Abstract
We present a rare case of fracture-dislocation at the level of the first sacral (S1) and second sacral (S2) vertebrae. The S1 was displaced forward into the pelvic cavity and was located just in front of the S2. Because the patient also had extensive neurological injury to the lumbar plexus and instability of the pelvic ring, surgery to stabilize the pelvis and to decompress the lumbar plexus was performed. The surgery was successful and the patient experienced marked improvement in neurological function.
Keywords: Fracture, Dislocation, Sacrum
INTRODUCTION
Transverse fracture of the sacrum is uncommon and accounts for only 2-5% of all sacral fractures1,2,4). Concomitant dislocation of the sacrum, as was seen in our patient, is less common5). In this report, we describe an uncommon case of fracture-dislocation of the sacrum at the S1-S2 level and its operation and treatment, including a review of the literature.
CASE REPORT
A 54-year-old male presented with paraplegia and sensory loss of both lower extremities following a fall injury. On admission, vital signs were normal. He showed decreased sensation over the dorsal aspect and soles of the feet and along the lateral parts of the legs bilaterally. Motor strength was grade 2/5 throughout both lower extremities. The patellar tendon reflex and Achilles tendon reflex were diminished on both sides. In addition, anal sphincter tone and sensation were absent.
Radiographic study was inconclusive. Computerized tomography (CT) showed a complete fracture and dislocation at the S1-S2 level, with anterior displacement of the S1 body into the pelvic cavity just in front of the S2 vertebra. It also showed a fracture of the body and ala of the sacrum (Fig. 1). In addition, soft tissue and bony edemas were seen by magnetic resonance imaging (MRI) (Fig. 2). With the patient in the prone position, the fracture and dislocation site was approached through a midline incision, which showed a complete anterior dislocation of S1 on S2.
Fig. 1.
Initial lateral (A), axial (B), and three dimensional (C) tomography scans of the lumbosacral spine confirmed bilateral longitudinal fractures through the sacral foraminae (A) and forward displacement of the S1 vertebra into the pelvic cavity, just in front of the S2 vertebra (B).
Fig. 2.

Sagittal view of magnetic resonance image showing the fracture and dislocation, and injury of the soft tissue.
Open reduction was attempted, but failed. We could not reduce the dislocated S1 body any further because of the increasing risk of aggravating the patient's neurological injury and worsening his general condition, so wide laminectomies of S1 and S2 were performed instead. During the procedure, dural tearing and serpentine spinal roots were seen. Injury to the sacral nerve roots below S1 was also apparent. Dura was sutured. To achieve rigid fusion, sacropelvic fixation was used (Fig. 3). At the level of the posterior superior iliac spine, both the inner and the outer tables of the ilium were identified, and a screw was inserted into each anterior superior iliac spine on both sides. Another screw was placed just cephalad to each superior gluteal notch. The screws were connected to the longitudinal rod by a connector tunnel. Finally, bone from the right iliac crest and laminectomies was grafted over the sacrum and ileum and along the transverse processes to obtain a fusion (Fig. 4).
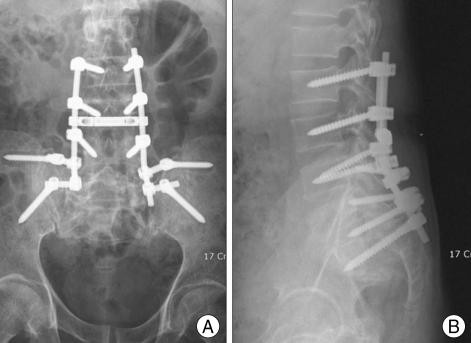
Fig. 3.
Antero-posterior (A) and lateral (B) radiographs after internal fixation with spinal instrumentation.
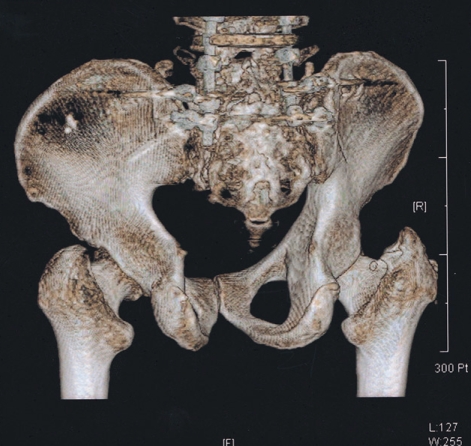
Fig. 4.
3-dimensional computed tomography image demonstrating rods and intrapedicular and intrailiac screws.
The patient's postoperative course was satisfactory, with immediate pain relief of both extremities and gradual improvement in muscle strength after surgery. By the fifth postoperative week, the patient was able to walk with a cane.
DISCUSSION
It has been reported that 15-45% of major pelvic fractures include an associated sacral fracture2,10). In contrast, transverse fractures of the sacrum are uncommon and occurs in only 2-5% of all sacral fractures1,5). Moreover, concomitant sacral dislocation, as was seen in our patient, is extremely rare7,9).
Denis et al.2) have proposed a classification of sacral fractures based on the direction, location, and level of the fracture. Zone I fractures involve the alar region, zone II fractures occur in the sacral foramina area, and zone III fractures occur in the vicinity of the central sacral canal. Zone III fractures are frequently associated with neurological damage and can involve bowel and bladder dysfunction. In their review, Denis et al. also discussed the mechanism of lower lumbar root damage that arises at the upper region of the level of dislocation. The L5 root is usually caught between the displaced lateral sacral fragment and the transverse process of L5, as the alar fragment migrates superiorly and posteriorly. This can result in foot drop as in our patient.
They also stated that the positional relationships between the lumbar spine, the pelvis, and the lower limbs are important. Two major opposing forces combine to produce a sacral fracture : the body weight and the resistance to the ground transmitted through the lower limbs and the pelvis. These two vectors, when merged, produce a rotation at the sacral level that twists the pelvis horizontally and makes the sacrum vertical; this can fracture the sacrum transversely. Based on an experimental study performed on fresh cadaveric specimens, Roy-Camille et al.7) established a classification system for transverse fractures of the upper sacrum. While evaluating the position of the lumbar spine in lordosis or kyphosis at the time of impact, they identified three types of fracture-dislocation : type 1, anterior flexion fracture; type 2, anterior flexion fracture with horizontal posterior displacement; and type 3, extension fracture with anterior displacement and neurological impingement7). According to the classification of Denis et al., our patient's transverse fracture-dislocation was a zone III lesion. Under the system of Roy-Camille et al., it qualifies as a type 3 lesion.
Several surgeons have reported spontaneous neurological recovery in their patients with transverse sacral fracture, and therefore recommend that these fractures be treated nonoperatively3,5). Other have prescribed surgical treatment for this injury when severe neurological deficits are present or when there is instability2,7,8,10). For example, Taguchi et al.10) stated that operative treatment provided mechanical stability, facilitating immediate mobilization and early rehabilitation. However, they also stated that delayed surgery was efficacious in alleviating pain, but not in abolishing the neurological impairment, and early surgery appeared to facilitate neurological improvement.
CONCLUSION
Transverse fracture-dislocation at the S1-S2 level is extremely rare. It can be stabilized by sacropelvic fixation with spinal instrumentation, while an S2 laminectomy can decompress the lumbar plexus and preserve neurological function.
References
- 1.Carl A, Delman A, Engler G. Displaced transverse sacral fractures: a case report, review of the literature, and the CT scan as an aid in management. Clin Orthop. 1985;194:195–198. [PubMed] [Google Scholar]
- 2.Denis F, Davis S, Comfort T. Sacral fractures: an important problem : retrospective analysis of 236 cases. Clin Orthop. 1988;227:67–81. [PubMed] [Google Scholar]
- 3.Ebraheim NA, Biyani A, Salpietro B. Zone III fractures of the sacrum. A case report. Spine. 1996;21:2390–2396. doi: 10.1097/00007632-199610150-00020. [DOI] [PubMed] [Google Scholar]
- 4.Fountain SS, Hamilton RD, Jameson RM. Transverse fractures of the sacrum: a report of six cases. J Bone Joint Surg Am. 1977;59:486–489. [PubMed] [Google Scholar]
- 5.Phelan ST, Jones DA, Bishay M. Conservative management of transverse fractures of the sacrum with neurological features: a report of four cases. J Bone Joint Surg Br. 1991;73:969–971. doi: 10.1302/0301-620X.73B6.1955446. [DOI] [PubMed] [Google Scholar]
- 6.Purser DW. Displaced fracture of the sacrum: report of a case. J Bone Joint Surg Br. 1969;51:346–347. [PubMed] [Google Scholar]
- 7.Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum: suicidal jumper's fracture. Spine. 1985;10:838–845. doi: 10.1097/00007632-198511000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Sapkas G, Makris A, Korres D, Kyratzoulis J, Meleteas E, Antoniadis A. Anteriorly displaced transverse fractures of the sacrum in adolescents: report of two cases. Eur Spine J. 1997;6:342–346. doi: 10.1007/BF01142683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suzuki K, Mochida J. Operative treatment of a transverse fracturedislocation at the S1-S2 Level. J Orthop Trauma. 2001;15:363–367. doi: 10.1097/00005131-200106000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Taguchi T, Kawai S, Kaneko K, Yugue D. Operative management of displaced fractures of the sacrum. J Orthop Sci. 1999;4:347–352. doi: 10.1007/s007760050115. [DOI] [PubMed] [Google Scholar]