Abstract
We experienced a case of giant arachnoid granulation misdiagnosed as dural sinus thrombosis. A 66-year-old woman presented with a one month history of progressive occipital headache. Computed tomography angiography and cerebral angiography showed a round filling defect at the transverse sinus which was speculated as a transverse sinus thrombosis. Anticoagulation therapy was performed to prevent worsening of thrombosis for 2 weeks and then a Gadolinium-enhanced magnetic resonance imaging scan was performed. The filling defect lesion at the transverse sinus revealed a non-enhancing granule with central linear enhancement, which was compatible with giant arachnoid granulation. We checked the intrasinus pressure difference across the lesion the through the dural sinus in order to exclude the lesion as the cause of headache. Normal venous pressure with no significant differential pressure across the lesion was noted. Headache was treated with medical therapy.
Keywords: Giant, Arachnoid granulation, Dural sinus thrombosis
INTRODUCTION
Arachnoid granulations are growth of arachnoid membrane into the dural sinuses through which cerebrospinal fluid (CSF) enters the venous system. Normally, the arachnoid granulation measures a few millimeters, but they may grow sufficiently to partially occlude and enlarge the dural sinus. Also, they rarely cause symptoms from venous hypertension secondary to partial sinus obstruction, making imaging interpretation difficult with dural sinus thrombosis. We present a case of a giant arachnoid granulation involving torcular herophili and the left transverse sinus misdiagnosed as sinus thrombosis. Intrasinus pressure measurement across the lesion was performed to exclude venous hypertension.
CASE REPORT
A 66-year-old woman with hypertension was transferred to our department with a one month history of progressive occipital headache. The neurological and general physical examinations were normal. Contrast-enhanced brain computed tomography (CT) scan showed a filling defect in the right transverse sinus (Fig. 1). CT angiography and cerebral angiography showed a round filling defect in the left transverse sinus and the torcular herophili, which was assumed to be a sinus thrombosis (Fig. 2). The screening test for the coagulation system, such as protein C, S, and coagulation factors were normal and tumor markers were negative. Heparin anticoagulant therapy was performed for 2 weeks. Follow-up CT angiography showed no interval change. Headache wasn't much improved, either. Gadolinium-enhanced brain magnetic resonance imaging (MRI) scan was done and the filling defect lesion revealed a low signal on T1-weighted image (T1WI), a high signal on T2-weighted image (T2WI) and non-enhancing granules with central linear enhancement (Fig. 3). These findings are the differential points of giant arachnoid granulation. Because of the possibility of relative venous obstruction by arachnoid granulation producing venous hypertension and headache, cerebral venography was performed. We checked the intrasinus pressure difference across the lesion through the dural sinus (Fig. 4). The presence of normal venous pressure (~15mmHg) and lack of significant differential pressure across the lesion within all the dural venous limbs (<5mmHg) was revealed excluding the lesion as the cause of headache. The headache was managed with symptomatic treatment.
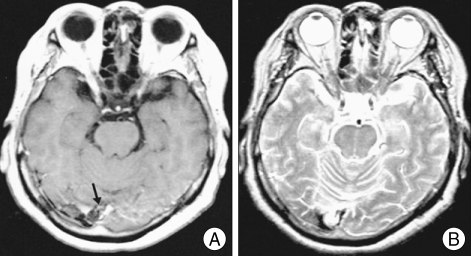
Fig. 1.
Contrast-enhanced brain computed tomography reveals round low density mass within the right transverse sinus.
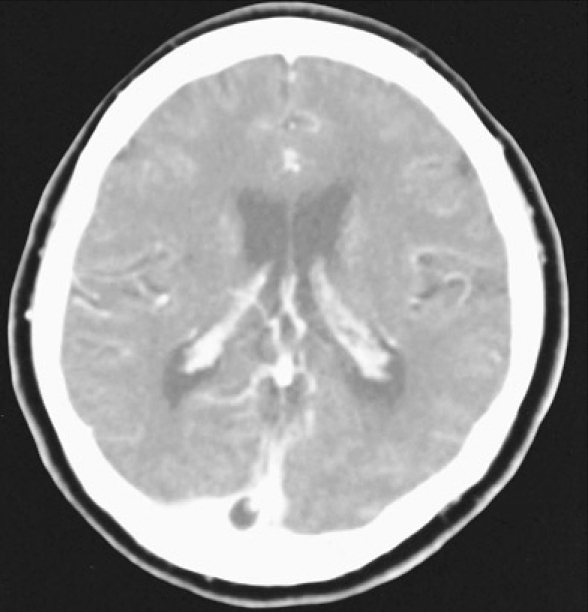
Fig. 2.

Cerebral angiography shows round filling defect at the junction of the torcular herophili and the left transverse sinus.
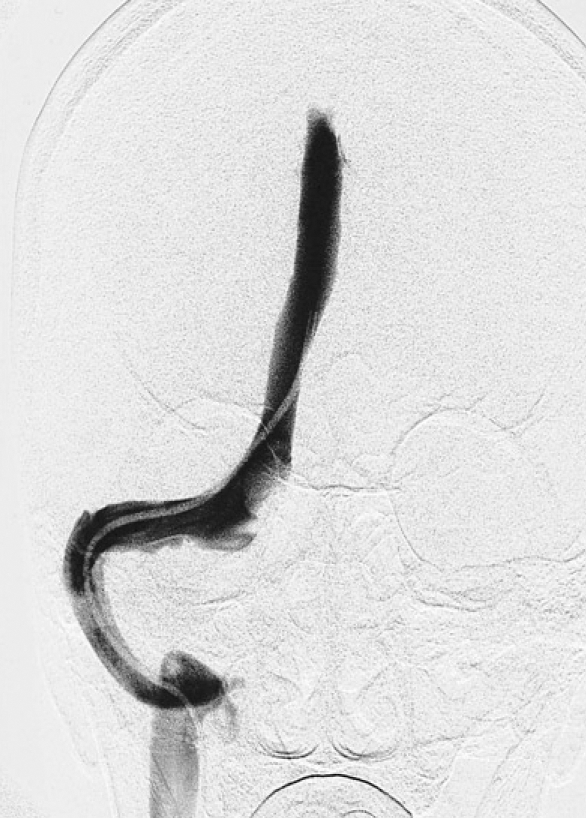
Fig. 3.
A: Gadolinium-enhanced T1-weighted magnetic resonance imaging (MRI) shows central linear enhancement (black arrow) in the low signal mass. B: T2-weighted MRI shows high signal intensity at the lesion.
Fig. 4.
Cerebral venography of the superior sagittal sinus shows a microcatheter transversing through the right venous channel to measure the pressure across the lesion.
DISCUSSION
The growth of arachnoid membrane into the dural sinus (glandulae conglobatae) was first described by Pacchioni2) in 1705. These projections are called arachnoid villi or arachnoid granulation, depending on their size. Arachnoid villi are microscopic, whereas granulation is visible to the naked eye11). They function as a passive filtration system for CSF, providing a pathway from subarachnoid space into the venous system. Arachnoid granulations increase in number and enlarge with age in response to increased CSF pressure from the subarachnoid space and are usually quite conspicuous by 4 years of age5,9). Arachnoid granulations are most commonly seen at the junction between the middle and lateral thirds of the transverse sinuses (92%) near the entry sites of the superficial veins8). We refer to arachnoid granulation as "giant" when it is of sufficient size to fill the lumen of a dural sinus and cause local dilatation or filling defect7).
Although giant arachnoid granulations are sometimes discovered as an incidental finding in the transverse and posterior superior sagittal sinus1,3,10), they rarely cause symptoms of increased intracranial pressure from venous hypertension secondary to partial sinus occlusion1). If symptoms present, intrasinus pressure measurements across the lesion through each dural sinus can be used to determine whether the lesion is causing venous outflow obstruction and venous hypertension7).
In the differential diagnosis of masses within the dural sinus it is important to consider dural sinus thrombosis which is potentially dangerous and needs immediate management5,6). Thrombosis usually involves an entire segment of a sinus or multiple sinuses and can extend to cortical veins, whereas arachnoid granulations produce focal, well-defined nodular defects in the sinuses8). A thrombosed dural sinus has homogenous hyperdensity on unenhanced CT. Arachnoid granulations are never hyperdense on CT or hyperintense on T1WI8,12). The typical MRI findings of dural sinus thrombosis are an iso- to hyperintense blood clot in the sinus on T1WI which is hyperintense on T2WI4). The key MRI features of giant arachnoid granulations are non-enhancing granules with central linear enhancement and surrounding enhancing flowing blood on contrast-enhanced MR venography3). Intrasinus thrombus may show contrast enhancement and occlude venous flow. Focal central linear enhancement in the arachnoid nodule may represent an extension of the endothelium-lined venous sinuses into the fissure of the granulation13). Other diseases including meningioma, inclusion tumor, sinus cavernoma and meningocele14), can be excluded by their characteristic imaging findings.
CONCLUSION
We experienced a case of giant arachnoid granulation misdiagnosed as dural sinus thrombosis. Before diagnosing the sinus thrombosis, giant arachnoid granulation should be considered as a differential diagnosis. MRI is the most useful tool to differentiate giant arachnoid granulation from dural sinus thrombosis. If we suspect that giant arachnoid granulations are the cause of venous hypertension, interdural sinus pressure measurement can be used to exclude the lesion as the cause of the symptom.
Acknowledgement
There is no funding resources and interest in this manuscript and this has never been presented in neurosurgical society until now.
References
- 1.Arjona A, Delgado F, Fernandez-Remero E. Intracranial hypertension secondary to giant arachoind granulations. J Neurol Neurosurg Psychiatry. 2003;74:418. doi: 10.1136/jnnp.74.4.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brunori A, Vagnozzi R, Giuffre R. Antonio Pacchioni (1665-1726): early studies of the dura mater. J Neurosurg. 1993;78:515–518. doi: 10.3171/jns.1993.78.3.0515. [DOI] [PubMed] [Google Scholar]
- 3.Chin SC, Chen CY, Lee CC, Chen FH, Lee KW, Hsiao HS, et al. Giant arachnoid granulation mimicking dural sinus thrombosis in a boy with headache: MRI. Neuroradiology. 1998;40:181–183. doi: 10.1007/s002340050564. [DOI] [PubMed] [Google Scholar]
- 4.Dormont D, Sag K, Biondi A, Wechsler B, Marsault C. Gadolinium-enhanced MR of chronic dural sinus thrombosis. AJNR. 1995;16:1347–1352. [PMC free article] [PubMed] [Google Scholar]
- 5.Grossman CB, Potts DG. Arachnoid granulations: radiology and anatomy. Radiology. 1974;113:95–100. doi: 10.1148/113.1.95. [DOI] [PubMed] [Google Scholar]
- 6.Hsu FP, Nesbit GM, Barnwell SL. Youmans Neurosurgical Surgery. ed 5. Vol. 2. Philadelphia: Saunders; 2003. Cerebral venous and sinus thrombosis in Winn HR (ed) pp. 1723–1731. [Google Scholar]
- 7.Kan P, Stevens EA, Couldwell WT. Incidental giant arachnoid granulation. AJNR. 2006;27:1491–1492. [PMC free article] [PubMed] [Google Scholar]
- 8.Leach JL, Jones BV, Tomsick TA, Stewart CA, Balko MG. Normal appearance of arachnoid granulations on contrast-enhanced CT and MR of the brain: differentiation from dural sinus disease. AJNR. 1996;17:1523–1532. [PMC free article] [PubMed] [Google Scholar]
- 9.LeGros Clark WE. On the pacchionian bodies. J Anat. 1920;55:40–48. [PMC free article] [PubMed] [Google Scholar]
- 10.Mamourian AC, Towfighi J. MR of giant arachnoid granulation, a normal variant presenting as a mass within the dural venosus sinus. AJNR. 1995;16:901–904. [PMC free article] [PubMed] [Google Scholar]
- 11.Potts DG, Reilley KF, Deonarine V. Morphology of arachnoid villi and granulations. Radiology. 1972;105:333–341. doi: 10.1148/105.2.333. [DOI] [PubMed] [Google Scholar]
- 12.Tokiguchi S, Hayashi S, Takahashi H, Okamoto K, Ito J. CT of the pacchionian body. Neuroradiology. 1993;35:347–348. doi: 10.1007/BF00588366. [DOI] [PubMed] [Google Scholar]
- 13.Wolpow ER, Schaumburg HH. Structure of the human arachnoid granulation. J Neurosurg. 1972;37:724–727. doi: 10.3171/jns.1972.37.6.0724. [DOI] [PubMed] [Google Scholar]
- 14.Case records of the Massachusetts General Hospital Weekly clinicopathological exercises Case 42-1984 A 29-year-old woman with a lytic lesion of a parietal bone. N Engl J Med. 1984;311:1036–1043. doi: 10.1056/NEJM198410183111608. [DOI] [PubMed] [Google Scholar]