Abstract
Recent epidemiologic studies suggest that uric acid predicts the development of new-onset kidney disease, but it is unclear whether uric acid is an independent risk factor. In this study, data from 21,475 healthy volunteers who were followed prospectively for a median of 7 yr were analyzed to examine the association between uric acid level and incident kidney disease (estimated GFR [eGFR] <60 ml/min per 1.73 m2). After adjustment for baseline eGFR, a slightly elevated uric acid level (7.0 to 8.9 mg/dl) was associated with a nearly doubled risk for incident kidney disease (odds ratio 1.74; 95% confidence interval 1.45 to 2.09), and an elevated uric acid (≥9.0 mg/dl) was associated with a tripled risk (odds ratio 3.12; 95% confidence interval 2.29 to 4.25). These increases in risk remained significant even after adjustment for baseline eGFR, gender, age, antihypertensive drugs, and components of the metabolic syndrome (waist circumference, HDL cholesterol, blood glucose, triglycerides, and BP). In a fully adjusted spline model, the risk for incident kidney disease increased roughly linearly with uric acid level to a level of approximately 6 to 7 mg/dl in women and 7 to 8 mg/dl in men; above these levels, the associated risk increased rapidly. In conclusion, elevated levels of uric acid independently increase the risk for new-onset kidney disease.
The incidence of ESRD and concomitantly the number of patients on renal replacement therapy are increasing steadily.1–3 Established cardiovascular risk factors are associated with ESRD, hypertension and diabetes being the leading causes.1–3 Uric acid (UA) is strongly associated with renal failure and cardiovascular disease4,5 and is particularly common in people with hypertension and metabolic syndrome, associated with its metabolic abnormalities (e.g., dyslipidemia, insulin resistance). In humans, hyperuricemia has been found to be a risk factor for hypertension6,7 and, moreover, for proteinuria in rats,8,9 leading to the suggestion that this should promote initial kidney damage or its progression.10
Recent epidemiologic and experimental evidence suggests a role for UA not only as a marker of reduced kidney function and an independent cardiovascular risk factor11 but also as a causal risk factor for the development and progression of renal disease.5,9,12 Two large epidemiologic studies demonstrated that UA was a major predictor for the development of incident renal disease,13,14 but none of these studies evaluated the amount of its real role as an independent risk factor. Furthermore, hyperuricemia is associated with a greater incidence of ESRD.15 Findings from experimental animal and cell biologic studies support the suggested nephrotoxicity of elevated UA levels: UA plays a role in platelet adhesiveness16; hyperuricemia may be one of the key mechanisms for the activation of the renin-angiotensin and cyclooxygenase-2 systems in progressive renal disease, which could be mediated by its effect to upregulate angiotensin-1 receptors on vascular smooth muscle cells17,18; oxonic acid induced–hyperuricemia induced systemic hypertension, glomerular hypertrophy/hypertension, afferent arteriolar sclerosis, and macrophage infiltration in the rat kidney8; hyperuricemia induced arteriolopathy of preglomerular vessels, which impairs the autoregulatory response of afferent arterioles, resulting in glomerular hypertension, and lumen obliteration induced by vascular wall thickening produces severe renal hypoperfusion19; direct entry of UA into both endothelial and vascular smooth muscle cells results in local inhibition of endothelial nitric oxide levels, stimulation of vascular smooth muscle cell proliferation, and stimulation of vasoactive and inflammatory mediators.20
The aim of this study was to provide epidemiologic evidence for hyperuricemia as a potential independent risk factor for the development of new-onset kidney disease; therefore confounder models using mixed-effect models with increasing levels of UA were fitted. The data file of the Vienna Health Screening Project was used for analysis.14
RESULTS
Baseline characteristics stratified by the clinically predefined UA groups are shown in Table 1: The reference group, UA <7.0 mg/dl; the slightly elevated UA group (SEUAG), UA = 7.0 to 8.9 mg/dl; and the elevated UA group (EUAG), UA ≥9.0 mg/dl. With increasing UA groups, we observed lower GFR, higher age, the widely known gender differences, higher waist circumference, higher triglycerides, lower HDL cholesterol, higher fasting serum glucose, higher mean arterial BP (MAP), and higher antihypertensive drug use.
Table 1.
Baseline characteristics, stratified by clinically defined UA groupsa
| Characteristic | UA Groups (mg/dl)
|
P for Trend | ||
|---|---|---|---|---|
| <7.0 | 7.0 to 9.0 | >9.0 | ||
| Sample size (n) | 19,466 | 1821 | 188 | |
| GFR (ml/min per 1.73 m2; mean ± SD) | 100 ± 20 | 93 ± 17 | 90 ± 26 | <0.01 |
| Male gender (%) | 55.40 | 79.00 | 93.60 | <0.01 |
| Age (yr) | 42.2 ± 12.0 | 45.5 ± 12.1 | 48.8 ± 12.4 | <0.01 |
| Waist circumference (cm) | 82 ± 11 | 91 ± 11 | 95 ± 12 | <0.01 |
| Triglycerides (mg/dl) | 113 ± 58 | 176 ± 69 | 256 ± 99 | <0.01 |
| HDL (mg/dl) | 62 ± 16 | 51 ± 13 | 48 ± 12 | <0.01 |
| Fasting serum glucose (mg/dl) | 86 ± 12 | 93 ± 13 | 100 ± 17 | <0.01 |
| MAP (mmHg) | 95 ± 10 | 101 ± 10 | 107 ± 11 | <0.01 |
| Antihypertensive drug use (%) | 2.94 | 6.42 | 8.51 | <0.01 |
| β Blocker (%) | 1.55 | 3.29 | 3.72 | |
| ACEI (%) | 0.97 | 2.47 | 2.13 | |
| Calcium antagonist (%) | 0.31 | 0.44 | 0.53 | |
| Diuretic (%) | 0.11 | 0.22 | 2.13 | |
| Alcohol consumption | ||||
| >3 drinks/wk (%) | 13.40 | 14.50 | 15.40 | 0.11 |
| ≤3 drinks/wk (%) | 86.60 | 85.50 | 84.60 | |
| Proteinuria (≥ +) (%) | 8.30 | 7.50 | 9.00 | 0.46 |
ACEI, angiotensin-converting enzyme inhibitor.
Ascertainment of Confounders
Baseline variables were selected as confounders when they were significantly associated with the exposure variable at baseline (Table 1), as well as significantly and causally related with the development of stage 3 chronic kidney disease (CKD).21,22 The following confounders were detected: baseline estimated glomerular filtration rate (GFRb), gender, age, log-HDL cholesterol, log-triglycerides, waist circumference, fasting glucose (spline), MAP (spline), and antihypertensive drug use.
Ascertainment of the Relationship between UA Levels and the Development of stage 3 CKD by Stepwise Adjustment
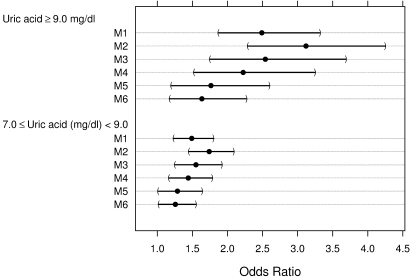
The unadjusted odds ratio (OR) was 1.49 (95% confidence interval [CI] 1.23 to 1.80) in the SEUAG and 2.49 (95% CI 1.87 to 3.32) in the EUAG. After adjustment for GFRb, OR increased to 1.74 (95% CI 1.45 to 2.09) in the SEUAG and to 3.12 (95% CI 2.29 to 4.25) in the EUAG. Additional adjustment for gender and age decreased OR to 1.55 (95% CI 1.25 to 1.92) in the SEUAG and to 2.54 (95% CI 1.75 to 3.69) in the EUAG. Further adjustment for the metabolic factors of the metabolic syndrome (MF) decreased OR to 1.44 (95% CI 1.17 to 1.78) in the SEUAG and to 2.22 (95% CI 1.52 to 3.25) in the EUAG. Continuing the additional adjustment for MAP remarkably decreased OR to 1.29 (95% CI 1.01 to 1.64) in the SEUAG and to 1.76 (95% CI 1.20 to 2.59) in the EUAG. Final adjustment for antihypertensive drug use decreased OR to 1.26 (95% CI 1.02 to 1.55) in the SEUAG and to 1.63 (95% CI 1.18 to 2.27) in the EUAG (Figure 1). Effect decomposition concerning the influence of UA levels on the development of stage 3 CKD resulted in 35% of residual unexplained odds in the SEUAG and 30% in the EUAG, respectively.
Figure 1.
Stepwise adjusted OR for development of a GFR < 60 ml/min per 1.73 m2 depending on UA group. OR (points) with 95% CI (bars) were calculated by logistic mixed-effect models with increasing adjustment from model M1 to model M6. Reference group was UA <7.0 mg/dl. The SEUAG was defined as 7.0 to 8.9 mg/dl and the EUAG as UA >9.0 mg/dl. M1, unadjusted; M2, adjusted for GFR at baseline; M3, additionally adjusted for age and gender (sum-to-zero-constraints); M4, additionally adjusted for the MF (waist circumference, fasting glucose [natural cubic spline], HDL [log-transformed], triglycerides [log-transformed]); M5, additionally adjusted for MAP (natural cubic spline); and M6, additionally adjusted for antihypertensive drug use.
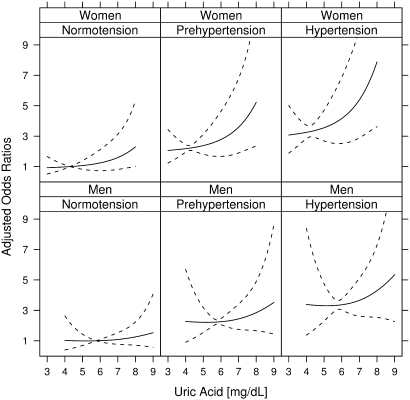
Effects of increasing UA levels, modeled by splines, stratified by gender and hypertension groups,23 and adjusted for the remaining identified confounders, are plotted: The influence of UA levels on OR for the development of a GFR <60 ml/min per 1.73 m2 is roughly linear until approximately 6 to 7 mg/dl in women and 7 to 8 mg/dl in men. Subsequently, OR increase rapidly (Figure 2).
Figure 2.
OR for development of a GFR <60 ml/min per 1.73 m2 depending on UA levels (natural cubic splines) compared with mean UA levels (4.2 mg/dl for women and 5.9 mg/dl for men); stratified for gender and hypertension groups23 adjusted for GFRb, age, waist circumference, fasting glucose (natural cubic spline), HDL (log-transformed), triglycerides (log-transformed), and antihypertensive drug use. Dashed lines denote 95% CI. Hypertension groups: normal BP, systolic <120 mmHg and diastolic <80 mmHg; prehypertension, systolic 120 to 139 mmHg or diastolic 80 to 89 mmHg; hypertension, systolic ≥140 mmHg or diastolic ≥90 mmHg.23
DISCUSSION
A few studies have found that hyperuricemia is associated with an increased risk for new-onset kidney disease,13,14 but this association could be confounded by some metabolic factors and other risk factors that were not included in these previous studies. A confounder model was performed to provide epidemiologic evidence for UA as a possible independent risk factor for the development of incident kidney disease.21
The unadjusted OR was 1.49 in the SEUAG and 2.49 in the EUAG, which represents the predictive strength of elevated UA for the development of new-onset kidney disease, but this does not allow causal interpretation.
GFRb was considered as the crucial confounder variable, because elevated serum UA levels usually are associated with defects of UA transport in the nephron when kidney function worsens.24 Adjustment of UA for GFRb in the respective UA groups allows examination of different UA levels at a GFR that is held constant in the statistical model; therefore, a possible detrimental effect of UA on kidney function can be investigated independent of the individual GFR. After adjustment of UA for GFRb, OR increased by 17% in the SEUAG and by 25% in the EUAG. This result suggests a direct or indirect (mediated) toxic effect of UA on the development of stage 3 CKD.22
Additional adjustment for gender and age decreased OR by 11% in the SEUAG and by 19% in the EUAG. Gender differences of UA levels are widely known. We used sum-to-zero constraints for the factor gender in all models. The interpretation of gender concerning the outcome should be done retentively as discussed in detail elsewhere.14 As generally known, kidney function decreases with aging.25,26
The American Heart Association defines the metabolic syndrome (MS) by the variables waist circumference, serum triglycerides, HDL cholesterol, fasting serum glucose, and BP.27 In this analysis, the MF and BP were analyzed separately. UA is suggested as a major determinant of the MS, and the prevalence of the MS increases substantially with increasing levels of serum UA levels.28,29 Moreover, numerous studies demonstrated that hyperuricemia is an independent risk factor for hypertension.10 Recently, one study could not confirm this association when UA levels were adjusted for several MF.30 Further adjustment for the MF in this study decreased OR by 8% in the SEUAG and by 13% in the EUAG. Additional adjustment for MAP and antihypertensive drug treatment decreased OR by 13% in the SEUAG and remarkably by 27% in the EUAG.
Alcohol consumption did not fulfill the criteria as a confounder variable in this study. Keeping in mind the generally known influence of alcohol consumption on UA levels as well as its possible protective influence on the outcome, we found an evaluation of its influence interesting.13 In this study, the effect was weak, the OR for the outcome variable remained nearly unchanged, and confounding could have been explained by only 2% in both elevated UA groups.
Proteinuria is a strong predictor for a decline in GFR and correlated with other covariates. Because its lack of association with UA, proteinuria did not fulfill the criteria as a potential confounder (Table 1). As expected, the calculated effect was weak: OR for the outcome variable remained nearly unchanged, and potential confounding could have been explained by only 4% in both elevated UA groups. Noteworthy, evidence for an association of hyperuricemia and greater proteinuria is weak and is provided only in rats.9
After adjustment of both elevated UA groups for all detected confounders (Figure 1), OR for the development of CKD stage 3 were 1.26 (95% CI 1.18 to 2.27) in the SEUAG and 1.63 (95% CI 1.18 to 2.27) in the EUAG. Moreover, effect decomposition showed that 35% of the influence of UA on the development of CKD stage 3 could not be explained by confounding in the SEUAG and 30% in the EUAG, respectively. Even when residual confounding remains, strong support for an independent (directly toxic) effect of elevated UA levels on the development of new-onset kidney disease exists. This major finding is supported by a differing recent study.31
These findings are supported by small clinical pilot trials in which allopurinol therapy decreased serum UA levels in patients with hyperuricemia and mild to moderate kidney disease. Its use was safe and helped preserve kidney function during 12 mo of therapy compared with control subjects.32 Moreover, indirect evidence was given when hyperuricemia decreased GFR in other trials, when allopurinol treatment was withdrawn.33,34
An additional interesting topic of this study was the examination of the interaction between elevated UA levels and hypertension concerning the development of stage 3 CKD; therefore, a model using splines for UA, stratified by gender and the defined BP groups adjusted for all detected confounders, was fitted (Figure 2).23 The influence of UA levels on OR for development of new-onset kidney disease is roughly linear until approximately 6 to 7 mg/dl in women and 7 to 8 mg/dl in men. Subsequently, OR increase rapidly. The observed effect of increased UA levels on OR for development of new-onset kidney disease is increasing rapidly with each hypertension group and is more pronounced in women, a finding that is supported by studies concerning the early detection of renal disease and its progression to ESRD.15,35 Noteworthy, mild hyperuricemia was shown to be associated with renal damage in untreated primary hypertension.36 All in all, we assume that the findings of the stratified spline analyses seem to be substantial from a public health viewpoint, because in the general adult population the prevalence of prehypertension and hypertension is approximately 60%,37 and the prevalence of hyperuricemia (defined as UA >6.0 mg/dl in women and UA >7.0 mg/dl in men) is approximately 17%.38 Future clinical trials might clarify whether lower UA treatment points should be entertained in this context.
The Vienna Health Screening Project is an ongoing study including new participants continuously. The sample size increased by approximately 20% compared with our previous analysis.14 A very comparable data set was used for this study; therefore, the detailed examination of UA must be considered as a post hoc analysis, but statistical power should be high enough to provide correct results. Moreover, this study may have been subject to a survival bias because participants had to attend follow-up examinations and 599 participants dropped out. Although unlikely (they showed very similar baseline data compared with the study cohort), it is possible that those individuals may have developed more severe risk factors after the baseline examination and could have had rapid disease progression in the interim. This may have led to underestimation of some findings. In addition using eGFR calculated by the Modification of Diet in Renal Disease (MDRD) formula to represent the severity of kidney disease is not a gold standard method, and correction of routine measured creatinine to “MDRD creatinine” is mandatory.39 Nevertheless, imprecision and bias are greater at a higher GFR, limiting the accuracy of classification in the mildly decreased GFR group.40 This may have led to an underestimation of GFR. A minor limitation is that the influence of the different antihypertensive drugs as confounder variables was not examined separately because of low use; however, antihypertensive drug use was a weak confounder. Especially diuretics are associated with an increase in serum UA levels, and it is suggested that raising UA levels can stimulate the renin-angiotensin-system accelerating the development of renal microvascular disease and thereby predispose the patient to renal disease progression.12 Thereupon, in humans, asymptomatic hyperuricemia induced progression of CKD and worsened control of hypertension, an effect that was blocked by angiotensin-converting enzyme inhibitor treatment when allopurinol therapy was withdrawn,34 which could not be examined in this study. Moreover, accurate UA-lowering therapy is safe and does not deteriorate kidney function32; therefore, it seems unlikely that accurate UA-lowering therapy can substantially confound the relationship between UA and development of new-onset kidney disease.
Hyperuricemia was revealed as an important possibly independent risk factor for new-onset kidney disease. The relation between UA and new-onset kidney disease cannot be explained solely by the detected confounder variables. Clinical trials of UA lowering are needed to evaluate the causal inference of UA on the progression of CKD.
CONCISE METHODS
Study Sample
The Vienna Health Screening Project is an ongoing prospective cohort study that began in January 1990. Because of the study protocol, participants are further included continuously, and, thus, the sample is growing; the study sample and design have been described in detail elsewhere.14 Until January 2007, 22,441 seemingly healthy volunteers (46.5% women, age range 20 to 84 yr, men 20 to 89 yr) performed a baseline examination at any time within the study period. For investigation of volunteers at an earlier stage of kidney disease, 367 participants with a baseline GFR <60 ml/min per 1.73 m2 (calculated by the abbreviated MDRD equation) were excluded. Another 599 participants dropped out after the baseline examination; they did not show systematic differences in their baseline characteristics compared with the total cohort. The median follow up period was 7 yr (interquartile range 4 to 11); the mean follow-up period was 7.4 ± 3.9 yr. A total of 21,475 baseline examinations and 73,015 follow-up examinations (a median of three follow-up examinations) were used for analyses. Moreover, a total of 417 missing values were imputed by their respective means. All participants gave informed consent according to the Declaration of Helsinki.
Ascertainment of Risk Factors
Assessment of medical history, habits in daily living, and physical examination were performed by specially trained general practitioners and study nurses with respect to the study protocol; chemical laboratory analyses are described in detail elsewhere, too.14 MAP (mmHg) was calculated by the generally used empiric equation: MAP (mmHg) = diastolic BP + (systolic BP − diastolic BP)/3. CKD was classified using the National Kidney Foundation CKD classification.22
Ascertainment of UA
UA was measured by an enzymatic method (UA-plus; Roche Diagnostics GmbH, Vienna, Austria) on the Hitachi (Hitachi Europe Ltd., Maidenhead, United Kingdom) 917 clinical chemistry analyzer. UA groups were clinically defined: The reference group, UA <7.0 mg/dl; the SEUAG, UA = 7.0 to 8.9 mg/dl; and the EUAG, UA ≥9.0 mg/dl. This classification was chosen because normal UA levels are usually defined as UA <7.0 mg/dl and UA-lowering drugs in hyperuricemia can be supported only in serum UA levels ≥9.0 mg/dl20,41; therefore, this classification was preferred to a classification in, for example, quartiles for its clinical presentiveness.20,41
Ascertainment of Kidney Function
Creatinine was measured by means of a kinetic Jaffé method on the Hitachi 917 clinical chemistry analyzer. Measurements, calibration, standardization, and validation were performed in a single laboratory throughout the 17-yr study period. Kidney function was estimated by GFR,25,42,43 which was calculated by the abbreviated MDRD equation:GFR (ml/min per 1.73 m2) = 186.3 × serum creatinine−1.154 × age−0.203 × (0.742 if female).25 Because the MDRD formula is sensitive to the creatinine assay method, the following correction formula was necessary (because of our creatinine assay method used) to convert measured creatinine to “MDRD creatinine”: MDRD creatinine (mg/dl) = −0.215 + 1.08 × measured creatinine.39,44
Statistical Analysis
The outcome of interest was the development of kidney disease defined as a decrease of GFR <60 ml/min per 1.73 m2 (i.e., stage 3 CKD) at the follow-up examinations. The exposure variables were the SEUAG (UA 7.0 to 8.9 mg/dl) and the EUAG (UA ≥9.0 mg/dl) compared with the reference group (UA <7.0 mg/dl).
For each baseline variable, its association with the exposure variable and its relation to the outcome were analyzed.14,21 Log-transformation was used for blood lipids. Natural cubic splines with three knots were used for glucose and MAP to adjust accurately for blood glucose levels in the normal, impaired fasting glucose, and diabetic ranges,45 as well as for MAP in the normotensive, prehypertensive, and hypertensive ranges.23 Trends of the exposure variable concerning the UA groups were determined by one-way ANOVA for continuous variables and χ2 tests for categorical variables (Table 1). Relations with the outcome were determined by logistic mixed-effect models,46 adjusted for gender and age: All baseline variables that were used in the confounder model were modeled by fixed effects. Correlation introduced by multiple follow-up visits of participants was modeled by random effects. Visual inspection of the linearity hypothesis was performed. Variables that were both associated with the exposure and deemed to be causally related to the outcome were included as potential confounders.21
To estimate the influence of UA on the outcome, first the crude relationship for UA and the development of new-onset kidney disease was calculated by logistic mixed-effect models. Second, this model was stepwise adjusted for the identified confounders. Third, the total influence of UA on the outcome was split into an independent effect, as well as parts that can be attributed to the confounding variables. This effect decomposition was performed by calculating percentage of explained excess odds from the fitted models, with the model adjusted for GFRb as the reference.21 Sum-to-zero constraints were used for the factor gender in all models.47 Finally, a model using splines for UA, stratified by gender and predefined BP groups adjusted for all detected confounders, was included.23
All continuous data are presented as means ± SD. Categorical data are presented as percentages. All data analysis was done in the R environment for statistical computing, version 2.6, using the “lme4 library” and “the spline library.”48–50
DISCLOSURES
None.
Acknowledgments
This study was financially supported by the Medizinische Forschungsgesellschaft Donaustadt and by grants from the Austrian Science Fund (FWF P-18325) and the Austrian Academy of Science (OELZELT EST370/04) to Rainer Oberbauer.
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Uric Acid Levels Increase Risk for New-Onset Kidney Disease,” on pages 2251–2253.
REFERENCES
- 1.US Renal Data System: USRDS 2003 Annual Data Report, Bethesda, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2003
- 2.Stengel B, Billon S, Van Dijk PC, Jager KJ, Gekker FW, Simpson K, Briggs JD: Trends in the incidence of renal replacement therapy for end stage renal disease in Europe, 1990–1999. Nephrol Dial Transplant 18: 1824–1833, 2003 [DOI] [PubMed] [Google Scholar]
- 3.Kramar R, Oberbauer R: Austrian Dialysis and Transplantation Registry (OEDTR)-Annual Report 2007. Austrian Society of Nephrology. Available at: http://www.nephro.at/oedr2006/oedr2006.htm. Accessed June 25, 2008
- 4.Tomita M, Mizuno S, Yamanaka H, Hosoda Y, Sakuma K, Matuoka Y, Odaka M, Yamaguchi M, Yosida H, Morisawa H, Murayama T: Does hyperuricaemia affect mortality? A prospective cohort study of Japanese male workers. J Epidemiol 10: 403–409, 2000 [DOI] [PubMed] [Google Scholar]
- 5.Nagakawa T, Kang DH, Feig D, Sanchez-Lozada LG, Srinivas TR, Sautin Y, Ejaz AA, Segal M, Johnson RJ: Unearthing uric acid: An ancient factor with recently found significance in renal and cardiovascular disease. Kidney Int 69: 1722–1725, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Nagahama K, Inoue T, Iseki K, Touma T, Kinjo K, Ohya Y, Takishita S: Hyperuricaemia as a predictor of hypertension in a screened cohort in Okinawa, Japan. Hypertens Res 27: 835–841, 2004 [DOI] [PubMed] [Google Scholar]
- 7.Sundstrom J, Sullivan J, D'Agostino RB, Levey D, Kannel WB, Vasan RS: Relations of serum uric acid to longitudinal blood pressure tracking and hypertension incidence. Hypertension 45: 28–33, 2005 [DOI] [PubMed] [Google Scholar]
- 8.Nakagawa T, Mazzali M, Kang DH, Sanchez-Lozada LG, Herrara-Acosta J, Johnson RJ: Uric acid: A uremic toxin? Blood Purif 24: 67–70, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Kang DH, Nakagawa T, Feng L, Watanabe S, Han L, Mazzali M, Truong L, Harris R, Johnson RJ: A role of uric acid in the progression of renal disease. J Am Soc Nephrol 13: 2888–2897, 2002 [DOI] [PubMed] [Google Scholar]
- 10.Heinig M, Johnson RJ: Role of uric acid in hypertension, renal disease, and metabolic syndrome. Cleve Clin J Med 73: 1059–1064, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Fang J, Alderman MH: Serum uric acid and cardiovascular mortality: The NHANES I epidemiologic follow-up study, 1971–1992. JAMA 283: 2404–2410, 2000 [DOI] [PubMed] [Google Scholar]
- 12.Johnson RJ, Segal MS, Srinivas T, Ejaz A, Mu W, Roncal C, Sànchez-Lozada LG, Gersch M, Rodriguez-Iturbe B, Kang DH, Acosta JH: Essential hypertension, progressive renal disease, and uric acid: A pathogenetic link? J Am Soc Nephrol 16: 1909–1919, 2005 [DOI] [PubMed] [Google Scholar]
- 13.Domrongkitchaiporn S, Sritara P, Kitiyakara C, Stitchantrakul W, Krittaphol V, Lolekha P, Cheepudomwit S, Yipintsoi T: Risk factors for development of decreased kidney function in a Southeast Asian population: A 12-year cohort study. J Am Soc Nephrol 16: 791–799, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Obermayr RP, Temml C, Knechtelsdorfer M, Gutjahr G, Kletzmayr J, Heiss S, Ponholzer A, Madersbacher S, Oberbauer R, Klauser-Braun R: Predictors of new-onset decline in kidney function in a general middle-European population. Nephrol Dial Transplant 23: 1265–1273, 2008 [DOI] [PubMed] [Google Scholar]
- 15.Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Takishita S: Significance of hyperuricaemia as a risk factor for developing ESRD in a screened cohort. Am J Kidney Dis 44: 642–650, 2004 [PubMed] [Google Scholar]
- 16.Glinsberg MH, Kozin F, O'Malley M, McCarty DJ: Release of platelet constituents by monosodium urate crystals. J Clin Invest 60: 999–1007, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kang DH, Nakagawa T: Uric acid and chronic renal disease: Possible implication of hyperuricaemia on progression of renal disease. Semin Nephrol 25: 43–49, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Kang D-H, Yu ES, Park J-E, Yoon K-I, Kim M-G, Johnson RJ: Uric acid induced C-reactive protein expression via upregulation of angiotensin type 1 receptors in vascular endothelial cells and smooth muscle cells [Abstract]. J Am Soc Nephrol 14: 136A, 2003 [Google Scholar]
- 19.Sanchez-Lozada LG, Tapia E, Santamaria J, Avila-Casado C, Soto V, Nepomuceno T, Ródriguez-Iturbe B, Johnson RJ, Herrara-Acosta J: Mild hyperuricaemia induces vasoconstriction and maintains glomerular hypertension in normal and remnant kidney rats. Kidney Int 67: 234–247, 2005 [DOI] [PubMed] [Google Scholar]
- 20.Johnson RJ, Kang DH, Feig D, Kivlighn S, Watanabe S, Tuttle KR, Rodriguez-Iturbe B, Herrara-Acosta J, Mazzali M: Is there a pathogenic role for uric acid in hypertension, and cardiovascular and renal disease? Hypertension 41: 1183–1190, 2003 [DOI] [PubMed] [Google Scholar]
- 21.Szklo M, Nieto FJ, eds.: Epidemiology Beyond the Basics, 2nd Ed., Boston, Jones and Bartlett Publishers, 2007, pp 154–187
- 22.National Kidney Foundation: K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification and stratification. Am J Kidney Dis 39[Suppl 1]: S1–S266, 2002 [PubMed] [Google Scholar]
- 23.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure [published erratum appears in JAMA 290: 197, 2003]. The JNC 7 report. JAMA 289: 2560–2571, 2003 [DOI] [PubMed] [Google Scholar]
- 24.Sica DA, Schoolwerth AC: Handling of organic anions and cations: Excretion of uric acid. In: The Kidney, 7th Ed., edited by Brenner BM, Philadelphia, WB Saunders, 2004, pp 645–649
- 25.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D: A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130: 461–470, 1999 [DOI] [PubMed] [Google Scholar]
- 26.Lindeman RD, Tobin J, Shock NW: Longitudinal studies on the rate of decline in renal function with aging. J Am Geriatr Soc 33: 278–285, 1985 [DOI] [PubMed] [Google Scholar]
- 27.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F, American Heart Association, National Heart, Lung and Blood Institute: Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung and Blood Institute Scientific Statement. Circulation 112: 2735–2752, 2005 [DOI] [PubMed] [Google Scholar]
- 28.Choi HK, Ford ES: Prevalence of the metabolic syndrome in individuals with hyperuricaemia. Am J Med 120: 442–447, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Tsouli SG, Liberopoulos EN, Mikhailidis DP, Athyros VG, Elisaf MS: Elevated serum uric acid levels in metabolic syndrome: An active component or an innocent bystander? Metabolism 55: 1293–1301, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Forman JP, Choi H, Curhan GC: Plasma uric acid level and risk factor for incident hypertension among men. J Am Soc Nephrol 18: 287–292, 2007 [DOI] [PubMed] [Google Scholar]
- 31.Weiner DE, Tighiouart H, Elsayed EF, Griffith JL, Salem DN, Levey AS: Uric acid and incident kidney disease in the community. J Am Soc Nephrol 19: 1204–1211, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siu YP, Leung KT, Tong MK, Kwan TH: Use of allopurinol in slowing the progression of renal disease through its ability to lower serum uric acid level. Am J Kidney Dis 47: 51–59, 2006 [DOI] [PubMed] [Google Scholar]
- 33.Kanbay M, Ozkara A, Selcoki Y, Isik B, Turgut F, Bavbek N, Uz E, Akzay A, Yigitoglu R, Covic A: Effect of treatment of hyperuricaemia with allopurinol on blood pressure, creatinine clearance, and proteinuria in patients with normal renal functions. Int Urol Nephrol 39: 1227–1233, 2007 [DOI] [PubMed] [Google Scholar]
- 34.Taalat KM, El-Sheikh AR: The effect of mild hyperuricaemia on urinary transforming growth factor beta and the progression of chronic kidney disease. Am J Nephrol 27: 435–440, 2007 [DOI] [PubMed] [Google Scholar]
- 35.Iseki K, Oshiro S, Tozawa M, Iseki C, Ikemiya Y, Takishita A: Significance of hyperuricaemia on the early detection of renal failure in a cohort of screened subjects. Hypertens Res 24: 691–697, 2001 [DOI] [PubMed] [Google Scholar]
- 36.Viazzi F, Leoncini G, Ratto E, Falqui V, Parodi A, Conti N, Derchi LE, Tomolillo C, Deferrari G, Pontremoli R: Mild hyperuricaemia and subclinical renal damage in untreated primary hypertension. Am J Hypertens 20: 1276–1282, 2007 [DOI] [PubMed] [Google Scholar]
- 37.Wang Y, Wang QJ: The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: New challenges of the old problem. Arch Intern Med 164: 2126–2134, 2004 [DOI] [PubMed] [Google Scholar]
- 38.Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN: Uric acid and the development of metabolic syndrome in women and men. Metabolism 57: 845–852, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Biesen W, Vanholder R, Veys N, Verbeke F, Delanghe J, De Bacquer D, Lameire N: The importance of standardization of creatinine in the implementation of guidelines and recommendations for CKD: Implications for CKD management programs. Nephrol Dial Transplant 21: 77–83, 2006 [DOI] [PubMed] [Google Scholar]
- 40.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298: 2038–2047, 2007 [DOI] [PubMed] [Google Scholar]
- 41.Pöllmann G, Kullich W, Klein G: Therapy of hyperuricaemia and gout. Wien Med Wochenschr 147: 382–387, 1997 [PubMed] [Google Scholar]
- 42.Stevens LA, Coresh J, Greene T, Levey AS: Assessing kidney function: Measured and estimated glomerular filtration rate. N Engl J Med 354: 2473–2483, 2006 [DOI] [PubMed] [Google Scholar]
- 43.Coresh J, Stevens LA: Kidney function estimation equations: Where do we stand? Curr Opin Nephrol Hypertens 15: 276–284, 2006 [DOI] [PubMed] [Google Scholar]
- 44.Hallan S, Asberg A, Lindberg M, Johnsen H: Validation of the Modification of Diet in Renal Disease formula for estimating GFR with special emphasis on calibration of the serum creatinine assay. Am J Kidney Dis 44: 84–93, 2004 [DOI] [PubMed] [Google Scholar]
- 45.Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, Nathan D, Palmer J, Rizza R, Saudek C, Shaw J, Steffes M, Stern M, Tuomilehto J, Zimmet P, Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 26: 3160–3167, 2003 [DOI] [PubMed] [Google Scholar]
- 46.Wolfinger R, O'Connell M: Generalized linear mixed models: A pseudo-likelihood approach. J Stat Comput Simul 48: 233–243, 1993 [Google Scholar]
- 47.Chambers J, Hastie T: Statistical Models in S. London, United Kingdom: Chapman & Hall, 1991, pp 32–37
- 48.R Development Core Team: R: A Language Environment for Statistical Computing. Vienna, R Foundation for Statistical Computing, 2007. Available at: http://www.R-project.org. Accessed April 25, 2008
- 49.Bates D: Fitting linear mixed models in R. R-News 5: 27–30, 2005 [Google Scholar]
- 50.Soo Y-W, Douglas M: Multiresponse spline regression. Computational Statistics & Data Analysis 22: 619–631, 1996 [Google Scholar]