Abstract
Objective
Rapid increase in aged population and westernization of lifestyle have modified epidemiological status of stroke. The purpose of this study is to analyze changing trends of stroke epidemiology in South Korea.
Methods
We reviewed retrospectively medical records of 1,124 cases diagnosed as stroke among 54,534 patients who visited the Emergency Medical Center at our hospital from January 1994 to December 1996 (Group A). Also, we evaluated 1,705 cases diagnosed as stroke among 55,381 patients who visited to the same hospital from January 2003 to December 2005 (Group B). The variable features of stroke, such as age, sex, seasonal variation and distribution of stroke subtypes were studied by comparing group A with B.
Results
In group A, hemorrhagic stroke (67.9%) was more prevalent than ischemic stroke (32.1%). However, group B showed that the ratio of hemorrhagic stroke (40.3%) to ischemic stroke (59.6%) has been reversed. The highest incidence of stroke was noted in their sixties and seventies of age in group B, which was older than that of group A. In group A, male ischemic stroke (IS) patients outnumbered female patients (1.26:1). Moreover, this gender disproportion became higher in group B (1.53:1). In group A, the number of male intracerebral hermorrhage (ICH) patients were similar to that of female patients (0.97:1). However, male ICH patients outnumbered female patients in group B (1.23:1). As for subarachnoid hemorrhage (SAH), female patients outnumbered male patients more than two-fold in both groups. Both groups showed that the occurrence of ischemic stroke was highest in summer, but that of hemorrhagic stroke was the highest in winter.
Conclusion
This study showed the changing trends of stroke in its distribution of subtypes. Multicenter prospective study using stroke registry would be required for the determination of national epidemiologic trends.
Keywords: Stroke, Epidemiology, Seasons, South Korea
INTRODUCTION
Cerebral stroke is the second most common cause of death and the leading cause of disability in South Korea.18) South Korea is a rapidly developing country, and its gross national product is ranked currently as the 11th largest in the world. However, regarding stroke mortality, it still retains major problems. The mortality from stroke was recorded as 64.3 per 100,000 deaths in 20051), which was considerably higher than that reported in the Western countries10). There have been many reports on stroke in South Korea, most of which were done at Department of Neurosurgery, Neurology, and Internal Medicine. It is established that hemorrhagic stroke occurs at a relative high rate compared to that of Western societies. In the past, hemorrhagic stroke was more prevalent than ischemic stroke in South Korea21,26). In Far Eastern countries where primary intracerebral hemorrhage is relatively common16), it has even been suggested that a low level of blood cholesterol may predispose subjects to develop hemorrhagic stroke13,28). The increasing prevalence of hypercholesterolemia, which is inversely associated with the risk of hemorrhagic stroke but positively associated with the risk of ischemic stroke in eastern Asian populations8), might have also contributed to the changing pattern of stroke subtypes.
Stroke is not a homogeneous condition but rather a mixture of clinically distinct subtypes that have different etiological and epidemiological characteristics. Although ischemic and hemorrhagic stroke share some common risk factors such as age and hypertension, the population-attributable risks from these individual risk factors vary by stroke subtypes, and thus the prevention strategies are also different. Therefore, from a public health perspective, it is important to understand the incidence and secular trends of stroke subtypes in rapidly developing areas such as South Korea. The purpose of this study is to analyze changing trends of stroke epidemiology.
MATERIALS AND METHODS
We retrospectively reviewed medical records of 1,124 cases diagnosed as stroke among 54,534 patients who visited the Emergency Medical Center at our institution from January 1994 to December 1996 (Group A). We also studied 1,705 cases diagnosed as stroke among 55,381 patients who visited to the same hospital from January 2003 to December 2005 (Group B). The changing features of stroke, such as age, sex, seasonal variation and distribution of stroke subtypes were studied by comparing group A with B.
The diagnosis and classification of stroke were performed according to a slightly revised version of the one used in the Atherosclerosis Risk in Communities (ARIC) Study12). Briefly, the minimum criteria for a definite or probable stroke diagnosis included evidence of sudden or rapid onset of neurological symptoms lasting for >24 hours or leading to death in the absence of evidence for a nonstroke cause. Exclusions included major brain trauma, neoplasm, coma attributable to metabolic disorders, vasculitis involving the brain, peripheral neuropathy, hematologic abnormalities, or central nervous system infections. Transient ischemic attacks and silent brain infarctions (cases without clinical symptoms and signs) were not included. Stroke subtypes were defined according to published criteria12) and then grouped into 3 major types : ischemic stroke (IS ; including thrombotic brain infarction, cardioembolic stroke, and lacunar infarcts), intracerebral hemorrhage (ICH), or subarachnoid hemorrhage (SAH).
RESULTS
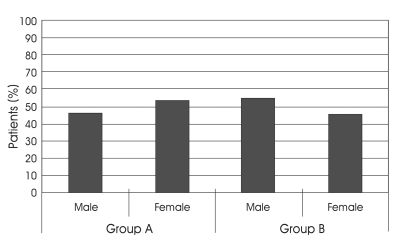
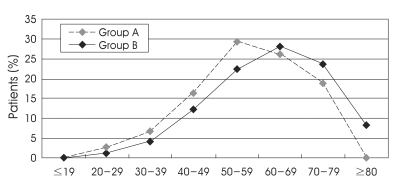
Sex and age distribution
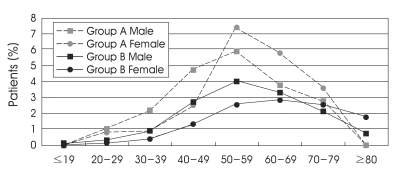
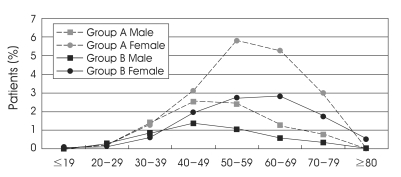
In Group A, we diagnosed 1,124 cases (2.1%) as having stroke among 54,534 patients. There were 522 men (46.4%) and 602 women (53.6%). In Group B, we diagnosed 1,705 cases (3.1%) as having stroke among 55,381 patients. There were more male patients (929, 54.5%) than female patients (776, 45.5%) (Fig. 1). In Group A, the highest incidence of stroke was noted in their fifties (181, 29.4%) and sixties (331, 26.3%). However, the highest incidence of stroke was noted in their sixties (479, 28.1%) and seventies (403, 23.1%) in Group B (Fig. 2). In Group A, their mean age±SD was 56.7±12.70. The mean age of Group B (61.5±13.71)was older than that of group A.
Fig. 1.
Sex distribution.
Fig. 2.
Age distribution.
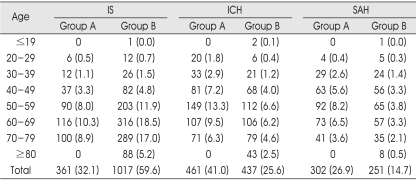
Distribution of stroke subtypes
In Group A, we divided stroke subtypes as follows : IS in 361 patients (32.1%), ICH in 461 (41.0%), and SAH in 302 (26.9%). Hemorrhagic stroke (67.9%) including ICH and SAH was more prevalent than IS (32.1%) in Group A. In Group B, stroke subtypes were divided as follows : IS in 1017 patients (59.6%), ICH in 437 (25.6%), and SAH in 251 (14.7%). Group B showed that the ratio of hemorrhagic stroke (40.3%) to ischemic stroke (59.6%) has been reversed (Table 1).
Table 1.
Distribution of stroke subtypes in Group A and B*
IS: ischemic stroke, ICH: intracerebral hemorrhage, SAH: subarachnoid hemorrhage. *Values represent the number of patients (%).
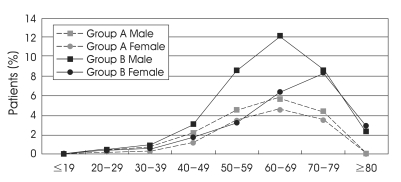
Distribution of ischemic stroke
In Group A, male IS patients outnumbered female patients (1.26:1). Also, this gender disproportion became higher in group B (1.53:1). The mean age of Group B (63.7±12.66) was older than that of group A (60.6±11.78). Fifty-five patients (4.9%) were aged below 50 years (younger age group) in group A. But, there were 121 patients (7.1%) in Group B, which showed that the proportion of IS patients in younger age group increased. Interestingly, male proportion between their fifties and sixties patients in Group B was significantly higher than that of Group A. However, the number of male IS patients over 70 years was similar to that of female in both groups (Fig. 3).
Fig. 3.
Age and sex distribution of ischemic stroke.
Distribution of intracerebral hemorrhage
In Group A, there were slightly more female ICH patients (234, 20.8%) than male patients (227, 20.2%). However, there were more male ICH patients (241, 14.1%) than female patients (196, 11.5%) in Group B. The mean age of Group B (60.0±14.66) was older than that of Group A (54.9±13.02). One hundred thirty-four patients (11.9%) were aged below 50 years (younger age group) in Group A. But, there were 97 patients (5.7%) in Group B, which showed that the proportion of ICH patients in younger age group decreased. The male proportion of younger age group in Group B (68, 70.1%) was higher than that of Group A (88, 65.7%). Male proportion between their fifties and sixties patients in Group B was significantly higher than that of Group A. However, the number of male ICH patients over 70 years was less than that of female in both groups, which may have been due to increase of female senior population (Fig. 4).
Fig. 4.
Age and sex distribution of intracerebral hemorrhage.
Distribution of subarachnoid hemorrhage
In Group A, female SAH patients (208, 18.5%) outnumbered male patients (94, 8.4%) by more than two-fold. Female SAH patients (178, 10.4%) also outnumbered male patients (73, 4.3%) by more than two-fold in Group B. The mean age of Group B (55.1±13.84) was slightly older than that of Group A (54.7±12.23). In younger age group (age below 50), there were slightly more female patients (51, 4.5%) than male (45, 4.0%) in Group A. There were also slightly more female patients (45, 2.6%) than male (41, 2.4%) in Group B. However, there was a striking difference of gender distribution in SAH patients over 50 years in Group A (49:157) and B (32:133) (Fig. 5).
Fig. 5.
Age and sex distribution of subarachnoid hemorrhage.
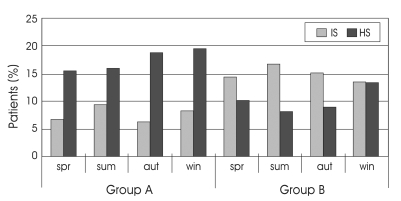
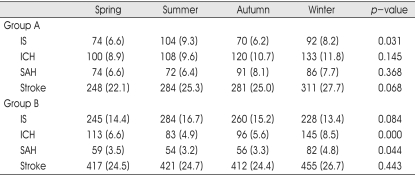
Seasonal distribution of stroke subtypes
The date of onset was split into quartiles based on seasonal trends. The winter quartile was defined as December, January, and February; the spring quartile as March, April, and May; the summer quartile as June, July, and August; and the fall quartile as September, October, and November. The occurence of stroke was increased during winter in both groups, but there was no statistical significance between winter and stroke in Group A (p=0.068) and B (p=0.443). However, seasonal distribution of stroke varied with stroke subtypes. The occurrence of ischemic stroke was highest in summer in both groups, but the occurrence of hemorrhagic stroke (ICH, SAH) was highest in winter (Fig. 6). There was statistical significance between summer and ischemic stroke in Group A (p=0.031), but there was no statistical significance in Group B (p=0.084). There there was no statistical significance between winter and hemorrhagic stroke (ICH, p=0.145; SAH, p=0.368) in Group A, but there was statistical significance in Group B (ICH, p=0.000; SAH, p=0.044) (Table 2).
Fig. 6.
Seasonal distribution of ischemic and hemorrhagic stroke. IS: ischemic stroke, HS: hemorrhagic stroke, spr: spring, sum : summer, au : autumn, win: winter.
Table 2.
Seasonal distribution of stroke subtypes*
IS: ischemic stroke, ICH: intracerebral hemorrhage, SAH: subarachnoid hemorrhage. *Values represent the number of patients (%).
DISCUSSION
With the economic booming in South Korea, Korean populations are rapidly adopting Western lifestyle and dietary habits, including increased energy intake, fat intake, alcohol consumption, decreased physical activity and cigarette smoking. These changes may have resulted in increased prevalence of obesity, hypertension, diabetes, and hypercholesterolemia in Korean people18) and may explain the increasing trend of ischemic stroke as observed in this study. Uncontrolled hypertension and high prevalence of smoking might partially have related to the hemorrhagic stroke predominance among Korean in the past, and the increasing awareness of hypertension control and decrease in cigarette smoking may have contributed to its decrease in the past decade. On the other hand, the increasing prevalence of hypercholesterolemia, which is positively associated with the risk of ischemic stroke, might have also contributed to the changing pattern of stroke subtypes. Also, appropriate treatment for hypertension may help decrease in the incidence of hemorrhagic stroke, and patients who have been exposed to the risk of hemorrhagic stroke are moving to the ischemic stroke group.
The use of neuroimaging techniques makes it easier to identify mild stroke cases and to accurately classify its subtypes. The development of diagnostic tools for stroke diagnosis may potentially contribute to the observed increase of ischemic stroke incidence. However, this cannot explain the decreasing trend of hemorrhagic stroke. On the contrary, the simultaneously increasing use of neuroimaging and decreasing incidence of hemorrhagic stroke suggest a real decline in the incidence of hemorrhagic stroke.
With the rapid aging of Korean populations in the years to come, the public health burden associated with stroke will increase substantially. This will be accompanied by a Westernization of stroke subtype composition probably as a result of the adoption of Western diet and lifestyle by the Korean. These behavioral changes will not only result in more ischemic stroke but also may contribute to increasing incidence of other chronic diseases such as diabetes, cardiovascular diseases, and cancer. Therefore, there is an utmost urgency to face these challenges and to launch appropriate public health campaigns to prevent the occurrence of these chronic diseases.
Our study showed that the ages of peak incidence of stroke moved from fifties and sixties to sixties and seventies. It reveals that age group of stroke has been older, like other studies7,14,15). The reason is, first, that the elderly population has increased in our society and risk group occuring stroke is larger. Second, the overall number of ischemic stroke patients, who are older than hemorrhagic stroke patients, was increased. Third, improved contorol of disease associated with stroke, such as hypertension, might be one factor contributing to older age of stroke patients.
Male preponderance has indeed noted in general stroke population7,14,15,19,31). This study showed that the male proportion of stroke patients increased; the proportion of men was 46.4% in Group A, while it was 54.5% in Group B. This resulted from much higher incidence of ischemic stroke in Group B. Male proportion of ischemic stroke patients increased and that of ICH patients also increased in this study. The prevalence of cigarette smoking in Korean adult males is much higher than that in the United States and European countries19). On the other hand, Korean women rarely smoke. Alchol consumption is also much more prevalent in men than that in women in the general Korean population. Furthermore, Korean men tend to take more salt and less often try to control their hypertension than women17). In contrast to the other subtypes of stroke, female SAH patients outnumbered male patients more than twice in both group A and B. In particular, the trend of increasing prevalence rates with age was significant after the menopause (≥50 years) among females like other report9).
Seasonal variation in stroke has been reported in many countries, and most studies have reported a marked increase in both stroke mortality and the rate of hospital admissions in the winter6,11,20,30). In contrast, no seasonal preponderance was demonstrated in other studies25,27). In our study, the occurrence of ischemic stroke was the highest in summer, but the occurrence of hemorrhagic stroke was the highest in winter. Berginer et al.2) suggested that exposure to heat is likely to cause dehydration, increasing the viscosity of the blood. Also peripheral vasodilatation cause a reduction of blood supply to the cental nervous system during heat exposure. These effects in persons without vascular disease might cause no damage, while in older patients with vascular disease the effects could predispose to thromboembolic episodes. Possible biological mechanisms for an apparent seasonal variation and low temperature relationship to hemorrhagic stroke incidence rates include an increased rate of influenza and respiratory infection morbidity during the winter-time20), vasoconstriction and increased blood pressure at colder temperatures4,12,29), and circannual variation in cortisol levels22). Although many studies suggested significant relationships between seasonal variation and stroke prevalence, others reported no relationship between them. Environmental and acquired factors are thought to have a role in this variation.
CONCLUSION
This study shows the changing trends of stroke in its distribution of subtypes. The incidence of hemorrhagic stroke decreased, but that of ischemic stroke increased. This trend might be due to the westernization of life style and aging of population as well as better control of stroke risk factors in Korea. Multicenter prospective study using stroke registry would be required for the determination of national epidemiologic trends.
References
- 1.Annual Report on the Cause of Death Statistics, 2005. Republic of Korea: National Statistical Office; 2005. [Google Scholar]
- 2.Berginer VM, Goldsmith J, Batz U, Vardi H, Shapiro Y. Clustering of stroke in association with meteorologic factors in the Negev Desert of Israel. Stroke. 1989;20:65–69. doi: 10.1161/01.str.20.1.65. [DOI] [PubMed] [Google Scholar]
- 3.Biller J, Jones MP, Bruno A, Adams HP, Jr, Banwart K. Seasonal variation of stroke-dose it exist? Neuroepidemiology. 1998;7:89–98. doi: 10.1159/000110140. [DOI] [PubMed] [Google Scholar]
- 4.Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. BMJ. 1982;285:919–923. doi: 10.1136/bmj.285.6346.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bronner LL, Kanter DS, Manson JE. Primary prevention of stroke. N Engl J Med. 1995;23:1392–1400. doi: 10.1056/NEJM199511233332106. [DOI] [PubMed] [Google Scholar]
- 6.Chen ZY, Chang SF, Su CL. Weather and stroke in a subtropical area: Ilan, Taiwan. Stroke. 1995;26:569–572. doi: 10.1161/01.str.26.4.569. [DOI] [PubMed] [Google Scholar]
- 7.Chon JS, Chon SI, Park SH, Bask SY, Kim DA. Recent epidemiologic trends of stroke. J Korean Acad Rehab Med. 1998;22:1159–1165. [Google Scholar]
- 8.Eastern Stroke and Coronary Heart Disease Collaborative Research Group. Blood pressure, cholesterol, and stroke in eastern Asia. Lancet. 1998;352:1801–1807. [PubMed] [Google Scholar]
- 9.Epidemiology of Aneurysmal Subarachnoid Hemorrhage in Australia and New Zealand. Incidence and Case Fatality From the Australasian Cooperative Research on Subarachnoid Hemorrhage Study (ACROSS) Stroke. 2000;31:1843–1850. doi: 10.1161/01.str.31.8.1843. [DOI] [PubMed] [Google Scholar]
- 10.Feigin VL, Lawes CMM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- 11.Feigin VL, Nikitin YP, Bots ML, Vinogradova TE, Grobbee DE. A population-based study of the associations of stroke occurrence with weather parameters in Siberia, Russia (1982-1992) Eur J Neurol. 2000;7:171–178. doi: 10.1046/j.1468-1331.2000.00016.x. [DOI] [PubMed] [Google Scholar]
- 12.Hata T, Ogihara T, Maruyama A, Mikami H, Nakamaru M, Naka T, et al. The seasonal variation of blood pressure in patients with essential hypertension. J Hypertens. 1993;11:1267–1274. doi: 10.3109/10641968209060747. [DOI] [PubMed] [Google Scholar]
- 13.Iso H, Jacobs DR, Jr, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the Multiple Risk Factor Intervention Trial. N Engl J Med. 1989;320:904–910. doi: 10.1056/NEJM198904063201405. [DOI] [PubMed] [Google Scholar]
- 14.Kang SD, Jeong JW, Moon BS, Kim JM. Current epidemiological status of cerebrovascular disease. J Korean Neurosurg Soc. 1999;28:509–513. [Google Scholar]
- 15.Kim KT, An JD, Kim BY, Jeong JI, Lee SH, Lee SC. Current epidemiologic status of stroke. J Korean Acad Rehab Med. 2003;27:178–175. [Google Scholar]
- 16.Korean Neurological Association. Epidemiology of cerebrovascular disease in Korea. J Kor Med Sci. 1993;8:281–289. doi: 10.3346/jkms.1993.8.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korean Nutritional Society. Recommended dietary allowances for Koreans. 6th ed. Jun-Ju: Jung-Ang Munhwa; 1995. pp. 75–79. [Google Scholar]
- 18.Korean Statistical Inforamtion Service
- 19.Kwon SU, Kim JS, Lee JH, Lee MC. Ischemic stroke in Korean young adults. Acta Neurol Scand. 2000;101:19–24. doi: 10.1034/j.1600-0404.2000.00004.x. [DOI] [PubMed] [Google Scholar]
- 20.Lanska DJ, Hoffman RG. Seasonal variation in stroke mortality rates. Neurology. 1999;52:984–990. doi: 10.1212/wnl.52.5.984. [DOI] [PubMed] [Google Scholar]
- 21.Moon JS, Park DH, Kim W, Kim BT. Computerized Tomogsaphic Findings and Clinical Observations of Cerebrovascular Accidents. J Korean Med Sci. 1985;28:499–507. [Google Scholar]
- 22.Nyquist PA, Brown RD, Jr, Wiebers DO, Crowson CS, O'Fallon WM. Circadian and seasonal occurrence of subarachnoid and intracerebral hemorrhage. Neurology. 2001;56:190–193. doi: 10.1212/wnl.56.2.190. [DOI] [PubMed] [Google Scholar]
- 23.Rosamod WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, et al. Stroke incidence and survival among middleaged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30:736–743. doi: 10.1161/01.str.30.4.736. [DOI] [PubMed] [Google Scholar]
- 24.Scandinavian Simvastatin Survival Study Group. Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease : the Scandinavian Simvastatin Survival Study. Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 25.Sobel E, Zhang ZX, Alter M, Lai SM, Davanipour Z, Friday G, et al. Stroke in the Lehigh Valley: seasonal variation in incidence rates. Stroke. 1987;18:38–42. doi: 10.1161/01.str.18.1.38. [DOI] [PubMed] [Google Scholar]
- 26.Song HS, Kwon KY, Kim KB. A Clinical Study on CVA with Brain Scan. J Korean Med Sci. 1982;25:1348–1358. [Google Scholar]
- 27.Field TS, Hill MD. Weather, Chinook, and Stroke Occurrence. Stroke. 2002;33:1751–1757. [PubMed] [Google Scholar]
- 28.Ueda K, Hasuo Y, Kiyohara Y, Wada J, Kawano H, Kato I, et al. Intracerebral hemorrhage in a Japanese community, Hisayama: incidence, changing pattern during long-term follow-up, and related factors. Stroke. 1988;19:48–52. doi: 10.1161/01.str.19.1.48. [DOI] [PubMed] [Google Scholar]
- 29.Woodhouse PR, Khaw KT, Plummer M. Seasonal variation in blood pressure and its relation to ambient temperature in an elderly population. J Hypertens. 1993;11:1267–1274. [PubMed] [Google Scholar]
- 30.Wang Y, Levi CR, Attia JR, D'Este CA, Spratt N, Fisher J. Seasonal variation in stroke in the Hunter region, Australia: A 5-year hospitalbased study, 1995-2000. Stroke. 2003;34:1144–1150. doi: 10.1161/01.STR.0000067703.71251.B6. [DOI] [PubMed] [Google Scholar]
- 31.Yoon SJ, Choi KH, Joo BG, Ha SB. Seasonal variation in the occurrence of stroke. J Korean Acad Rehab Med. 1998;22:1166–1172. [Google Scholar]