Abstract
Objective
The objective of this study is to investigate the safety, surgical efficacy, and advantages of a polyaxial screw-rod system for posterior occipitocervicothoracic arthrodesis.
Methods
Charts and radiographs of 32 patients who underwent posterior cervical fixation between October 2004 and February 2006 were retrospectively reviewed. Posterior cervical polyaxial screw-rod fixation was applied on the cervical spine and/or upper thoracic spine. The surgical indication was fracture or dislocation in 18, C1-2 ligamentous injury with trauma in 5, atlantoaxial instability by rheumatoid arthritis (RA) or diffuse idiopathic skeletal hyperostosis (DISH) in 4, cervical spondylosis with myelopathy in 4, and spinal metastatic tumor in 1. The patients were followed up and evaluated based on their clinical status and radiographs at 1, 3, 6 months and 1 year after surgery.
Results
A total of 189 screws were implanted in 32 patients. Fixation was carried out over an average of 3.3 spinal segment (range, 2 to 7). The mean follow-up interval was 20.2 months. This system allowed for screw placement in the occiput, C1 lateral mass, C2 pars, C3-7 lateral masses, as well as the lower cervical and upper thoracic pedicles. Satisfactory bony fusion and reduction were achieved and confirmed in postoperative flexion-extension lateral radiographs and computed tomography (CT) scans in all cases. Revision surgery was required in two cases due to deep wound infection. One case needed a skin graft due to necrotic change. There was one case of kyphotic change due to adjacent segmental degeneration. There were no other complications, such as cord or vertebral artery injury, cerebrospinal fluid leak, screw malposition or back-out, or implant failure, and there were no cases of postoperative radiculopathy due to foraminal stenosis.
Conclusion
Posterior cervical stabilization with a polyaxial screw-rod system is a safe and reliable technique that appears to offer several advantages over existing methods. Further biomechanical testings and clinical experiences are needed in order to determine the true benefits of this procedure.
Keywords: Cervical spine, Lateral mass, Polyaxial screw-rod
INTRODUCTION
Posterior stabilization of the cervical spine is a common surgical procedure which is used in a variety of spinal disorders, including cervical spondylosis, postsurgical deformity or instability, tumor and trauma5). Of the numerous techniques for stabilizing the cervical spine, transpedicular screw fixation allows three column fixation with more stable architecture, and insertion into pedicle that gives better bony purchase than insertion into lateral mass. However, pedicle screw fixation is technically more difficult than other methods, and perforation of cortical bone is possible23). In addition, screw placement can cause injuries to adjacent vital structures such as the spinal cord or vertebral artery. Lateral mass plate and screw devices have been proven to be safe in spite of their proximity to neurovascular structures. However, posterior plate-screw techniques can be associated with potential problems, including injuries to the vertebral artery, nerve root, spinal cord and facet joint6,8,9,13,14,21,22). Also, the plates are difficult to contour and screw position is constrained by the plate's entry holes. Screw back-out can also occur, and the plate systems are not easily adapted for extension to the occiput or thoracic spine18). Moreover, there is a risk of implant failure and loss of alignment9).
The authors report the clinical experiences of cervical stabilization with a polyaxial screw-rod system and investigate the safety, surgical efficacy, and advantages of a polyaxial screw-rod system for posterior occipitocervicothoracic arthrodesis that addresses some of the limitations associated with lateral mass plating.
MATERIALS AND METHODS
Patient demographics
This study was based on the charts and radiological records of 32 patients who were treated at our institution. The patients were operated from October 2004 to February 2006, and all patients were treated by posterior cervical fixation using a polyaxial screw-rod system. There were 21 men and 11 women (age range, 19 to 74 years; mean, 47.3 years). Preoperative diagnoses included cervical spondylosis with myelopathy in 4, fracture or dislocation in 18, C1-2 ligamentous injury with trauma in 5, atlantoaxial instability by RA or DISH in 4, spinal metastatic tumor in 1 (Fig. 1). The patient characteristics are recorded in Table 1.
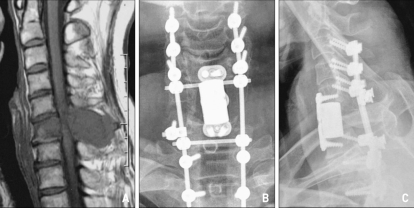
Fig. 1.
A 43-year-old patient with quadriparesis and a history of hepatocellular carcinoma. Preoperative magnetic resonance image showing an expansile bony lesion involving the body and posterior elements of the C6 vertebra with marked compression of the spinal cord (A). He underwent radical tumor resection including the body of C6 and anterior and posterior reconstruction at the level of C3-T2 using a titanium mesh and plate and the polyaxial screw-rod system (B), (C).
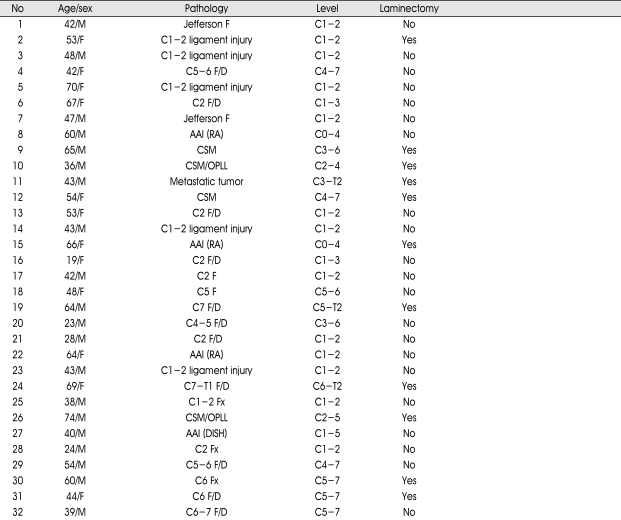
Table 1.
Clinical and demographic data of the patients in this study
AAI : atlantoaxial instability, Ant : anterior, CSM : cervical spondylotic myelopathy, DISH : diffuse idiopathic skeletal hyperostosis, DWI : deep wound infection, F/D : fracture/dislocation, F : fracture, OPLL : ossification of posterior longitudinal ligament, postop : postoperative, RA : rheumatoid arthritis
Surgical technique
With the patient in the prone position, a vertical midline posterior cervical incision was made. Exposure of the lateral masses was done in a sub- periosteal fashion to the lateral margins of the facet joints. The motion segments to be fused had their facet joints above and below the instrumented levels. With the aid of digital fluoroscopy, screws were placed in the lateral mass of C1, pars interarticularis of C2, the lateral masses of C3-C6, the lateral mass or pedicle of C7 and the upper thoracic pedicles, depending on the needs of each individual. The majority of the screws were 14 mm in length, and the length of the screws ranged from 10 to 32 mm. The standard screw diameter was 3.5 mm, and the diameter of the rescue screw was 4.0 mm. The screws were placed after decompressive laminectomy.
The entry point was 1 mm medial to the midpoint of the lateral mass. The screws were angulated 30-40 degrees laterally and superiorly in an attempt to attain the best purchase of the lateral mass with minimal risk of neural or vascular injury, which is a modification of the An technique22). A rod was cut to the appropriate length and contoured, so that it would easily pass through the heads of all polyaxial screws. This process was facilitated by adjusting the orientation of the heads of the polyaxial screws using tools especially made for that purpose. Once the rod was positioned, it was captured to the heads of the screws using outer nuts or set screws. Each segment was distracted or compressed, as needed, before the final tightening. In most cases, morcellized local autograft bone from the posterior elements and an allobone chip was placed over the decorticated lateral masses after the screws were in place. Routine closure was carried out, and the wounds were drained for 24 to 48 hours. The procedure was easily adapted for occipitocervical and cervicothoracic stabilization, and was used in conjunction with combined anterior-posterior procedure as needed. The Vertex Reconstruction System (Medtronic Sofamor Danek, Memphis, TN) was used in all cases.
RESULTS
Thirty-two patients underwent posterior cervical arthrodesis. A total of 189 screws were implanted in all patients. The mean number of levels fused was 3.3 (range, 2 to 7). The mean follow-up interval was 20.2 months. Laminectomy was performed in 11 patients, and concomitant anterior reconstructive surgery was performed in 6 patients.
The polyaxial screw-rod system was successfully implanted in all patients despite the presence of coronal and sagittal plane deformities and/or lateral mass abnormalities in the majority of the patients. This system allowed for screw placement in the occiput, C1 lateral mass, C2 pars, C3-7 lateral mass, as well as the lower cervical and upper thoracic pedicles.
The patients were followed-up and were evaluated based on their clinical status and radiographs at 1, 3, 6 months, and 1 year after surgery. Satisfactory bony fusions and reductions were achieved and confirmed by postoperative flexion-extension lateral radiographs and CT scans in all patients, with the exception of 2 cases due to a lack of follow up data.
One patient underwent a skin graft due to necrotic change. Two patients underwent a revision surgery due to a deep wound infection. There was one case of kyphotic change due to adjacent segment degeneration. That patient is under observation because the patient do not have any symptom. There were no complications, such as cord or vertebral artery injury, cerebrospinal fluid leakage, screw back-out, or implant failure, and there were no cases of postoperative radiculopathy due to foraminal stenosis after reduction of dislocation.
DISCUSSION
Posterior stabilization of the cervical spine has been performed using a variety of techniques. Traditionally2,11), posterior fixation of the cervical spine has involved some forms of wire fixation. Wire fixation is inexpensive, has a proven long-term track record, and requires no special expertise or X-ray guidance1,3,4,7,16). However, wire fixation falls short in treating the osteoporotic patient, where solid immediate stabilization is required, where the posterior elements have been removed or are compromised, or where forces other than pure fixation need to be counteracted5,8,10,17). Unlike newer titanium plate or screw and rod constructs, stainless-steel wires can also interfere with postoperative magnetic resonance imaging19).
Lateral mass plating has been shown to be a useful and suitable alternative to wiring in posterior cervical arthrodesis8). This method requires the use of plates and monoaxial screws to attach the lateral masses of the subaxial cervical spine and the pars interarticularis of C215). Although lateral mass plating represents a major advancement in posterior cervical stabilization, it has some limitations. One shortcoming of this method is that it may be difficult to contour an appropriate plate for patients who have abnormal curvatures due to the degenerative cervical spondylosis. Another shortcoming is that implant failure, loss of alignment, and screw back-out can occur if the screw is not tightly fixed to the plate9). It is also not easy to extend fusion up to the occiput or down to the thoracic spine. Some require a bulky connector device at the cervicothoracic junction; however, cervicothoracic fusion can decrease the rigidity of the system. There are several other problems associated with plating techniques. The fixed hole spacing of the plate makes it quite difficult to place the screw at the ideal position. Lateral mass screw placement must be precise because it can injur the spinal cord, nerve roots and vertebral artery if not done properly, and thus it can be a very risky procedure. Another concern is postoperative radiculopathy, which has been attributed to iatrogenic foraminal stenosis resulting from a lag screw effect5,9).
To overcome with these shortcomings, the polyaxial screw-rod system has been developed. Several authors have reported preliminary data to support the use of this technique throughout the cervical spine, including extension to the occiput and upper thoracic lesion10,18). There are several advantages of screw and rod fixation comparing to plating technique. One advantage is that the rods are much more flexible and allow for the multiplanar contouring of deformities associated with cervical spondylosis. Another strength of this method is that no cases of implant failure have been reported. The head of the polyaxial screw is tightly fixed to the rod in order to prevent screw back-out. In addition, it is easier to extend to the occiput and across the cervicothoracic junction using the screw and rod system (Fig. 2). There are other advantages of the polyaxial screw rod system. The screw placement is more delicate and precise using this method because there is a greater chance of placing the screw at the ideal position without having to make a hole in the plate. It is obvious that the screw-rod system is more flexible and can be used to treat lateral masses of various size, spacing and morphology. An additional advantage of the polyaxial screw-rod system is that it allows for compression, distraction, and reduction forces to be easily applied within the construct5).
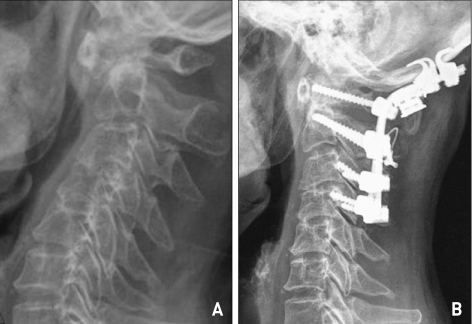
Fig. 2.
A 66-year-old woman presented with quadriparesis. She had a history of rheumatoid arthritis. Preoperative lateral radiograph demonstrating a poorly visualized odontoid process with widening of the C1-2 joint (A). Postoperative lateral radiograph revealing an occipitocervical fusion with the polyaxial screw-rod system (B).
The screw-rod system has been adapted for cervicothoracic fusion with dual diameter rods. This allows for lateral mass screw fixation in the cervical spine and standard pedicle screw or hook fixation in the thoracic spine to be performed using a single rod. The screw-rod system could be applied to the reduction of not only atlantoaxial subluxation but also dislocation of the subaxial spine (Fig. 3). When the lateral mass was violated or broken while it was being prepared for the insertion of the screw, it was possible to avoid a crisis by using a rescue screw with diameter of 4.0 mm or by changing the surgical technique into pedicle screw fixation. When operating on tumors located in the ventral or ventrolateral portion of the cervical or cervicothoracic spine, this system can play a role in temporary fixation at the contralateral side during the operation in order to avoid intraoperative instability caused by the compromise of the anterior column.
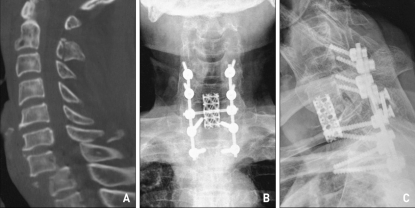
Fig. 3.
A 64-year-old man with quadriparesis after trauma. Preoperative sagittal computed tomography scan demonstrating fracture and dislocation at thelevel of C7-T1 (A). Postoperative anteroposterior and lateral radiographs revealing the completed posterior screw and rod construct with concomitant C7 corpectomy and anterior interbody fusion with titanium mesh (B), (C).
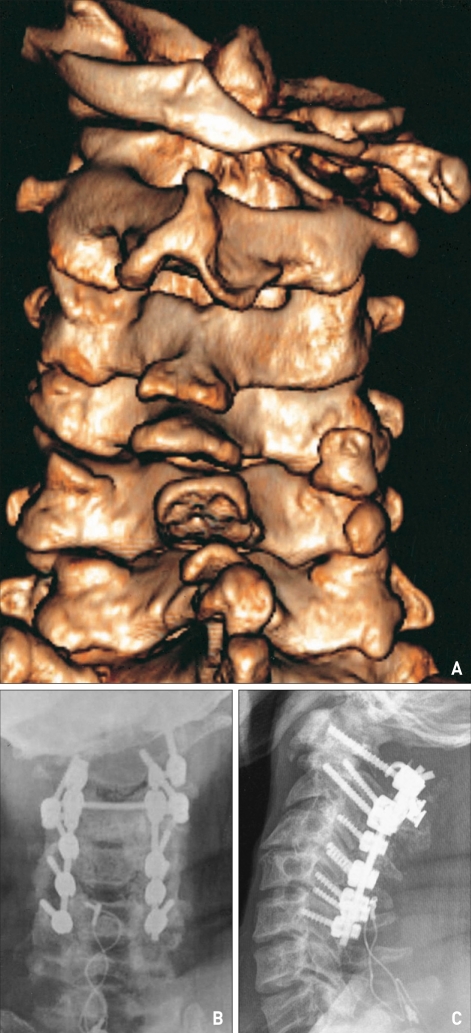
The screw-rod system can also be used with C1 lamina hook when the screw cannot be inserted into the lateral mass of C1 due to the presence of several eroded lateral masses caused by inflammation, such as RA or DISH (Fig. 4).
Fig. 4.
A 40-year-old man presented with quadriparesis. He had cerebral palsy and a history of diffuse idiopathic skeletal hyperostosis. Preoperative three-dimensional computed tomography reconstruction shows right atlas lateral mass erosion and atlantoaxial subluxation (A). He underwent atlantoaxial fixation with C1 lamina hook and lateral connector due to C1 lateral mass erosion (B), (C).
Wellman et al.20) reported that the average vertical distance between the posterior midpoint of the lateral mass and the vertebral foramen from C3 to C6 has been found to be approximately 9-12 mm. In this study, the majority of the screws were 14 mm in length because we believed that 14 mm screws positioned obliquely would adequately span the lateral mass.
CONCLUSION
Posterior cervical stabilization with polyaxial screw and rod system is a safe and reliable technique that appears to offer several advantages over existing methods. We have successfully used this system in 32 patients to achieve posterior cervical arthrodesis, with minimal complications. Further biomechanical testing and clinical experience are needed in order to determine the true benefits of the procedure.
References
- 1.An HS, Coppes MA. Posterior cervical fixation for fracture and degenerative disc disease. Clin Orthop. 1997;335:101–111. [PubMed] [Google Scholar]
- 2.Benzel EC, Kesterson L. Posterior cervical interspinous compression wiring and fusion for mid to low cervical spine injuries. J Neurosurg. 1989;70:893–899. doi: 10.3171/jns.1989.70.6.0893. [DOI] [PubMed] [Google Scholar]
- 3.Branch CL, Jr, Kelly DL, Jr, Davis CH, Jr, McWhorter JM. Fixation of fractures of the lower cervical spine using methylmethacrylate and wire : Technique and results in 99 patients. Neurosurgery. 1989;25:503–512. doi: 10.1097/00006123-198910000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Crockard A. Evaluation of spinal laminar fixation by a new, flexible stainless steel cable (Sof'wire) : early results. Neurosurgery. 1994;35:892–898. [PubMed] [Google Scholar]
- 5.Deen HG, Birch BD, Wharen RE, Reimer R. Lateral mass screw-rod fixation of the cervical spine : A prospective clinical series with 1-year follow-up. Spine J. 2003;3:489–495. [PubMed] [Google Scholar]
- 6.Ebraheim NA, Klausner T, Xu R, Yeasting RA. Safe lateral mass screw lengths in the Roy-Camille and Margerl techniques : an anatomic study. Spine. 1998;23:1739–1742. doi: 10.1097/00007632-199808150-00006. [DOI] [PubMed] [Google Scholar]
- 7.Geisler FH, Mirvis SE, Zrebeet H, Joslyn JN. Titanium wire internal fixation for stabilization of injury of the cervical spine : Clinical results and postoperative magnetic resonance imaging of the spinal cord. Neurosurgery. 1989;25:356–362. doi: 10.1097/00006123-198909000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Graham AW, Swank ML, Kinard RE, Lowery GL, Dials BE. Posterior cervical arthrodesis and stabilization with a lateral mass plate. Clinical and computed tomographic evaluation of lateral mass screw placement and associated complications. Spine. 1996;21:323–329. doi: 10.1097/00007632-199602010-00014. [DOI] [PubMed] [Google Scholar]
- 9.Heller JG, Silcox DH, Sutterrlin CE. Complications of posterior cervical plating. Spine. 1995;20:2442–2448. doi: 10.1097/00007632-199511001-00013. [DOI] [PubMed] [Google Scholar]
- 10.Horgan MA, Kellogg Jx, Chesnut RM. Posterior cervical arthrodesis and stabilization : an early report using a novel lateral mass screw and rod technique. Neurosurgery. 1999;44:1267–1272. [PubMed] [Google Scholar]
- 11.Jeanneret B, Margerl F, Ward EH, Ward JC. Posterior stabilization of the cervicl spine with hook plates. Spine. 1991;16:S56–S63. doi: 10.1097/00007632-199103001-00010. [DOI] [PubMed] [Google Scholar]
- 12.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws : anatomic feasibility and biomechanical comparison. Spine. 1997;22:977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 13.Jonsson H, Rauschning W. Anatomical and morphometric studies in posterior cervical spinal screw plate system. J Spinal Disord. 1994;7:429–438. [PubMed] [Google Scholar]
- 14.Lee DC, Yoon SH, Park HC, Park JO, Hyun DK, Park HS. Clinical and computed tomography evaluation of plate and screw on the cervical lateral mass : a modified Magerl's technique. J Korean Neurosurg Soc. 2006;39:251–255. [Google Scholar]
- 15.McCullen GM, Garfin SR. Spine update : cervical spine internal fixation using screw and screw-plate constructs. Spine. 1997;22:274–282. doi: 10.1097/00007632-200003010-00020. [DOI] [PubMed] [Google Scholar]
- 16.Mirvis SE, Geisler F, Joslyn JN, Zrebeet H. Use of titanium wire in cervical spine fixation as a means to reduce MR artifacts. AJNR Am J Neuroradiol. 1988;9:1229–1231. [PMC free article] [PubMed] [Google Scholar]
- 17.Muffoletto AJ, Hadjipavlou AG, Jensen RE, Nauta HJ, Necessary JT, Norcross-Nechay K. Techniques and pitfalls of cervical lateral mass plate fixation. Am J Orthop. 2000;29:897–903. [PubMed] [Google Scholar]
- 18.Mummaneni PV, Haid RW, Traynelis VC, Sasso RC, Subach BR, Fiore AJ, et al. Posterior cervical fixation using a new polyaxial screw and rod system : technique and surgical results. Neurosurg Focus. 2002;12:E8. doi: 10.3171/foc.2002.12.1.9. [DOI] [PubMed] [Google Scholar]
- 19.Sekhon LH. Posterior cervical lateral mass screw fixation. J Spinal Disord Tech. 2005;18:297–303. doi: 10.1097/01.bsd.0000166640.23448.09. [DOI] [PubMed] [Google Scholar]
- 20.Wellman BJ, Follett KA, Traynelis VC. Complications of posterior articular mass plate fixation of the subaxial cervical spine in 43 consecutive patients. Spine. 1998;23:193–200. doi: 10.1097/00007632-199801150-00009. [DOI] [PubMed] [Google Scholar]
- 21.Xu R, Ebraheim NA, Klausner T, Yeasting RA. Modified Magerl technique of lateral mass screw placement in the lower cervical spine : an anatomic study. J Spinal Disord. 1998;11:237–240. [PubMed] [Google Scholar]
- 22.Xu R, Haman SP, Ebraheim NA, Yeasting RA. The anatomic relation of lateral mass screws to the spinal nerves : a comparison of the Magerl, Anderson, and An techniques. Spine. 1999;24:2057–2061. doi: 10.1097/00007632-199910010-00016. [DOI] [PubMed] [Google Scholar]
- 23.Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T. Spinal reconstruction using a cervical pedicle screw system. Clin Orthop Relat Res. 2005;431:111–119. doi: 10.1097/01.blo.0000150321.81088.ab. [DOI] [PubMed] [Google Scholar]