Abstract
Objective
There are numerous reports on the primary stabilizing effects of the different cervical cages for cervical radiculopathy. But, little is known about the subsidence which may be clinical problem postoperatively. The goal of this study is to evaluate subsidence of cage and investigate the correlation between radiologic subsidence and clinical outcome.
Methods
To assess possible subsidence, the authors investigated clinical and radiological results of the one-hundred patients who underwent anterior cervical fusion by using AMSLU™ cage during the period between January 2003 and June 2005. Preoperative and postoperative lateral radiographs were measured for height of intervertebral disc space where cages were placed. Intervertebral disc space was measured by dividing the sum of anterior, posterior, and midpoint interbody distance by 3. Follow-up time was 6 to 12 months. Subsidence was defined as any change in at least one of our parameters of at least 3 mm.
Results
Subsidence was found in 22 patients (22%). The mean value of subsidence was 2.21 mm, and mean subsidence rate was 22%. There were no cases of the clinical status deterioration during the follow-up period. No posterior or anterior migration was observed.
Conclusion
The phenomenon of subsidence is seen in substantial number of patients. Nevertheless, clinical and radiological results of the surgery were favorable. An excessive subsidence may result in hardware failure. Endplate preservation may enables us to control subsidence and reduce the number of complications.
Keywords: Subsidence, AMSLU™ cage, Anterior cervical fusion
INTRODUCTION
The optimum treatment for degenerative cervical disc disease is not fully established yet, and controversy still exists16). When a surgical intervention is planned, anterior interbody fusion is usually indicated to restore physiologic disc height and to achieve solid fusion. For this purpose, a central discectomy is performed and then, the intervertebral disc space is filled with interbody fusion cages in most instances1,3,11,15,20).
Cho, et al.2) previously reported feasibility of cervical fusion in short-term period by using the AMSLU™ cage (Eurosurgical, Amsterdam, Netherlands). Anterior interbody fusion using cylindrical cage has many benefits including short incision, short operating time, low complication rate associated with bone graft, easy maneuverability of instrument and high rate of bone fusion. We found, however, the cages have been settled down and encroached toward the endplates as time passed. Thus, we evaluated subsidence of such cylindrical cage and investigated the correlation between radiographic subsidence and clinical outcome.
MATERIALS AND METHODS
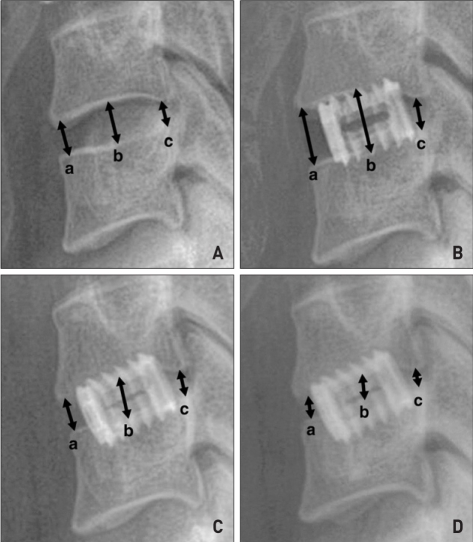
This retrospective study was based on a through review of the medical charts, operative notes, out-patient clinical charts and radiographic follow-up images. We identified 100 patients who underwent anterior cervical fusion by using AMSLU™ cage from January 2003 to June 2005. All patients were undertaken bone mineral density and their T score was less than -1.0 point. All patients were placed on the neck brace to prevent excessive neck movement during at least 1 month after surgery. For the purpose of this study, we defined the subsidence as any settlement in disc height of at least 3 mm on radiographic images. Intervertebral disc height was measured by dividing the sum of anterior, posterior, and midpoint interbody distance by 3 (Fig. 1).
Fig. 1.
Measurement of the anterior, middle and posterior disc space height. Disc height (DH) is defined as a+b+c/3(mm). The subsidence is defined as any change in at least one of our follow up DH of at least 3 mm. A and B, C, D shows pre and postoperative 3 months, 6 months, 12 months plain lateral views respectively.
Surgical technique
All patients underwent surgical procedures by the same standardized technique. Under a microscope, cervical discectomy was performed according to the traditional Smith-Robinson approach. The tube was positioned on the median part of the intervertebral space, distractor was then inserted through the tube. The distractor was rotated a quarter turn to realize the distraction. The impaction cap was placed in order to introduce the blades into the interbody space. And then, the distractor was removed with another quarter turn movement. The disc space was reamed off. The cage was positioned on the implant inserter by 3 pins secured by the threaded shaft. The cage is filled with the bone fragments collected during the approach and the drilling. Finally, the cylindrical cage (AMSLU™) was inserted by turning clockwise the implant inserter and applying a light pressure.
Radiological evaluation
Plain radiographs in anterior-posterior and lateral views were obtained postoperatively prior to hospital discharge and at 3, 6, 12 months after operation respectively. In order to assess subsidence, three different measurements on the lateral radiographs were taken for each case postoperatively and at the last follow-up. We defined the subsidence as any change in at least one of our follow-up disc height of at least 3 mm.
RESULTS
Patients'age ranged from 29 to 71 years (mean : 47.7 year). There were 78 cases of single-level fusion. The decrease of disc height was measured by a mean of 1.9 mm in single level fusion and, 2.7 mm in two-level, 3.2 mm in three-level fusion at postoperative 12 months compared to immediate postoperation. The most common level involved was C5-C6 (52.3%) and, C6-C7 (20.5%) and C4-C5 (19.3%) comprised the remote next level.
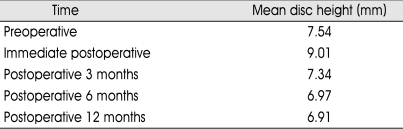
The mean disc height was 7.54 mm in the preoperative state, 9.01 mm in the immediate postoperative state, 7.34 mm in 3 months, 6.97 mm in 6 months and 6.91 mm in 12 months (Table 1).
Table 1.
Mean disc height (mm)
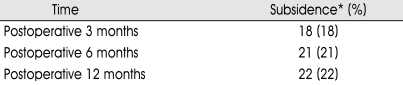
Patients who exhibited more than 3 mm of the disc height reduction in 3 months later were 18 (18%), in 6 months later 21 (21%) and in 12 months later 22 (22%) (Table 2). No posterior or anterior migration of device was observed in any of patients.
Table 2.
Subsidence rate (%)
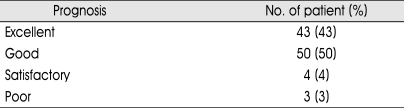
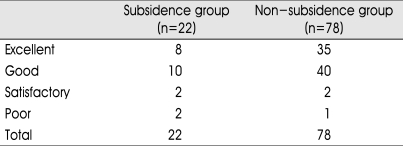
According to Odom's classification13), the excellent outcome was seen in 43 (43%) patient, good in 50 (50%), satisfactory in 4 (4%) and poor in 3 (3%) (Table 3). Comparison of outcome between subsidence group and non-subsidence group in postoperative 12 months was conducted. In subsidence group, 8 patients showed excellent, 10 patients good, 2 patients satisfactory and 2 patients poor outcome. This result was not statistically significant (p value>0.05) (Table 4).
Table 3.
Overall outcome (n=100) (Odom, et al13))
Table 4.
Comparison of clinical outcome between subsidence group and non-subsidence group according to Odom's classification (p value > 0.05)
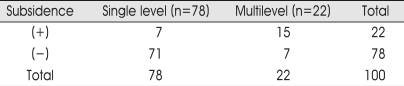
Subsidence rate was compared between multilevel patients and single level patients. Fifteen patients showed subsidence among 22 multilevel patients and only 7 patients displayed subsidence among 78 single level patients (Table 5). This result was statistically significant (p value<0.05).
Table 5.
Comparison of subsidence rate between in single-level group and in multilevel group (p value < 0.05)
DISCUSSION
Subsidence is the term given to the postoperative process of decreasing construct length due to the effects of load bearing. It is relevant to surgeons performing anterior cervical interbody fusion because the grafts act to distract the neural foramina. And, this distraction can be lost as a result of subsidence, potentially resulting in the recurrence of radiculopathy.
The causes of subsidence may result from the instability created by discectomy, postoperative cervical motion, cage design, end plate preparation, or bone mineral density itself4,8,9,14,19). Because excessive postoperative cervical movement caused subsidence in various cervical interbody implant types19), all of our patients received anterior cervical interbody fusion put on neck brace by the end of 1 month after surgery.
In the study by Vavruch, et al.17), the carbon-fiber cage group did as well as the group with the classic Cloward procedure and the pseudoarthrosis rate of their cage group is 38%, but their exact rates and degrees of subsidence remain unknown. Gercek, et al.6) reported subsidence in five out of nine cages which was measured by a decrease in the disc space narrowing of at least 3 mm.
Gary W, et al.5) reported that in 67 of the 70 patients, subsidence could be measured. But, they didn't define subsidence as decrease in the disc space narrowing of at least 3 mm. In this study, subsidence was greater in multilevel fusions than in single-level fusions. Our study also showed the similar esults.
Recently, Van Limbeek, et al.16), in a systematic literature review, failed to identify the best method for a single-level anterior cervical interbody fusion. With the introduction of different interbody fusion devices, such as cages, surgical strategies have been evolved to achieve anterior cervical fusion. The studies on such promising techniques have been published thereafter7,12,15,17). However, Wigfield18), in a thorough literature review, concluded that there was limited evidence supporting the use of a cervical interbody fusion device in place of autologous bone.
In this study, there was no statistically significant difference in subsidence and clinical outcome. But, graft subsidence may have contributed to the formation of postoperative kyphosis. Graft subsidence in patients in whom anterior cervical instrumentation concomitantly is being placed is also likely to result in increased load bearing by the metal construct, with potential subsequent migration or failure. Therefore, surgeon must bear these points and try every effort to minimize subsidence.
The anterior cervical fusion using AMSLU™ cage in the cervical radiculopathy is a useful method2,10). If keeping in mind the possibility of hardware related complication such as subsidence, cylindrical cage will be more broadly used.
CONCLUSION
There was no statistically significant difference between subsidence and clinical outcome. But, subsidence was greater in multilevel fusions than in single-level fusions. Nevertheless, excessive subsidence may result in hardware related complications such as migration of instrument, surgeon must bear in mind preservating endplate and gentle handling to avoid subsidence, particularly in multilevel patient.
References
- 1.Brooke NS, Rorke AW, King AT. Preliminary experience of carbon fiber cage prostheses for treatment of cervical spine disorders. Br J Neurosurg. 1997;11:221–227. doi: 10.1080/02688699746285. [DOI] [PubMed] [Google Scholar]
- 2.Cho DC, Oh SH, Lee KS, Hong HJ, Yi HJ. Short-term results of anterior cervical fusion with cylindrical cage(AMSLU™) J Korean Neurosurg Soc. 2004;35:569–573. [Google Scholar]
- 3.Cunningham BW, Kanayama M, Parker LM. Osteogenic protein versus autologous interbody arthrodesis in the sheep thoracic spine : A comparative endoscopic study using the Bagby and Kuslich interbody fusion device [in process citation] Spine. 1999;24:509–518. doi: 10.1097/00007632-199903150-00002. [DOI] [PubMed] [Google Scholar]
- 4.Curylo LJ, Lindsey RW, Doherty BJ, LeBlanc A. Segmental variations of bone mineral density in the cervical spine. Spine. 1996;21:319–322. doi: 10.1097/00007632-199602010-00013. [DOI] [PubMed] [Google Scholar]
- 5.Gary W, R Scott Graham, William C. Graft subsidence after instrument-assisted anterior cervical fusion. J Neurosurg. 2002;97(Spine 2):186–192. doi: 10.3171/spi.2002.97.2.0186. [DOI] [PubMed] [Google Scholar]
- 6.Gercek E, Arlet V, Deliscle J, Marchesi D. Subsidence of stand-alone cervical cages in anterior interbody fusion : warning. Eur Spine J. 2003;12:513–516. doi: 10.1007/s00586-003-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hacker RJ. A randomized prospective study of an anterior cervical interbody fusion device with a minimum of 2 years of follow-up results. J Neurosurg. 200;93(Suppl 2):222–226. doi: 10.3171/spi.2000.93.2.0222. [DOI] [PubMed] [Google Scholar]
- 8.Hollowell JP, Vollmer DG, Wilson CR, Pintar FA, Yoganandan N. Biomechanical analysis of thoracolumbar interbody constructs : how important is the endplate. Spine. 1996;21:1032–1036. doi: 10.1097/00007632-199605010-00007. [DOI] [PubMed] [Google Scholar]
- 9.Kettler A, Wilke HJ, Claes L. Effects of neck movements on stability and subsidence in cervical interbody fusion : an in vitro study. J Neurosurg. 2001;94(Suppl 1):97–107. doi: 10.3171/spi.2001.94.1.0097. [DOI] [PubMed] [Google Scholar]
- 10.Luitjes WF. The AMSLU™ cage : a minimally invasive procedure for anterior cervical interbody fusion. KAECH. 2002;21:235–247. [Google Scholar]
- 11.Matge G. Anterior interbody fusion with the BAK-cage in cervical spondylosis. Acta Neurochir (Wien) 1998;140:1–8. doi: 10.1007/s007010050049. [DOI] [PubMed] [Google Scholar]
- 12.Matge G, Leclercq TA. Rationale for interbody fusion with threaded titanium cages at cervical and lumbar levels. Results on 357 cases. Acta Neurochir(Wien) 2000;142:425–433. doi: 10.1007/s007010050453. [DOI] [PubMed] [Google Scholar]
- 13.Odom GL, Finney W, Woodhall B. Cervical disc lesions. JAMA. 1958;166:23–28. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 14.Panjabi MM, White AA, Johnson RM. Cervical spine mechanics as a function of transection of components. J Biomech. 1975;8:327–336. doi: 10.1016/0021-9290(75)90085-8. [DOI] [PubMed] [Google Scholar]
- 15.Shono Y, McAfee PC, Cunningham BW. A biomechanical analysis of decompression and reconstruction methods in the cervical spine : Emphasis on a carbon-fiber-composite cage. J Bone Joint Surg Am. 1993;75:1674–1684. doi: 10.2106/00004623-199311000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Van Limbeek J, Jacobs WC, Anderson PG, Pavlov PW. A systematic literature review to identify the best method for a single level anterior cervical interbody fusion. Eur Spine J. 2000;9:129–136. doi: 10.1007/s005860050223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vavruch L, Hedlung R, Javid D, Leszniewski W, Shalabi A. A prospective randomized comparison between the Cloward procedure and a carbon fiber cage in the cervical spine : a clinical and radiologic study. Spine. 2002;27:1694–1701. doi: 10.1097/00007632-200208150-00003. [DOI] [PubMed] [Google Scholar]
- 18.Wigfield CC, Nelson RJ. Non autologous interbody fusion materials in cervical spine surgery: how strong is the evidence to justify their use. Spine. 2001;26:687–694. doi: 10.1097/00007632-200103150-00027. [DOI] [PubMed] [Google Scholar]
- 19.Wilke HJ, Kettler A, Goetz C, Claes L. Subsidence resulting from simulated postoperative neck movements : an in vitro investigation with a new cervical fusion cage. Spine. 2000;25:2762–2770. doi: 10.1097/00007632-200011010-00008. [DOI] [PubMed] [Google Scholar]
- 20.Zdeblick TA, Ghanayem AJ, Rapoff AJ. Cervical interbody fusion cages : An animal model with and without bone morphogenetic protein. Spine. 1998;23:758–765. doi: 10.1097/00007632-199804010-00002. discussion 766. [DOI] [PubMed] [Google Scholar]