Abstract
Objective
Persistent trigeminal artery variant (PTAV) is an anastomosis between the internal carotid artery (ICA) and the cerebellar artery without any interposing basilar artery segment. We discuss its probable embryological origin and emphasize clinical implications.
Methods
Retrospectively 1250 conventional cerebral angiograms and 2947 cranial magnetic resonance angiographies (MRAs) were evaluated for the patients with PTAV.
Results
Five patients (four men and one woman, 23 to 76 years of age, median age 65 years) had a PTAV. Three patients who underwent MRA had a PTAV (3/2947=0.1%). Four of the patients who underwent cerebral angiography had a PTAV (4/1250=0.32%). Two of 143 patients who underwent both conventional angiography and cranial MRA showed PTAV. The PTAV was an incidental finding in all five patients. The PTAV originated from the cavernous segment of the left ICA in four patients and from the cavernous segment of the right ICA in one patient. The terminal branch of the PTAV was the anterior inferior cerebellar artery (AICA) and superior cerebellar artery (SCA) in two patients and the AICA only in the other three patients.
Conclusion
Neurosurgeons should be aware of possible presence of PTAV. Manipulation of this vessel during a surgical approach to the parasellar region and percutaneous gasserian ganglion procedure may result in hemorrhage or ischemia.
Keywords: Persistent trigeminal artery variant, Incidence, Clinical implication
INTRODUCTION
Persistent trigeminal artery is the most cephalic and the most frequent anomaly of the internal carotid-basilar artery anastomosis, with an angiographic incidence of approximately 0.2%10). The Persistent trigeminal artery variant (PTAV) is an anastomosis between the internal carotid artery (ICA) and cerebellar artery without an interposing segment of basilar artery15). Anatomically, this PTAV, which originate from the cavernous ICA, runs along the trigeminal nerve, enters the posterior fossa through Meckel's cave or the isolated dural foramen, and directly supplies the cerebellum. In this in vivo study, we used high resolution magnetic resonance imaging, magnetic resonance angiography (MRA), and conventional angiography, to demonstrate the incidence, origin, course and relationships of the PTAV. We discuss their probable embryological origin and emphasize clinical implications.
MATERIALS AND METHODS
We retrospectively reviewed the 1250 conventional cerebral angiograms and 2947 cranial MRAs for searching patients with PTAV. Conventional cerebral angiography (Philips V-5000, Philips Medical System, Eindhoven, Netherlands) was performed in 744 patients between July 1, 1997 and August 31, 2006, and cranial MRA (1.5T, Signa, General Electric, Milwaukee, WI, USA) was performed in 880 patients between May 1, 2001 and June 30, 2004 in one hospital. In addition, conventional cerebral angiography (Philips V-3000, Philips Medical System, Eindhoven, Netherlands) was performed in 506 patients between April 1, 2000 and September 30, 2006 and cranial MRA (1.5T, Intera Achieva, Philips Medical System, Eindhoven, Netherlands) was performed in 2067 patients between August 1, 2003 and May 5, 2007 in another hospital. Both cerebral angiography and MRA were performed in 143 of the patients. The initial angiographic studies were undertaken for a variety of clinical conditions including symptoms of cerebral ischemia, cerebral infarction, hemorrhagic contusion, intracerebral hemorrhage, headache and dizziness. The images were obtained either from a routine diagnostic study or from the initial diagnosis during an interventional procedure. We subsequently evaluated all of the angiograms for PTAV. In patients exhibiting PTAV, special attention was given to define the origin and cerebellar territory of this vessel. We recorded the presence of associated vascular lesions including cerebral aneurysms, vascular stenosis, or occlusions and other anomalies.
RESULTS
Five patients (four men and one woman, 23 to 76 years of age, median age 65 years) had a PTAV.
Three patients among the 2947 patients who underwent MRA had a PTAV (3/2947=0.1%) (Fig. 1). Four of the patients who underwent cerebral angiography had a PTAV (4/1250=0.32%) (Fig. 2). Two of 143 patients who underwent both conventional angiography and cranial MRA showed PTAV (Table 1). Five out of 4054 patients (2947+1250-143=4054) had PTAV (5/4054=0.12%). PTAV was an incidental finding in all five patients. The PTAV originated from the cavernous segment of the left ICA in four patients and from the cavernous segment of the right ICA in one. The terminal branch of the PTAV was both AICAs and SCA in two patients, and the AICA only in three patients (Table 1).
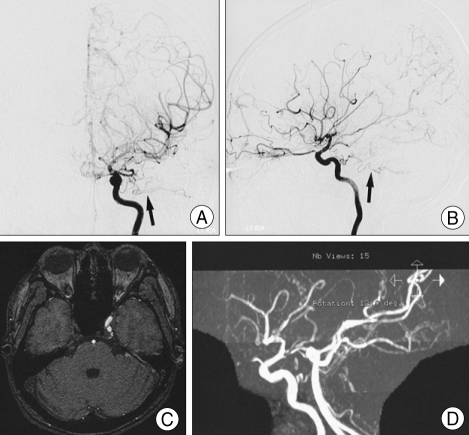
Fig. 1.
Patient 1. Left internal carotid angiograms, anteroposterior view (A) and lateral view (B), showing the persistent trigeminal artery variant (arrow) anastomosing the cavernous portion of the internal carotid artery to the anterior inferior cerebellar artery. Axial three-dimensional time-of-flight magnetic resonance source image (C) showing an abnormal vessel originating from the cavernous portion of the left internal carotid artery. Three-dimensional time-of-flight magnetic resonance angiography (D) showing a persistent trigeminal artery variant originating from the cavernous portion of the left internal carotid artery.
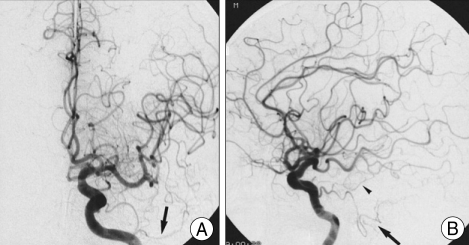
Fig. 2.
Patient 3. Left internal carotid angiograms, anteroposterior view (A) and lateral view (B), showing the persistent trigeminal artery variant (arrow) anastomosing the cavernous portion of the internal carotid artery to the superior cerebellar artery and anterior inferior cerebellar artery (arrow head).
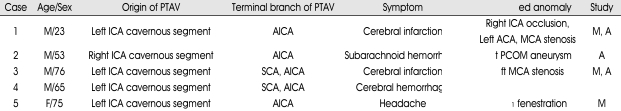
Table 1.
Summary of five patients with persistent trigeminal artery variant detected by transfemoral cerebral angiography and magnetic resonance angiography
PTAV : persistent trigeminal artery variant, SCA : superior cerebellar artery, AICA : anterior inferior cerebellar artery, ICA : internal carotid artery, ACA : anterior cerebral artery, MCA : middle cerebral artery, PCOM : posterior communicating artery, A1 : proximal anterior cerebral artery, M : magnetic resonance angiography, A : transfemoral cerebral angiography
Associated vascular abnormalities were middle cerebral artery stenosis, posterior communicating artery aneurysm, left proximal anterior cerebral artery fenestration, and ICA occlusion associated with stenosis of the anterior and the middle cerebral artery.
DISCUSSION
Incidence and pathogenesis
Neither the primitive trigeminal artery nor the paired longitudinal neural arteries normally persist in adults. Persistence of the primitive trigeminal artery with normal fusion of the longitudinal neural arteries into the basilar artery results in a carotid-basilar artery anastomosis. Persistence of the primitive trigeminal artery with incomplete fusion of the longitudinal neural arteries may result in either a superior or an inferior cerebellar vessel arising anomalously from the cavernous ICA. Cerebellar arteries originating from the ICA account for 0.18% of anomalous cerebellar arteries arising directly from the ICA on 5500 vertebral angiograms14). PTAVs may show distributions corresponding to the SCA, to the AICA, or to the posterior inferior cerebellar arterial territories. The corresponding artery of vertebrobasilar origin may be hypoplastic or absent, depending on the caliber of the PTAV14). Park et al.12) reported that five PTAVs were found, with an incidence of 0.14% (5/3552), on 3552 cerebral angiograms in Korea. In this study, four (0.32%) of 1250 patients who underwent cerebral angiography and three (0.1%) among the 2947 patients who underwent MRA had PTAVs. The origin of PTAV was cavernous portion of the ICA in all five patients. The terminal branch of the PTAV was AICA and SCA in two patients and AICA only in the other three patients (Table 1).
Because PTAVs are usually small vessels, MRI may fail to reveal them. In this study, three MRAs showed the PTAV. Although MRA images using a three-dimensional time-of-flight technique is limited, the PTAVs are usually located within the imaging slab. Despite the inferior anatomical resolution relative to conventional cerebral angiography, MRA facilitates a definite diagnosis and provides an excellent demonstration of anomalous vessels such as PTAVs16). However, other types of persistent carotid-basilar anastomosis such as the otic, hypoglossal, and proatlantal arteries, may be missed, because they are usually located caudal to the imaging slab.
Clinical implications
Persistent trigeminal arteries rarely cause trigeminal neuralgia as a result of their intracranial course. Because these vessels run medially and join the basilar artery after entering the posterior fossa, they are less likely to compress the root entry zone and therefore do not often cause trigeminal neuralgia. Those that do cause trigeminal neuralgia may be extremely long and tortuous one. PTAVs do not join the basilar artery as a persistent trigeminal artery does. After they enter the posterior fossa through the Meckel's cave or an isolated dural foramen, they course dorsally and run near the root entry zone of the trigeminal nerve11). Thus, PTAV should be considered as a possible cause of trigeminal neuralgia11). To the best of our knowledge, only four previous reports of trigeminal neuralgia caused by a PTA have been published8,9,11,13). During microvascular decompression, most PTA and PTAV loops are observed to compress the medial aspect of the root entry zone and branch into a few perforating arteries that proceed to the brainstem around the entire nerve root. Therefore, surgeons should take special care to prevent kinking and avulsion of the perforating arteries when these vessels are moved to different position with the use of a prosthesis.
The presence of an embryonic vessel persisting into adult life is indicative of disturbed cerebrovascular development. Therefore, a PTAV is frequently associated with other vascular abnormalities, particularly aneurysms3). PTAV may be associated with intracranial aneurysmwith an incidence of 26%17). The major sites of aneurysms associated with PTAV are the circle of Willis1,2,4-7,17). These anomalous vessels are congenital whereas the origin of aneurysm is unclean with acquired and congenital factors being implicated1). It is possible that maldevelopment causes structural insufficiency of the arterial wall, especially of the media, including massive arterial ectasias and subsequent saccular aneurysm1). Common congenital factors may be important in the development of arterial aneurysms.
Neurosurgeons should be aware of the presence of PTAVs in at least three situations. The first situation is related to the risk of hemorrhage or ischemia by manipulation of this vessel during a surgical approach to the parasellar region6). The second concern is a potential risk of cerebellar ischemia by therapeutic or spontaneous occlusion of the carotid artery. The third is related to the risk of hemorrhagic complications in the percutaneous gasserian ganglion procedure (gasserian ganglion alcohol block, radiofrequency gangliolysis, or retrogasserian glycerol injection) for the treatment of trigeminal neuralgia, because this vessel runs close to the Meckel's cave6,11).
CONCLUSION
We found that four (0.32%) of 1250 patients who underwent cerebral angiography and three (0.1%) of 2947 patients who underwent MRA showed PTAVs. Manipulation of this vessel during surgical approaches to the parasellar region and percutaneous gasserian ganglion procedure may carry the risks of hemorrhage or ischemia.
Acknowledgement
This work was supported by research grant from an Inje University Collage of Medicine.
References
- 1.Abe T, Matsumoto K, Aruga T. Primitive trigeminal artery variant associated with intracranial ruptured aneurysm and cerebral arteriovenous malformation -case report- Neurol Med Chir (Tokyo) 1994;34:104–107. doi: 10.2176/nmc.34.104. [DOI] [PubMed] [Google Scholar]
- 2.Chambers AA, Lukin R. Trigeminal artery connection to the posterior inferior cerebellar arteries. Neuroradiology. 1975;9:121–123. doi: 10.1007/BF00332958. [DOI] [PubMed] [Google Scholar]
- 3.Hanabusa K, Murao K, Morikawa A, Taki W, Waga S. Endovascular treatment for a ruptured persistent trigeminal artery variant aneurysm on the distal portion -case report- Neurol Med Chir (Tokyo) 2000;40:637–640. doi: 10.2176/nmc.40.637. [DOI] [PubMed] [Google Scholar]
- 4.Haughton VM, Rosenbaum AE, Pearce J. Internal carotid origins of the inferior cerebellar arteries. Am J Roentgenol. 1978;130:1191–1192. doi: 10.2214/ajr.130.6.1191. [DOI] [PubMed] [Google Scholar]
- 5.Hayashi M, Taira T, Terasaka N, Tanikawa T, Takakura K. Intracavernous internal carotid artery aneurysm associated with persistent trigeminal artery variant -case report- No Shinkei Geka. 1994;22:67–70. [PubMed] [Google Scholar]
- 6.Hirai T, Korogi Y, Sakamoto Y, Hamatake S, Murakami R, Ikushima I, et al. MR angiography of the persistent trigeminal artery variant. J Comput Assist Tomogr. 1995;19:495–497. doi: 10.1097/00004728-199505000-00027. [DOI] [PubMed] [Google Scholar]
- 7.Ito J, Takeda N, Suzuki Y, Takeuchi S, Osugi S, Yoshida Y. Anomalous origin of the anterior inferior cerebellar arteries from the internal carotid artery. Neuroradiology. 1980;19:105–109. doi: 10.1007/BF00342605. [DOI] [PubMed] [Google Scholar]
- 8.Jackson IJ, Garza-Mercado R. Persistent carotid-basilar anastomosis : occasionally a posible cause of tic douloureux. Angiology. 1960;11:103–107. doi: 10.1177/000331976001100203. [DOI] [PubMed] [Google Scholar]
- 9.Kempe LG, Smith DR. Trigeminal neuralgia, facial spasm, intermedius and glossopharyngeal neuralgia with persistent carotid basilar anastomosis. J Neurosurg. 1969;31:445–451. doi: 10.3171/jns.1969.31.4.0445. [DOI] [PubMed] [Google Scholar]
- 10.Lie TA. Congenital malformations of the carotid and vertebral arterial systems, including the persistent anastomoses. In: Vinken PJ, Bruyn GW, editors. Handbook of Clinical Neurology 12. Vol. 12. Amsterdam: Elsevier; 1972. pp. 289–339. [Google Scholar]
- 11.Morita A, Fukushima T, Miyazaki S, Shimizu T, Atsuchi M. Tic douloureux caused by primitive trigeminal artery or its variant. J Neurosurg. 1989;70:415–419. doi: 10.3171/jns.1989.70.3.0415. [DOI] [PubMed] [Google Scholar]
- 12.Park SI, Kim DI, Jun P, Yoon PH, Hwang GJ, Cheon YJ, et al. Persistent carotid-vertebrobasilar anastomosis : Radiologic findings. J Korean Radiol Soc. 1998;39:863–867. [Google Scholar]
- 13.Piatt JH, Wilkins RH. Treatment of tic douloureux and hemifacial spasm by posterior fossa exploration : therapeutic implications of various neurovascular relationships. Neurosurgery. 1984;14:462–471. doi: 10.1227/00006123-198404000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Siqueira M, Piske R, Ono M, Marino R., Jr Cerebellar arteries originating from the internal carotid artery. Am J Neuroradiol. 1993;14:1229–1235. [PMC free article] [PubMed] [Google Scholar]
- 15.Teal JS, Rumbaugh CL, Bergeron RT, Scanlan RL, Segall HD. Persistent carotid-superior cerebellar artery anastomosis : A variant of persistent trigeminal artery. Radiology. 1972;103:335–341. doi: 10.1148/103.2.335. [DOI] [PubMed] [Google Scholar]
- 16.Uchino A, Mizushima A, Aibe H, Tanaka M. MR imaging and MR angiography of persistent trigeminal artery and its variant. Clin Imaging. 1996;20:247–252. doi: 10.1016/0899-7071(95)00047-x. [DOI] [PubMed] [Google Scholar]
- 17.Watanabe T, Aoki A, Chan SC. Two cases of persistent trigeminal artery variant. No Shinkei Geka. 1988;16:95–100. [PubMed] [Google Scholar]