Tech. 2004;17:206–208. doi: 10.1097/00024720-200406000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22(19):2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 28.Liljenquist UR, Link TM, Halm HF. Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Spine. 2000;25(10):1247–1253. doi: 10.1097/00007632-200005150-00008. [DOI] [PubMed] [Google Scholar]
- 29.Louis-Philippe A, Karsten L, Michael P, Hartmut Z, Hubert L. Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar and sacral spine. Spine. 2000;25(5):606–614. doi: 10.1097/00007632-200003010-00012. [DOI] [PubMed] [Google Scholar]
- 30.Marty Z, Michael B, Christian K, Joachim L, Christian K, Leonard B. Accuracy of pedicle screw placement in thoracic spine fractures—part II: a retrospective analysis of 278 pedicle screws using computed tomographic scans. Eur J Trauma. 2004;30:241–247. [Google Scholar]
- 31.Masferrer R, Gomez CH, Karahalios DG, Sonntag VK. Efficacy of pedicle screw fixation in the treatment of spinal instability and failed back surgery: a 5 years review. J Neurosurg. 1998;89:371–377. doi: 10.3171/jns.1998.89.3.0371. [DOI] [PubMed] [Google Scholar]
- 32.Rampersaud YR, Foley KT, Shen AC, et al. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle insertion. Spine. 2000;25:2637–2645. doi: 10.1097/00007632-200010150-00016. [DOI] [PubMed] [Google Scholar]
- 33.Rampersaud YR, Simon DA, Folry KT. Accuracy requirements for image-guided spinal pedicle screw placement. Spine. 2001;26(4):352–359. doi: 10.1097/00007632-200102150-00010. [DOI] [PubMed] [Google Scholar]
- 34.Roy-Camille R, Saillant G, Mazel C. Plating of thoracic, thoracolumbar and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986;17:147–159. [PubMed] [Google Scholar]
- 35.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Ortop. 1988;203:7–17. [PubMed] [Google Scholar]
- 36.Sapkas GS, Papadakis SA, Stathakopoulos DP, et al. Evaluation of pedicle screw position in thoracic and lumbar spine fixation using plain radiographs and computed tomography. A prospective study of 35 patients. Spine. 1999;24:1926–1929. doi: 10.1097/00007632-199909150-00011. [DOI] [PubMed] [Google Scholar]
- 37.Schhwarzenbach O, Berlemann U, Jost B, Visarius H, Arm E, Langlotz F, et al. Accuracy of computer-assisted pedicle screw placement: An in vivo computed tomography analysis. Spine. 1997;22(4):452–458. doi: 10.1097/00007632-199702150-00020. [DOI] [PubMed] [Google Scholar]
- 38.Steib JP, Dumas R, Mitton D, Skalli W. Surgical correction of scoliosis by in situ contouring: a derotation analysis. Spine. 2004;29(2):193–199. doi: 10.1097/01.BRS.0000107233.99835.A4. [DOI] [PubMed] [Google Scholar]
- 39.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparision of Cotrel–Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 40.Suk SI, Lee CK, Kim W, Chung Y, Park Y. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. doi: 10.1097/00007632-199506000-00012. [DOI] [PubMed] [Google Scholar]
- 41.Suk SI, Kim WJ, Lee SM, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26(18):2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 42.Vaccaro AR, Rizzolo SJ, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part II: an anatomic and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 43.Weinstein J, Rydevik B, Rauschning W. Anatomic technical considerations of pedicle screw fixation. Clin Orthop Relat Res. 1992;284:34–46. [PubMed] [Google Scholar]
- 44.World Health Organization (2001) International classification of impairment, activity and participation. World Health Organization, Geneva, Switzerland, ICIDH-2
- 45.Zeiller SC, Lee J, Lim M, Vaccaro AR. Posterior thoracic segmental pedicle screw instrumentation: evolving methods of safe and effective placement. Neurol India. 2005;53(4):458–465. doi: 10.4103/0028-3886.22613. [DOI] [PubMed] [Google Scholar]
- 46.Zindrick MR, Wiltse LL, Widell EH, et al. A biomechanical study of intrapedicular screw fixation in the lumbosacral spine. Clin Ortop. 1986;203:99–111. [PubMed] [Google Scholar]


