Abstract
Objective
Thoracoscopic spinal surgery provides minimally invasive approaches for effective vertebral decompression and reconstruction of the thoracic and thoracolumbar spine, while surgery related morbidity can be significantly lowered. This study analyzes clinical results of thoracoscopic spinal surgery performed at our institute.
Methods
Twenty consecutive patients underwent video-assisted thoracosopic surgery (VATS) to treat various thoracic and thoracolumbar pathologies from April 2000 to July 2006. The lesions consisted of spinal trauma (13 cases), thoracic disc herniation (4 cases), tuberculous spondylitis (1 case), post-operative thoracolumbar kyphosis (1 case) and thoracic tumor (1 case). The level of operation included upper thoracic lesions (3 cases), midthoracic lesions (6 cases) and thoracolumbar lesions (11 cases). We classified the procedure into three groups: stand-alone thoracoscopic discectomy (3 cases), thoracoscopic fusion (11 cases) and video assisted mini-thoracotomy (6 cases).
Results
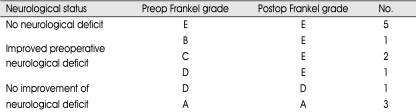
Analysis on the Frankel performance scale in spinal trauma patients (13 cases), showed a total of 7 patients who had neurological impairment preoperatively : Grade D (2 cases), Grade C (2 cases), Grade B (1 case), and Grade A (2 cases). Four patients were neurologically improved postoperatively, two patients were improved from C to E, one improved from grade D to E and one improved from grade B to grade D. The preoperative Cobb's and kyphotic angle were measured in spinal trauma patients and were 18.9±4.4° and 18.8±4.6°, respectively. Postoperatively, the angles showed statistically significant improvement, 15.1±3.7° and 11.3±2.4°, respectively (P<0.001).
Conclusion
Although VATS requires a steep learning curve, it is an effective and minimally invasive procedure which provides biomechanical stability in terms of anterior column decompression and reconstruction for anterior load bearing, and preservation of intercostal muscles and diaphragm.
Keywords: Video-assisted thoracoscopic surgery, Minimally invasive surgical procedure, Spinal fractures, Spinal fusion
INTRODUCTION
Video-assisted thoracoscopic spinal surgery (VATS) is an important minimally invasive approach to access for anterior pathologies of the thoracic and thoracolumbar spine. Since it was first reported in 1993 by Macks and associates, thoracoscopic spinal surgery has gradually become more popular in the treatment of various thoracic spinal pathologies. The use of VATS has several advantages including reduced postoperative pain and complication rates and faster recovery times. It is not yet familiar to most spinal surgeons because of its technically demanding performance and steep learning curve, and the need for special endoscopic instruments with related expenses. Therefore, the posterior approach is still a more universal procedure to treat thoracic lesions7).
Traumatic spinal injuries frequently involve the thoracolumbar junction, and cause significant injury to the anterior column of the spine, which absorbs the compression load of the spine. Thoracolumbar junction injuries presenting with neurological deficits have significant anterior compression of neural tissue. The anterior thoracic approach offers many biomechanical benefits, such as effective direct decompression of anterior pathologies, immediate restoration of anterior load-bearing, and short segment stabilization8). Given these biomechanically sound advantages, thoracoscopic spinal surgery is a useful minimally invasive procedure for the anterior approach.
This study analyzes our clinical experiences of thoracoscopic spinal surgery to treat various pathologies, such as thoracic disc herniation, tumors, and spinal trauma.
MATERIALS AND METHODS
Demographic features
Between April 2000 and July 2006, a total of twenty consecutive patients underwent video-assisted thoracoscopic surgery. They presented with thoracic spinal trauma (13 cases), thoracic disc herniations (4 cases), and one case of spinal tumor, tuberculous spondylitis, and postoperative kyphosis respectively. The mean age was 41 years (range, from 19 to 77 years) and the male to female ratio was three to one. Mean follow up period was 15 months. The characteristics of the patients are summarized in (Table 1).
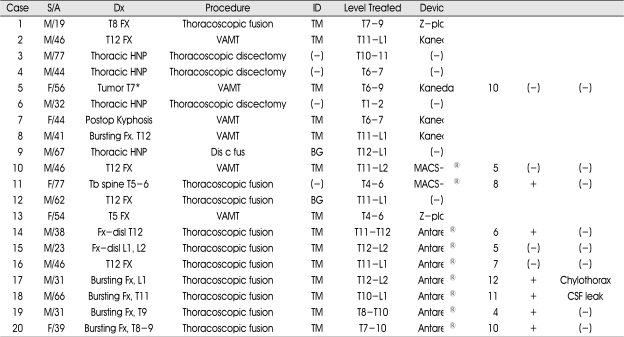
Table 1.
The characteristics of patients
S/A : Sex/Age, Dx : diagnosis, ID : interbody device, My : myelopathy, Cx : complication, FX : compression fracture with injury of ligament, VAMT : Video assisted mini-thoracotomy, dis & fus : video assisted thoracoscopic discectomy and fusion, Fx-disl : Fracture dislocation, TM : titanium mesh, BG : Autologus bone graft apply, *multiple myeloma
We classified the VATS procedures into three groups : standalone thoracoscopic discectomy (3 cases), thoracoscopic fusion (10 cases), and video assisted mini-thoracotomy (VAMT) (7 cases). The most frequent vertebral level of the bursting fracture and dislocation was T12 (6 cases), followed by midthoracic region (5 cases), T11 (1 case), L1 (2 cases) and L2 (1 case). Additional posterior instrumentation was performed for three patients who sustained three column injuries. The instruments used were Z-plate (Sofamor Danek, Memphis, TN) in 2 cases, Kaneda systems (DePuy AcroMed, Raynhem, MA) in 3 cases, MACS-TL® (Aesculap, Tuttlingen, Germany) in 2 cases, and Antares® (Medtronic SNT, Louisville, CO) in 6 cases.
Clinical and Radiographic Evaluation
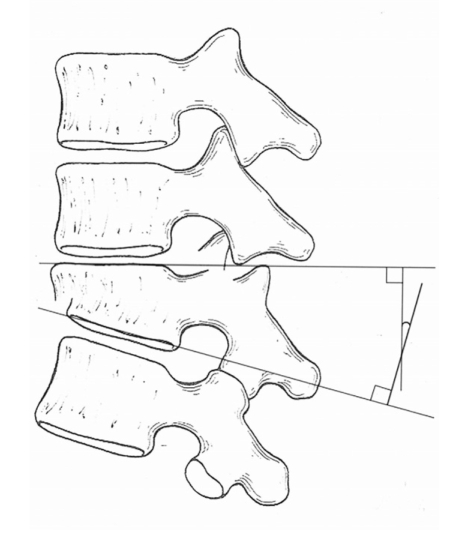
The comparison between preoperative and postoperative pain score was measured using the VAS score. We measured kyphotic angle and Cobb's angle in lateral radiographs of thoracic and thoracolumbar fractures due to trauma preoperatively and postoperatively19). To determine the Cobb's angle, measurements were taken from the superior endplate of the vertebra one level above the treated vertebra to the inferior endplate of the vertebral body one level below the treated vertebra. The local kyphotic angle was the angle in degree defined by the intersection of superior and inferior endplate of the fractured body (Fig. 1). The preoperative and postoperative angles were compared using paired t-tests statistically. The Frankel neurological performance scale was also evaluated to compare the preoperative or postoperative neurological status of the patients who sustained traumatic spinal fractures.
Fig. 1.
The measurement of kyphotic angle19).
Operative Technique
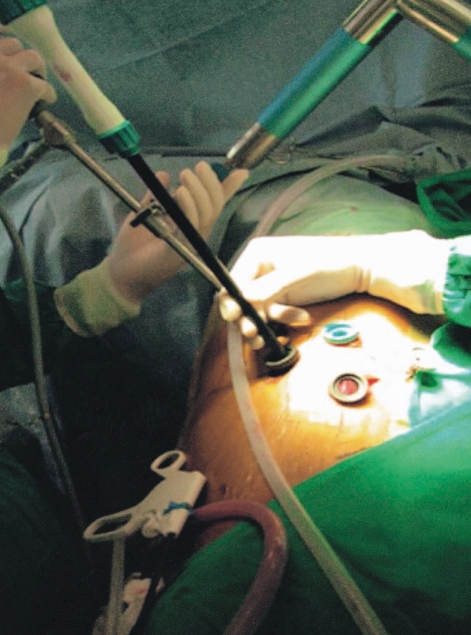
Under general anesthesia using a double lumen endotracheal intubation for one lung ventilation, the patients were positioned in the lateral decubitus position on the operating table. The portal placement was one of the most important procedures for successful thoracoscopic surgery. In the upper thoracic spine, the initial trocar incision was made at the fourth intercostal space along the anterior axillary line to avoid the brachial plexus. The other two manipulating channels were positioned at the posterior axillary line at the T2-3 and T3-4 intercostal space (ICS). In the middle thoracic or thoracolumbar junction lesion, the working channel was centered over the target vertebrae and the optical channel was placed two or three intercostal spaces cranial to the target vertebra. The approach for suction and irrigation or retractor was placed approximately 5 to 10 cm anterior to the working and optical channel. Another approach for diaphragm retraction was placed at the posterior axillary line at T9-T10 ICS. Thus the shape of the positioned portals were a diamond shape (Fig. 2).
Fig. 2.
Operative picture of the thoracoscopic portal placement to access level of T12 vertebra.
The parietal pleura over the level of the spinal pathology was incised and mobilized to expose the spine. To access the spinal canal, the rib head and proximal 2 to 3 cm of ribs of the target lesion were removed to expose the pedicles of the affecting vertebra. The pedicles were key landmarks for identifying the lateral margin of the spinal canal. The ipsilateral pedicle was removed after dissection of the rib to expose the dura. After the dura had been exposed and identified, the discectomy or corpectomy and interbody fusion were performed in affected site. To perform thoracoscopic discectomy, only the superior part of the pedicle was removed. If the disc had migrated caudally, the entire pedicle was resected.
The video assisted mini-thoracotomy procedure was also performed for effective corpectomy and interbody fusion using one or two thoracoscopic ports and a mini-skin incision (minithoracotomy). A mini-skin incision (5-7 cm) was made obliquely along the intercostal space at the level of the lesion without rib resection and retraction. Under video-assisted thoracoscopy, which provided better illumination and magnification, effective decompression and fusion could be performed through the minithoracotomy working port which provided better 3D visualization during surgery.
RESULTS
Stand-alone thoracoscopic discectomy
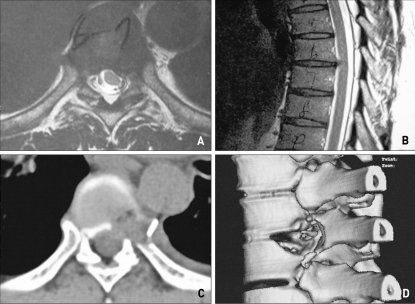
All three patients who had thoracic disc herniation underwent stand-alone thoracoscopic discectomy due to radiculopathy (1 case) and combined myelopathy with radiculopathy (2 cases). Postoperativelytheir symptoms and sign were significantly improved. Although pediculotomy and vertebrotomy were performed, the postoperative 3 dimensional CT scan demonstrated the degrees of the pediculotomy and vertebrotomy for the satisfactory decompression of the thoracic disc herniation (Fig. 3). The preoperative average of VAS score was 7.5 and it was improved to 1.5 postoperatively.
Fig. 3.
A case of 47 years old male patient with thoracic herniated nucleus pulposus. Preoperative MRI shows extruded disc compressing nerve root at the level of T6-7, left side (A, B). T2-weighted axial (A) and T2-weighted sagittal (B). Postoperative CT scan demonstrates satisfactory decompression of the T7 vertebra and rib head with disc space at T6-7 level (C, D).
Stand-alone thoracoscopic fusion versus video assisted mini-thoracotomy (VAMT)
We performed stand-alone thoracoscopic fusion in 11 patients. All patients had complete bony fusion without affecting kyphotic angle. Nine patients had traumatic spinal fractures, one patient had tuberculosis spondylitis of the thoracic spine, and the other one had thoracic disc herniation. The instruments were Z-plate (1 case), MACS-TL® (2 cases) and Antares® (6 cases). The mean length of surgery was 491 minutes and the mean blood loss was 1700 ml.
The video assisted mini-thoracotomy was performed for the six patients who had traumatic spinal fracture or dislocation (4 cases), multiple myeloma with severe kyphotic angle (1 case) and postoperative kyphosis (1 case). Early on in our clinical experiences of video assisted minithoracotomy spinal surgery until 2003, we used the Kaneda system (4 cases) and Z-plate (1 case).
The overall VAS score was significantly improved from 8.8 to 2.4. The minithoracotomy was useful for correction of the kyphotic deformity, effective decompression and restoration of the anterior column.
Clinical outcomes of spinal trauma
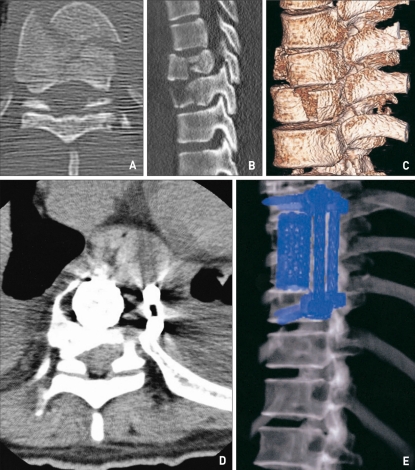
We performed thoracoscopic spinal fusion for traumatic spinal instability : compression fracture with ligament injury (6 cases), fracture and dislocation (3 cases), and bursting fracture (4 cases). A total of 13 patients were classified into five groups by using the Frankel neurological performance scale grade; grade E for five patients (38%), which is no motor or sensory deficits, grade D for two patients (15%) which is preservation of useful function distal to injury, grade C for two patients (15%) which is non-useful motor function distal to injury, grade B for one patients (8%) which is complete motor paralysis, but some residual sensory perception below the lesion, and grade A for three patients (23%) which is complete neurological injury. Postoperatively, four patients showed neurological significant improvement; two patients improved from C to E, one patients improved from grade D to E and one patient was improved from grade B to grade D. The patient who had complete spinal cord injury (Grade A) did not have any neurological improvement postoperatively (Table 2). One patient who had delayed postoperative kyphosis and myelopathy also did not show significant improvement after surgery (Fig. 4).
Table 2.
Frankel grades in trauma patients
Fig. 4.
A case of 38 years old female patient, preoperative 3D computer tomography (CT) scan shows bursting fractures at the level of T8 and T9 (A, B, C). Postoperative 3D CT scan demonstrates stable anterior column structure and fixation (D, E).
The preoperative Cobb and kyphotic angle were 18.9±4.4° and 18.8±4.6° respectively. Postoperative deformity angles were statistically improved to 15.1±3.7° and 11.3 ±2.4°, respectively (p<0.001) (Table 3). The average VAS score was also improved from 8.9 to 2 (preoperative and postoperative, retrospectively).
Table 3.
The Cobb angle and Kyphotic angle in the preoperative and postoperative status. (Trauma patients n=13)
Complications
There were three transient postoperative complications, including transitional pleural effusion, chylothorax followed by paraspinal abscess, and CSF leak. The pleural effusion was improved by repeated thoracentesis. The CSF leak due to dural laceration during surgery was improved by prolonged indwelling catheter and lumbar drainage. One patient who sustained a thoracolumbar burst fracture showed postoperative chylothorax due to traumatic injury of the thoracic duct. To treat the chylothorax, we maintained the patient with hyperalimentation for only 2 weeks. Eventually, he showed spiking fever, and postoperative MRI revealed paraspinal abscess formation. By revision of the operating wound with drainage of the abscess pocket using thoracoscopy and closed wound irrigation through a chest tube, the patient recovered from wound infection and chylothorax.
DISCUSSION
Video-assisted thoracoscopic surgery was developed in the late 1980s by cardiothoracic surgeons to decrease the morbidity of the open thoracotomy approach3,23). In the early 1990s, VATS techniques were applied to the treatment of spinal disease simultaneously by both Rosenthal et al. in Germany and Mack et al. in the United States23,27). Recently VATS have been used for management of thoracic and thoracolumbar junction pathologies, including thoracic disc herniation, fractures, tuberculosis spondylitis, idiopathic scoliosis, neuromuscular spinal deformity, congenital scoliosis, tumors1,2,4,6,8-18,21,25,26,29,30).
Using thoracoscopic surgery, anterior and anterolateral reconstruction can be performed to provide effective anterior load-bearing. In addition, thoracoscopic surgery provides small thin incisions without the need for rib resection or rib retractors, excellent direct intraoperative visualization of the abnormality, treatment of multisegmental abnormality without the need for additional rib resection, avoidance of division of the diaphragm and significantly reduced injury to the chest wall6,17). This procedure offers reduction of pain, better cosmetic effect, lower perioperative morbidity and an earlier return to normal activity4,6,8,10,16-18,25-27,29,30). The most significant disadvantage of VATS procedures is an extremely steep learning curve for proper thoracoscopic surgery technique; such as, establishing proper operative orientation under the angled 2-dimensional endoscopic image and performing the operation through the smaller portals with long surgical instruments at longer distances from the target area10,12,16-18,25,26,28).
The posterior elements, the contralateral pedicle, or contralateral transverse process cannot be exposed30). The costs for thoracoscopic instrumentation are high11,22). However, the learning curve associated with thoracoscopic spinal instrumentation appears to be acceptable22). The most common complication of VATS is intraoperative bleeding due to damage of the segmental vessels and intercostal vessels14). Although ligation of the segmental vessels is a time-consuming procedure, it eliminates catastrophic intraoperative or postoperative bleeding. It is important to identify the segmental vessels during the procedure at the midportion of the vertebral body. Transient intercostal neuralgia is the second most common complication, but it usually resolves spontaneously in one to 2 weeks. Other complications are related to pulmonary atelectasis or pleural effusions and these occur much less often than with an open procedure. Postoperative chylothorax is an uncommon complication, but a potentially lethal disorder14).
The author treated a patient who had post-traumatic or intraoperative chylothorax. It was successfully managed with prolonged indwelling chest tube and mid-chain triglyceride diet; however, the patient showed intermittent spiking high fever 14 days postoperatively due to paraspinal abscess formation caused by the long-standing malnourished status to treat chylothorax. The postoperative abscess formation was treated with re-exploratory thoracoscopic abscess drainage and irrigation with the use of closed suction-irrigation circuit.
VATS has many benefits compared to an open procedure, but the open procedure will still have a place for stabilization of the anterior column because of the steep learning curve. The video-assisted mini-thoracotomy provides a 3-dimensional operative image and wide space for manipulation of long instruments. Until 2003, only the Z-plate system or the Kaneda system were available for anterior fixation. The disadvantage of applying a plate system is that it is hard to apply and to correct coronal displacement or deformity caused by spinal trauma. However, anterior screw-rod systems can offer better stability to correct coronal spinal deformity and they make it easy to perform anterior spinal fixation compared with using plate systems. Since 2003, various thoracoscopic implants and instrumentations have been available such as MACS-TL® and Antares®, a dual-rod fixation system which is designed to be introduced thoracoscopically and assembled within the chest cavity using longer instruments. These systems decrease the instrumentation-related delays and difficulties substantially and serve biomechanical stability9,17).
Conclusively, the dual-rod system is the most useful instruments for performing thoracoscopic spinal surgery in terms of manipulation and application of the instrument to the deformed post-traumatic spine. Video assisted minithoracotomy using a dual-rod system is considered to be the most effective procedure for management of thoracic and thoracolumbar pathologies to correct post-traumatic spinal deformity. Recently, expandable interbody fusion devices are also available to correct some degree of sagittal deformity (kyphosis). The authors prefer to perform video-assisted mini-thoracotomy using expandable interbody devices and dual rod systems for direct anterior decompression and reconstruction.
CONCLUSION
Using VATS, the postoperative thoracotomy pain can be significantly reduced with lower perioperative morbidity and an earlier return to normal activity. Although spinal surgery using VATS requires a steep learning curve, it nevertheless provides effective anterior column decompression and short segment fusion and fixation with a minimally invasive approach.
References
- 1.Al-Sayyad MJ, Crawford AH, Wolf RK. Early experiences with video-assisted thoracoscopic surgery : our first 70 cases. Spine. 2004;29:1945–1951. doi: 10.1097/01.brs.0000137285.55865.c0. [DOI] [PubMed] [Google Scholar]
- 2.Benli IT, Alanay A, Akalin S, Kis M, Acaroglu E, Ates B, et al. Comparison of anterior instrumentation systems and the results of minimum 5 years follow-up in the treatment of tuberculosis spondylitis. Kobe J Med Sci. 2004;50:167–180. [PubMed] [Google Scholar]
- 3.Coltharp WH, Arnold JH, Alford WC, Jr, Burrus GR, Glassford DM, Jr, Lea JW, et al. Videothoracoscopy : improved technique and expanded indications. Ann Thorac Surg. 1992;53:776–778. doi: 10.1016/0003-4975(92)91434-b. [DOI] [PubMed] [Google Scholar]
- 4.Connelly CS, Manges PA. Video-assisted thoracoscopic discectomy and fusion. AORN J. 1998;67:940–952. doi: 10.1016/s0001-2092(06)62619-7. [DOI] [PubMed] [Google Scholar]
- 5.Das K, Rothberg M. Thoracoscopic surgery : historical perspectives. Neurosurg Focus. 2000;9:E10. doi: 10.3171/foc.2000.9.4.10. [DOI] [PubMed] [Google Scholar]
- 6.Dickman CA, Rosenthal D, Karahalios DG, Paramore CG, Mican CA, Apostolides PJ, et al. Thoracic vertebrectomy and reconstruction using a microsurgical thoracoscopic approach. Neurosurgery. 1996;38:279–293. doi: 10.1097/00006123-199602000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Fessler RG, Sturgill M. Review : complications of surgery for thoracic disc disease. Surg Neurol. 1998;49:609–618. doi: 10.1016/s0090-3019(97)00434-5. [DOI] [PubMed] [Google Scholar]
- 8.Han PP, Kenny K, Dickman CA. Thoracoscopic approaches to the thoracic spine : experience with 241 surgical procedures. Neurosurgery. 2002;51(Suppl):88–95. [PubMed] [Google Scholar]
- 9.Horn EM, Henn JS, Lemole GM, Jr, Hott JS, Dickman CA. Thoracoscopic placement of dual-rod instrumentation in thoracic spinal trauma. Neurosurgery. 2004;54:1150–1153. doi: 10.1227/01.neu.0000119229.92157.66. [DOI] [PubMed] [Google Scholar]
- 10.Huang TJ, Hsu RW, Liu HP, Hsu KY, Liao YS, Shih HN, et al. Video-assisted thoracoscopic treatment of spinal lesions in the thoracolumbar junction. Surg Endosc. 1997;11:1189–1193. doi: 10.1007/s004649900566. [DOI] [PubMed] [Google Scholar]
- 11.Huang TJ, Hsu RW, Liu HP, Liao YS, Hsu KY, Shih HN. Analysis of techniques for video-assisted thoracoscopic internal fixation of the spine. Arch Orthop Trauma Surg. 1998;117:92–95. doi: 10.1007/BF00703451. [DOI] [PubMed] [Google Scholar]
- 12.Huang TJ, Hsu RW, Liu HP, Liao YS, Shih HN. Technique of video-assisted thoracoscopic surgery for the spine : new approach. World J Surg. 1997;21:358–362. doi: 10.1007/pl00012253. [DOI] [PubMed] [Google Scholar]
- 13.Huang TJ, Hsu RW, Liu HP, Shih HN, Liao YS, Hsu KY, et al. Video-assisted thoracoscopic surgery to the upper thoracic spine. Surg Endosc. 1999;13:123–126. doi: 10.1007/s004649900919. [DOI] [PubMed] [Google Scholar]
- 14.Huang TJ, Hsu RW, Sum CW, Liu HP. Complications in thoracoscopic spinal surgery : a study of 90 consecutive patients. Surg Endosc. 1999;13:346–350. doi: 10.1007/s004649900987. [DOI] [PubMed] [Google Scholar]
- 15.Ishikawa E, Matsumura A, Ishikawa S, Nakamura K, Nose T. Combined minimallyinvasive approach using microsurgery and thoracoscopic surgery for resecting a dumbbell-type thoracic schwannoma. Minim Invasive Neurosurg. 2002;45:251–253. doi: 10.1055/s-2002-36201. [DOI] [PubMed] [Google Scholar]
- 16.Johnson JP, Filler AG, Mc Bride DQ. Endoscopic thoracic discectomy. Neurosurg Focus. 2000;9:E11. [PubMed] [Google Scholar]
- 17.Khoo LT, Beisse R, Potulski M. Thoracoscopic-assisted treatment of thoracic and lumbar fractures : a series of 371 consecutive cases. Neurosurgery. 2002;51(Suppl):S104–S117. [PubMed] [Google Scholar]
- 18.Kim DH, Jahng TA, Balabhadra RS, Potulski M, Beisse R. Thoracoscopic transdiaphragmatic approach to thoracolumbar junction fractures. Spine J. 2004;4:317–328. doi: 10.1016/j.spinee.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Kuklo TR, Polly DW, Owens BD, Zeidman SM, Chang AS, Klemme WR. Measurement of thoracic and lumbar fracture kyphosis : evaluation of intraobserver, interobserver, and technique variability. Spine. 2001;26:61–65. doi: 10.1097/00007632-200101010-00012. [DOI] [PubMed] [Google Scholar]
- 20.Levin R, Matusz D, Hasharoni A, Scharf C, Lonner B, Errico T. Mini-open thoracoscopically assisted thoracotomy versus video-assisted thoracoscopic surgery for anterior release in thoracic scoliosis and kyphosis : a comparison of operative and radiographic results. Spine J. 2005;5:632–638. doi: 10.1016/j.spinee.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Lonner BS, Kondrachov D, Siddiqi F, Hayes V, Scharf C. Thoracoscopic spinal fusion compared with posterior spinal fusion for the treatment of thoracic adolescent idiopathic scoliosis. Surgical technique. J Bone Joint Surg Am. 2007;89(Suppl):142–156. doi: 10.2106/JBJS.F.01389. [DOI] [PubMed] [Google Scholar]
- 22.Lonner BS, Scharf C, Antonacci D, Goldstein Y, Panagopoulos G. The learning curve associated with thoracoscopic spinal instrumentation. Spine. 2005;30:2835–2840. doi: 10.1097/01.brs.0000192241.29644.6e. [DOI] [PubMed] [Google Scholar]
- 23.Mack MJ, Aronoff RJ, Acuff TE, Ryan WH. Thoracoscopic transdiaphragmatic approach for adrenal biopsy. Ann Thorac Surg. 1993;55:772–773. doi: 10.1016/0003-4975(93)90295-s. [DOI] [PubMed] [Google Scholar]
- 24.Mack MJ, Regan JJ, Bobechko WP, Acuff TE. Application of thoracoscopy for diseases of the spine. Ann Thorac Surg. 1993;56:736–738. doi: 10.1016/0003-4975(93)90966-l. [DOI] [PubMed] [Google Scholar]
- 25.Mack MJ, Regan JJ, McAfee PC, Picetti G, Ben-Yishay A, Acuff TE. Video-assisted thoracic surgery for the anterior approach to the thoracic spine. Ann Thorac Surg. 1995;59:1100–1106. doi: 10.1016/0003-4975(95)00112-x. [DOI] [PubMed] [Google Scholar]
- 26.Niemeyer T, Freeman BJ, Grevitt MP, Webb JK. Anterior thoracoscopic surgery followed by posterior instrumentation and fusion in spinal deformity. Eur Spine J. 2000;9:499–504. doi: 10.1007/s005860000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenthal D, Dickman CA. Thoracoscopic microsurgical excision of herniated thoracic discs. J Neurosurg. 1998;89:224–235. doi: 10.3171/jns.1998.89.2.0224. [DOI] [PubMed] [Google Scholar]
- 28.Rosenthal D, Rosenthal R, de Simone A. Removal of a protruded thoracic disc using microsurgical endoscopy. A new technique. Spine. 1994;19:1087–1091. doi: 10.1097/00007632-199405000-00018. [DOI] [PubMed] [Google Scholar]
- 29.Son-Hing JP, Blakemore LC, Poe-Kochert C, Thompson GH. Video-assisted thoracoscopic surgery in idiopathic scoliosis : evaluation of the learning curve. Spine. 2007;32:703–707. doi: 10.1097/01.brs.0000257528.89699.b1. [DOI] [PubMed] [Google Scholar]
- 30.Visocchi M, Masferrer R, Sonntag VK, Dickman CA. Thoracoscopic approaches to the thoracic spine. Acta neurochirurgica. 1998;140:737–743. doi: 10.1007/s007010050174. [DOI] [PubMed] [Google Scholar]