Abstract
Hematomas caused by ruptured traumatic pseudoaneurysms of the middle meningeal artery (MMA) usually present with extradural hematomas, whereas intradural intraparenchymal hematomas are extremely rare. We report a case of traumatic pseudoaneurysm of the MMA giving rise to an intracerebral hematoma after head trauma. A 70-year-old man suffered a massive intracerebral temporoparietal hemorrhage after a head injury. CT angiogram of the brain revealed a large hematoma in the right middle cranial fossa extending to the right sylvian fissure. Cerebral angiogram also revealed a pseudoaneurysm of the MMA, which was successfully treated surgically. Although traumatic MMA pseudoaneurysm producing intracerebral hematoma (ICH) is rare, it should be considered as a possible cause of intracerebral hematoma.
Keywords: Traumatic pseudoaneurysm, Middle meningeal artery (MMA), Intracerebral hematoma
INTRODUCTION
Traumatic aneurysms comprise less than 1% of all intracranial aneurysms1,11). Most of these aneurysms are actually false aneurysms, or pseudoaneurysms, which are caused by the rupture of entire vessel wall layers, with the wall of the aneurysm being formed by the surrounding cerebral structures9). Traumatic pseudoaneurysms of the middle meningeal artery (MMA) are also rare. Acute or delayed epidural hematoma is the most frequent presentation of traumatic pseudoaneurysms9,11), but they can sometimes be associated with a subdural hematoma or subarachnoid hemorrhage. Intracerebral hematoma due to ruptured traumatic pseudoaneurysm of the MMA is extremely rare.
We report a case of patient with a ruptured traumatic pseudoaneurysm of the MMA who presented with a fatal intracerebral hematoma (ICH) in the right temporo-parietal region immediately after trauma.
CASE REPORT
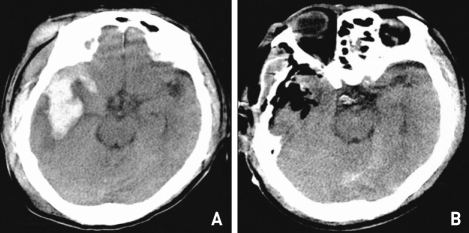
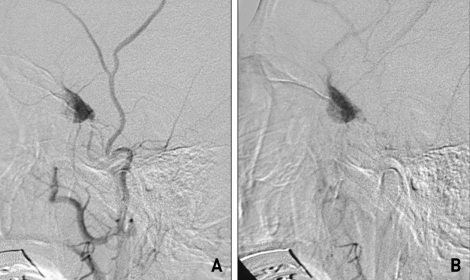
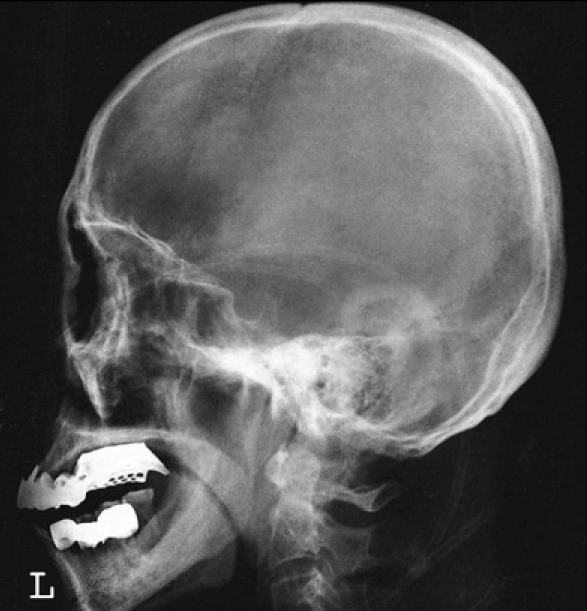
A 70-year-old man with a history of head trauma following a road traffic accident was admitted to our hospital on August 4, 2006. On admission, the patient was drowsy and his Glasgow Coma Scale (GCS) score was 13/15. He presented with left hemiparesis (grade IV). Skull x-ray showed no abnormalities (Fig. 1). Brain CT revealed a large hematoma in the right middle cranial fossa extending to the right sylvian fissure and in the right frontotemporal region of the scalp (Fig. 2A). Because the ICH was in contact with the sylvian fissure, a cerebral angiogram was performed to identify the cause of the bleed, such as an aneurysmal rupture. Cerebral angiogram revealed active bleeding from the right MMA and an active extravasation of contrast media. It also showed delayed filling and emptying of the contrast media, suggesting a ruptured pseudoaneurysm of the MMA (Fig. 3A, B). On admission, patient and his family refused the surgery. Two days later, when his level of consciousness began to deteriorate and develop hemiparesis on the left side, his family finally decided to allow him to undergo surgery, with a more deepened mental state and deteriorating neurologic findings suggesting a secondary rupture of the traumatic pseudoaneurysm. Follow-up brain CT scan showed no significant interval change to suggest a large hematoma, but he was in a state of stupor and had a GCS score of 10/15. An emergency right frontotemporal craniotomy was performed. There was an extensive hematoma of the scalp along the right frontotemporal area, but his skull appeared to be normal. On the inner surface of the intact dura, there was an irregular-shaped aneurysm arising from the MMA and active bleeding from the injured right MMA. There was an intracerebral hematoma caused by a ruptured traumatic pseudoaneurysm of the MMA. The parent vessel along the aneurysm was coagulated. The temporoparietal hematoma was evacuated successfully (Fig. 2B). His postoperative recovery was good. On discharge, on September 26, 2006, he was in a mild state of confusion, and his GCS score was 14/15. His hemiparesis on the left side was grade III.
Fig. 1.
Skull x-ray shows no skull fracture.
Fig. 2.
A : Preoperative brain computed tomography (CT) scan showing a large scalp hematoma and fatal intracerebral hematoma in the right temporoparietal region, centered on the sylvian fissure, contacting the dura mater and extending to the ventricles. B : Postoperative CT scan showing evidence of right frontotemporal cranioplasty and hematoma removal.
Fig. 3.
Right external carotid angiogram, lateral view, A : Early phase, B : Late phase. There is delayed filling of the pseudoaneurysm during the arterial phase and a very slow emptying during the venous phase. The distal segment of the artery is not visible.
DISCUSSION
Hematomas by ruptured traumatic pseudoaneurysms of MMA usually present with extradural hematomas3,6). However, traumatic pseudoaneurysms of the MMA, although rare, have been considered as a possible etiology of acute intracerebral hematoma. Two cases of ICHs caused by the rupture of traumatic MMA pseudoaneurysms have been reported in the English literature. Bruneau et al.2) reported a 64-year-old woman who suffered a massive spontaneous intracerebral frontotemporal hemorrhage with ventricular spread caused by a traumatic pseudoaneurysm of the MMA. Rambaugh et al.12) reported a 63-year-old woman who presented with a right temporal hematoma and in whom angiography revealed a false aneurysm of the MMA at the level of the sphenoid ridge.
About 70-90% of cases of traumatic MMA pseudoaneurysm are associated with a fracture crossing the MMA in the temporal region13). The MMA is injured at this site and covered by hematoma or secondary connective tissues, thus forming a pseudoaneurysm. In our patient, there was no skull fracture, but an extensive soft tissue hematoma along the right frontotemporal area was noted. Therefore, we assumed that the pseudoaneurysm might have arisen from a closed head injury that involved a traction injury to the vessel wall.
In the present case, the pattern of combined ICH and SAH on brain CTA was similar to that seen with ruptured MCA or ICA aneurysm. Thus, we performed a cerebral angiogram on admission to rule out the possibility of a non-traumatic ruptured MCA or ICA aneurysm as a cause of the hematoma. Fortunately, the MMA pseudoaneurysm was visualized on the angiography.
Traumatic pseudoaneurysms show specific characteristics on angiography4,5,7) : they are peripherally located, at a distance from a branching point, and they do not show evidence of a neck. The aneurysmal sac is sometimes irregular. Its filling and emptying are delayed and very slow, which means that the contrast medium has time to settle at the bottom of the aneurysm and the pre- and post-aneurysmal segments of the meningeal artery are not opacified at the same time. These features explain why traumatic meningeal pseudoaneurysms are usually visible only in the late injection stages of selective external carotid angiography. In our case, there was active bleeding, extravasation of the contrast media, delayed filling, and slow empting, which were not surprising considering the ruptured traumatic pseudoaneurysm of the MMA shown on cerebral angiography and the fact that the operation field revealed a traumatic pseudoaneurysm arising from the right MMA.
The natural history of traumatic aneurysms is not well known, but progressive growth of traumatic aneurysms has been demonstrated on repeated angiograms8,10). It is thought that they develop after a small tear in the meningeal artery, which is sealed off by a clot, then recanalize and form a false lumen. These pseudoaneurysms gradually enlarge and can rupture at any time2,5). Therefore, considering the risk of a secondary rupture, we suggest that the treatment of traumatic pseudoaneurysms must always be carried out without delay, especially the surgical management of these aneurysms is technically quite simple.
CONCLUSION
Although traumatic MMA pseudoaneurysm producing intracerebral hematoma (ICH) is rare, it should be considered as a possible cause of intracerebral hematoma. We suggest that such patients should be treated surgically as soon as possible in other to prevent a secondary bleeding from the traumatic pseudoaneurysm.
References
- 1.Benoit BG, Wortzman G. Traumatic cerebral aneurysms : clinical features and natural history. J Neurol Neurosurg Psychiatry. 1973;36:127–138. doi: 10.1136/jnnp.36.1.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bruneau M, Gustin T, Zekhnini K, Gilliard C. Traumatic false aneurysm of the middle meningeal artery causing an intracerebral hemorrhage : case report and literature review. Surg Neurol. 2002;57:174–178. doi: 10.1016/s0090-3019(01)00668-1. [DOI] [PubMed] [Google Scholar]
- 3.Garza-Mercado R, Rangel RA. Extradural hematoma associated with traumatic middle meningeal artery pseudoaneurysm. Report of two cases. Neurosurgery. 1979;5:500–503. doi: 10.1227/00006123-197910000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Higazi I, El-Banhawy A, El-Nady F. Importance of angiography in identifying false aneurysm of the middle meningeal artery as a cause of extradural hematoma. Case report. J Neurosurg. 1969;30:172–176. doi: 10.3171/jns.1969.30.2.0172. [DOI] [PubMed] [Google Scholar]
- 5.Kim JH, Yim MB, Lee CY, Kim IM. Surgical management of pseudoaneurysm. J Korean Neurosurg Soc. 2001;30:307–318. [Google Scholar]
- 6.Kimora T, Sako K, Satoh M, Nakai H, Yonemasu Y, Takeuchi E, et al. Post-traumatic pseudoaneurysm of the middle meningeal artery. A case report. No Shinkei Geka. 1995;23:1021–1025. [PubMed] [Google Scholar]
- 7.Kuhn RA, Kugler H. False aneurysms of the middle meningeal artery. J Neurosurg. 1964;21:92–96. doi: 10.3171/jns.1964.21.2.0092. [DOI] [PubMed] [Google Scholar]
- 8.Meder JF, Gaston A, Merienne L, Godon-Hardy S, Fredy D. Traumatic aneurysms of the internal and external carotid arteries. One case and review of the literature. J Neuroradiol. 1992;19:248–255. [PubMed] [Google Scholar]
- 9.Morard M, de Tribolet N. Traumatic aneurysm of the posterior inferior cerebellar artery : case report. Neurosurgery. 1991;29:438–441. doi: 10.1097/00006123-199109000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Okumura H, Tenjin H, Ueda S. A case of traumatic pseudoaneurysm of the middle meningeal artery treated with endovascular surgery. No Shinkei Geka. 1998;26:929–933. [PubMed] [Google Scholar]
- 11.Parkinson D, West M. Traumatic intracranial aneurysms. J Neurosurg. 1980;52:11–20. doi: 10.3171/jns.1980.52.1.0011. [DOI] [PubMed] [Google Scholar]
- 12.Rambaugh CL, Bergeron T, Kurze T. Intracranial vascular damage associated with skull fracture : radiological aspects. Radiology. 1972;104:81–87. doi: 10.1148/104.1.81. [DOI] [PubMed] [Google Scholar]
- 13.Tsutomu K, Teruaki K, Yoshirou K, Takao O, Hidesato O, Sadanobu O. Traumatic lesion of the bilateral middle meningeal arteries : case report. Neurol Med Chir (Tokyo) 2002;42:221–223. doi: 10.2176/nmc.42.221. [DOI] [PubMed] [Google Scholar]