Abstract
Objective
The current literature implies that the use of short-segment pedicle screw fixation for spinal fractures is dangerous and inappropriate because of its high failure rate, but favorable results have been reported. The purpose of this study is to report the short term results of thoracolumbar burst and compression fractures treated with short-segment pedicle instrumentation.
Methods
A retrospective review of all surgically managed thoracolumbar fractures during six years were performed. The 19 surgically managed patients were instrumented by the short-segment technique. Patients' charts, operation notes, preoperative and postoperative radiographs (sagittal index, sagittal plane kyphosis, anterior body compression, vertebral kyphosis, regional kyphosis), computed tomography scans, neurological findings (Frankel functional classification), and follow-up records up to 12-month follow-up were reviewed.
Results
No patients showed an increase in neurological deficit. A statistically significant difference existed between the patients preoperative, postoperative and follow-up sagittal index, sagittal plane kyphosis, anterior body compression, vertebral kyphosis and regional kyphosis. One screw pullout resulted in kyphotic angulation, one screw was misplaced and one patient suffered angulation of the proximal segment on follow-up, but these findings were not related to the radiographic findings. Significant bending of screws or hardware breakage were not encountered.
Conclusion
Although long term follow-up evaluation needs to verified, the short term follow-up results suggest a favorable outcome for short-segment instrumentation. When applied to patients with isolated spinal fractures who were cooperative with 3-4 months of spinal bracing, short-segment pedicle screw fixation using the posterior approach seems to provide satisfactory result.
Keywords: Pedicle screw instrumentation, Thoracolumbar fracture, Short-segment, Fixation
INTRODUCTION
Development of transpedicular screw fixation techniques and instrumentation systems has brought short-segment instrumentation (fixation of one normal vertebra above and below an injured segment) into general clinical practice22). After King25) initially reported vertebral body screw fixation through the transfacet approach to the lumbar spine in 1944, Boucher6) introduced the way to pierce screws into the vertebral body through the pedicle in 1958. Since pedicle screw fixation became widespread, as described by Roy-Camille35) and others in 1963, pedicle screws have been used widely in diseases of the lumbar spine18).
The optimal management of thoracolumbar fractures continues to be a matter of controversy2,4,31,37). The transpedicular short-segment construct represents an attempt to restore the anterior column without the need for anterior strut grafting or plate fixation, avoiding extensive arthrodesis of the motion segments. The use of pedicle screws, which can minimize the range of spinal segments to reduce damage to soft tissues and increase the rate of synostosis better than fixation using hooks and wires, expands the excellent functionalities of pedicle screws reported by studies26). To date, various unfavorable results have been reported with this method1,10,16). Those who suggest temporizing treatments insisted that they could achieve satisfactory results only by treatments using postures and long-term relaxations8,11,16,21). However, others who suggest surgical treatment, patients could expect to become mobile early, perform rehabilitative remedies, overcome anatomic fractures, restore swayback and improve, in most cases, nervous functions by using decompression and fixation1,7). After temporizing treatments, there were many reports on degrading nervous functions, worsening spinal stenosis, increasing pressure on the vertebral body, increasing kyphosis and causing radiculopathy, and pain10,29). This study evaluates and analyses the radiological outcome from short segment pedicle screw fixation in 19 patients with thoracolumbar spine fractures.
MATERIALS AND METHODS
Case materials
A retrospective review was performed in all surgically managed thoracolumbar fractures on various clinical parameters such as age, sex distribution, and cause and levels of injury. Consecutive thoracolumbar fractures from February 2000 to December 2006 were included. The short-segment transpedicular fixation was performed in 19 patients by three surgeons. Charts, operative notes, preoperative and postoperative radiographs, CT scans, MRI and follow-up records up to 12-month period were reviewed. Fractures were classified according to Denis10) (three-column classification). Neurological status was assessed using the Frankel/ASIA scale for spinal cord injury. Vertebral body injury was assessed by Load-sharing classification30).
Simple radiologic parameters were made for easier measurement and minimized interobserver bias. Sagittal index is the ratio of the anterior and posterior heights of the injured vertebral body on lateral view33). Sagittal plane kyphosis was measured between the inferior end plate of the injured segment and the superior end plate of the upper vertebral body33). Anterior body compression was measured preoperatively, postoperatively and at follow-up according to Mumford's anterior body compression30,33). Vertebral kyphosis was measured from the fractured vertebral body's superior end plate to its inferior end plate33). Regional kyphosis was measured from the inferior end plate of the intact vertebra above the fracture to the superior end plate of the intact vertebra below the fracture33). Follow-up assessment was done by radiographs. Simple X-ray was performed to check the fractures. Computed tomography and MRI were done for every patient to ensure accurate diagnosis of damage to the vertebra. Patients' complaints of pain were assessed using the pain scale of Denis10). Postoperative work status was also measured10).
Case selection
Indications for surgical instrumentation in this series included the presence of any one or more of the followings; neurological involvement caused by the fracture, kyphosis of more than 20 degrees, loss of more than 50% of the vertebral body's height, compromised spinal canals, or any other instability based on the criteria of unstable thoracolumbar fractures by McAfee et al.28). In highly comminuted fractures and severely midline retropulsed fragments (canal compromise ratio>0.7) with anticipated load sharing, operations were performed by ventral approach. Also, multiple fractures and severe pedicle fracture were excluded from this study.
Surgical method
Under general anesthesia on prone position, the skin of the midline was incised to expose the fractured part. From 1-2 vertebral bodies above the fractured site to one vertebral body below it, screw fixation and posterior-lateral synostosis were performed through bone fragments with autologous bone graft or allograft.
The length of screw fixation was from 2 to 4 segments and were fixed on the vertical segment including the fractured part. When the vertebral body and the pedicle were severely damaged and insertion of screws was difficult, screws were not inserted. When it was considered difficult to achieve stability with fixation of only the vertical segment because of a damaged posterior column in more than two segments, fixation was extended to four segments. If the bone fragment remained in the spinal canal, decompression followed by posterior pedicle fixation was done. After surgery, the patients started using wheelchairs and walking according to their clinical status and degree of fracture and transposition. In addition, they also used an orthosis for approximately six months.
Analysis
The degrees of correction of vertebral transformation were compared and analyzed by sagittal index, sagittal plane kyphosis, anterior body compression, vertebral kyphosis and regional kyphosis preoperatively, postoperatively and 12 months after surgery by periodic simple radiography. Repeated ANOVA (Analysis of Variance) method was used by SPSS 13.0.
RESULTS
Short-segment transpedicular fixation was performed on 19 patients including 13 males and 6 females. Patients were monitored until 12-month follow-up evaluation. Mean age was 46 (range : 17-75). Males had 14 fractures and the most common site was L2 (Fig. 1). Females had seven fractures and the most common site was L1. Four fractures and dislocations were noted only in males (Fig. 2). According to the classification of nervous function by Frankel et al.17), the patients were included as one A, one B, two Cs, four Ds and 11 Es. Load-sharing classification revealed that four was the most common value observed. Bone graft was performed in an autograft to allograft ratio of 6:13.
Fig. 1.
A 62-year-old male with an L2 burst fracture. A : Preoperative lateral thoracolumbar spinal image. B : preoperative lumbar spine computed tomography axial image showing apposition of bony fragments into the spinal canal with laminar impingement. C : preoperative lumbar spine computed tomography sagittal image showing encroachment of spinal canal by bony segment. D : bone fragment was removed and posterior fixation was performed during surgery; postoperative lateral thoracolumbar spinal image showing restoration of the thoracolumbar alignment.
Fig. 2.
T12/L1 fracture and dislocation in a 72-year-old man as a result of a traffic accident. Patient was paraplegic. A : preoperative lateral thoracolumbar spinal image. B : preoperative lumbar spine computed tomography axial image. C : preoperative lumbar spine computed tomography sagittal image. D : postoperative lateral thoracolumbar spinal image shows short-segment reconstruction and healing in normal alignment.
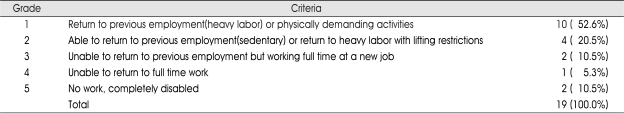
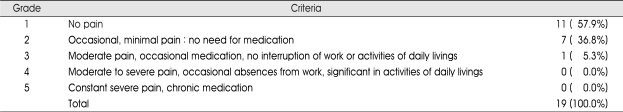
Patients were classified by Denis' et al's Work scale10). The patients were predominantly categorized in grade 1 (Table 1). Patients were also classified by Denis' et al's pain scale. There were no grades 4 or 5 (Table 2).
Table 1.
Distribution of patients classified by Denis et al.'s Work scale6)
Table 2.
Distribution of patients classified by Denis et al.'s Pain scale6)
One screw pullout resulted in kyphotic angulation. Two other complications were encountered; one screw was misplaced, and one patient suffered angulation of the proximal segment on follow-up. One patient complained of moderate pain and other was disabled by the initial spinal cord injury, but these findings were not related to the radiographic findings. Significant bending of screws or hardware breakage were not encountered. Initial progressive osseous collapse was noted in a paraplegic patient, but without increasing pain.
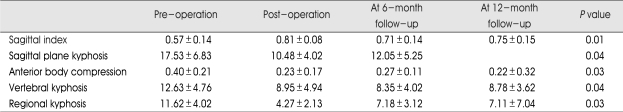
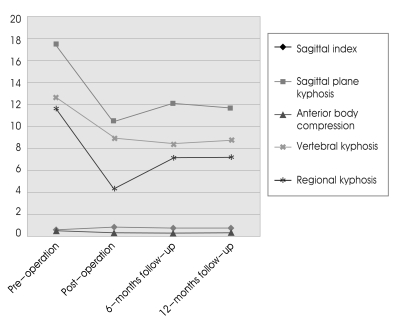
Sagittal index, sagittal plane kyphosis, anterior body compression, vertebral kyphosis and regional kyphosis were investigated by serial follow-up for 12 months. During this period, preoperative sagittal index increased after surgery, then decreased at the six-month follow-up and again increased at the 12-month follow-up. Each group's sagittal index was statistically significant (p-value=0.01). Preoperative sagittal plane kyphosis decreased after operation, then increased at six months and decreased at 12 months. Each group's value was statistically significant (p-value=0.04). Preoperative anterior body compression decreased after surgery, then increased at six months and decreased at 12 months (p=0.03). Preoperative vertebral kyphosis decreased after surgery, decreased more at the six-month follow-up, then increased at 12 months. This result was also statistically significant (p=0.04). Preoperative regional kyphosis decreased after surgery, then increased at six months and decreased a little at 12 months with a statistical significance (p=0.03)(Table 3, Fig. 3).
Table 3.
Thoracolumbar fractures : Means and standard deviations of sagittal index, sagittal plane kyphosis, anterior body compression, vertebral kyphosis and regional kyphosis until the 12th post-operative month
Fig. 3.
The radiologic changes are shown until the 12-months follow-up. All parameters are statistically significant.
DISCUSSION
The purposes of treating vertebral fractures are to achieve early neurological restoration, overcome damaged spinal segments anatomically and accomplish firm and stable fixation for early rehabilitation27). Pedicle screw fixation of spinal fractures is performed as a basic treatment for thoracic and lumbar vertebral fractures and posterior-lateral synostosis in many hospitals1,5,11,13,21). Sasso et al.38) did clinical comparisons and analyses among Harrington rods, hooks, Luque rods, sublaminar wires and pedicle screws with 70 patients and found that pedicle screw fixation was a posterior fixation which could be applied to shorter segments than could other posterior fixation tools. Therefore, pedicle screw fixation is a good posterior fixation method suitable for this purpose23,24).
The main advantages of the dorsal approach in short-segment fixation are that it preserves the motion segment, and is simple and familiar to spine surgeons but a recognized disadvantage is the difficulty in restoring the anterior column. Failure to restore the anterior column support can lead to secondary kyphosis, instability, pain and late onset neurologic deficit, depending primarily on residual load transfer capacity of the fractured vertebral body24,29).
Some reports have indicated that sagittal plane kyphosis was incurable using pedicle screw fixation in thoracic and lumbar fractures due to bone breakdown by the follow-up examination at 12 months38). However, this study demonstrated a satisfactory results with no patient worsened neurologically after pedicle screw fixation.
Pedicle screws can be used both in the lumbar and thoracic vertebrae and are useful in severe fractures such as fracture-dislocation. Documented reports indicated the infection rate as approximately 6%36) after posterior fixation and synostosis, however, no infection was seen in this study.
Humford et al.12) reported that temporizing methods showed good results for patients with thoracic and lumbar segmented fractures without nerve damage. However, Denis et al.10) found that patients with thoracic and lumbar segmented fractures without nerve damage could better return to their daily livings when they underwent surgical treatment, and that 17 of patients under temporizing treatment exhibited abnormal findings and needed preventive fixation and synostosis more than temporizing treatments9). Major advantages of surgical internal fixation over temporary treatments that use postures and depend on relaxation are to make patients mobile, preventing nerve damage by overcoming the damaged spine and doing internal fixation early34,38); to protect damaged structures from external forces while increasing the possibility of restoration of neurological disorders and to replace the damaged structures' functions with appropriate internal fixation tools7). Frankel et al.15) reported that treatments using postures would be enough and that it would be possible to make patients mobile after restoring their stability by long-term relaxation. Jacobs et al.21) performed comparative studies between surgical methods and temporizing methods, and found that surgical methods were better than temporizing ones at overcoming fractures, restoring nervous functions, moving patients and decreasing complications.
Burst fractures typically involve violation of the inferior and/or superior endplates, and therefore the deformity may progress by gradual settling of the discs into the fractured endplates and vertebral body. Farcy et al.13) proposed that if the sagittal index exceeds 15 degrees, the biomechanical environment favors the progression of kyphosis33).
There was one case of loss of kyphotic correction in an elderly osteoporotic patient. Therefore, in osteoporotic patients, certain principles should be considered, such as multiple segment fixations, accepting lesser degrees of deformity correction, and avoiding the instrumentation length within the kyphotic segment19,24).
Individual patient characteristic may affect the occurrence of adjacent segment degeneration32). In particular, age at surgery was a potential risk factor for the radiologic degeneration of adjacent, especially older than 60 years of age. Age was likely related to the decreased ability of the aged spine to accommodate the biomechanical alterations imposed by a fusion20). Aota et al.3) observed that the incidence of adjacent segment degeneration was much higher in patients older than 55 years of age20).
CONCLUSION
This study showed meaningful radiological corrections in 19 surgically treated cases. Patients showed satisfactory synostosis and successful healing in virtual anatomic alignment without any complications. But, this study is limited by its short follow-up period and small study population. Patients' clinical outcomes seem to be comparable to any other fixation methods. When applied to cooperative patients willing to tolerate postoperative bracing, with assiduous assessment of the fracture's nature and using a method to evaluate the vertebral body's injury, short-segment pedicular instrumentation is considered a safe and effective technique.
References
- 1.Aebi M, Etter C, Kehl T. Stabilization of the lower thoracic and lumbar spine the internal spine skeletal fixation system. Indication, technique, and first results of treatment. Spine. 1987;12:544–551. doi: 10.1097/00007632-198707000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Ahmet A, Emre A, Muharrem Y, Ali O, Adil S. Short-Segment Pedicle Instrumentation of Thoracolumbar Burst Fractures Does Transpedicular Intracorporeal Grafting Prevent Early Failure? Spine. 2001;26:213–217. doi: 10.1097/00007632-200101150-00017. [DOI] [PubMed] [Google Scholar]
- 3.Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J spinal Disord. 1995;8:464–473. [PubMed] [Google Scholar]
- 4.Been HD, Bouma GJ. Comparison of two Types of Surgery for Thoraco-Lumbar Burst Fractures : Combined Anterior and Posterior Stabilization vs. Posterior Instrumentation Only. Acta Neurochir (Wien) 1999;141:349–357. doi: 10.1007/s007010050310. [DOI] [PubMed] [Google Scholar]
- 5.Blauth M, Tscherne M. Theraputic concept and results of operative treatment in acute trauma of the thoracic and lumbar spine : The Hanover experience. J Orthop Trauma. 1987;1:240–252. doi: 10.1097/00005131-198701030-00009. [DOI] [PubMed] [Google Scholar]
- 6.Boucher HH. A method of spinal fusion. J Bone Joint Surg Br. 1959;41B:248. doi: 10.1302/0301-620X.41B2.248. [DOI] [PubMed] [Google Scholar]
- 7.Bradford DS, Akbarnia BA, Winter RB. Surgical stabilization of fractures and fracture dislocation of the thoracic spine. Spine. 1977;2:185–196. [Google Scholar]
- 8.Cantor JB, Labwohl NH, Garvey T. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine. 1993;18:971–976. doi: 10.1097/00007632-199306150-00004. [DOI] [PubMed] [Google Scholar]
- 9.Chun SW, Hwang JH, Sung JK, Hwang SK, Hamm IS, Park YM, et al. Pedicle Screw Fixation and Posterolateral Fusion for Thoracolumbar Spine Fracture. J Korean Neurosurg Soc. 1999;28:644–648. [Google Scholar]
- 10.Denis F, Armstrong GWD, Searis K. Acute thoracolumbar burst fractures in the absence of neurologic deficits. Clin Orthop Relat Res. 1984;189:142–149. [PubMed] [Google Scholar]
- 11.Dickson JH, Harrington PR, Erwin WD. Results of reduction and stabilization of the severely fractured thoracic and lumbar spine. J Bone Joint Surg. 1978;60A:799–805. [PubMed] [Google Scholar]
- 12.Dorr LD, Harvey JP, Nickel VL. Clinical review of the early stability of spine injuries. Spine. 1882;7:545–553. doi: 10.1097/00007632-198211000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Farcy JP, Veidenbaum M, Glassman S. Sagittal index in management of thoracolumbar burst fractures. Spine. 1990;15:958–965. doi: 10.1097/00007632-199009000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Flesch JR, Leider LL, Erickson DL. Harrington instrumentation and spine fusion for unstable fractures and fracture dislocations of the thoracic and lumbar spine. J Bone Joint Surg. 1977;59:143–153. [PubMed] [Google Scholar]
- 15.Frankel H, Hancock DO, Hyslop G. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 16.Gertzbein SD, Court-Brown CM, Marks P. The neurologic outcome following surgery for spinal fractures. Spine. 1988;13:641–644. [PubMed] [Google Scholar]
- 17.Guttman L. Comprehensive management and research. Oxford: Blackwell scientific Publication; 1976. Spinal cord injuries; p. 152. [Google Scholar]
- 18.Han IH, Song GS. Thoracic Pedicle Screw Fixation and Fusion in Unstable Thoracic Spine Fractures. J Korean Neurosurg Soc. 2002;32:334–340. [Google Scholar]
- 19.Hu SS. Internal fixation in the osteoporotic spine. Spine. 1997;22:43s–48s. doi: 10.1097/00007632-199712151-00008. [DOI] [PubMed] [Google Scholar]
- 20.Hyun SJ, Lim YB, Hong HJ, Kwon JT, Suk JS, Min BK. Predictable risk factors for adjacent segment degeneration after lumbar fusion. J Korean Neurosurg Soc. 2007;41:88–94. [Google Scholar]
- 21.Jacobs RR, Casey MP. Surgical management of thoracolumbar spinal injuries. Clin Orthop Relat Res. 1984;189:22–35. [PubMed] [Google Scholar]
- 22.Jeffrey WP, Joel RL, Eldin EK, Robert WG. Successful Short-Segment Instrumentation and Fusion for Thoracolumbar Spine Fractures A Consecutive 4 1/2-Year Series. Spine. 2000;25:1157–1169. doi: 10.1097/00007632-200005010-00018. [DOI] [PubMed] [Google Scholar]
- 23.James JY, Allen S, Christopher S, Lawrence S, Kenneth W, Mark T, et al. The Treatment of Unstable Thoracic Spine Fractures with Transpedicular Screw Instrumentation : A 3-Year Consecutive Series. Spine. 2002;27:2782–2787. doi: 10.1097/00007632-200212150-00008. [DOI] [PubMed] [Google Scholar]
- 24.Kim KS, Oh SH, Huh JS, Noh JS, Chung BS. Dorsal Short-Segment Fixation for Unstable Thoracolumbar Junction Fractures. J Korean Neurosurg Soc. 2006;40:249–255. [Google Scholar]
- 25.King D. Internal fixation for lumbosacral fusion. Am J Surg. 1944;66:357–367. [PubMed] [Google Scholar]
- 26.Kothe R, Panjabi MM, Liu W. Multidirectional instability of the thoracic spine due to iatrogenic pedicle injuries during transpedicular fixation. A biomechanical investigation. Spine. 1997;22:1836–1842. doi: 10.1097/00007632-199708150-00008. [DOI] [PubMed] [Google Scholar]
- 27.Lee YS, Sung JK. Long-term Follow-up Results of Short-segment Posterior Screw Fixation for Thoracolumbar Burst Fractures. J Korean Neurosurg Soc. 2005;37:416–421. [Google Scholar]
- 28.McAfee OC, Yuan HA, Fredrickson BE, Lubicky JP. The value of computed tomography in thoracolumbar fractures. J Bone Joint Surg. 1983;65:461–473. [PubMed] [Google Scholar]
- 29.McCormack T, Karaikovic E, Gaines RW. The load-shearing classification of spine fractures. Spine. 1994;19:1741–1744. doi: 10.1097/00007632-199408000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Mumford J, Weinstein JN, Spratt KF. Thoracolumbar burst fractures : The clinical efficacy and outcome of nonoperative management. Spine. 1993;18:955–970. [PubMed] [Google Scholar]
- 31.Muller U, Berlemann U, Sledge J, Schwarzenbach O. Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation : bisegmental stabilization with monosegmental fusion. Eur Spine J. 1999;8:284–289. doi: 10.1007/s005860050175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar ot lumbosacral fusion. Spine. 2004;29:1938–1944. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 33.Patrick T, Russel CH, Christian AL, Dominique GP, Rene PL. Functional and radiologic outcome of thoracolumbar and burst fractures managed by closed orthopedic reduction and casting. Spine. 2003;28:2459–2465. doi: 10.1097/01.BRS.0000090834.36061.DD. [DOI] [PubMed] [Google Scholar]
- 34.Patrick WH, James CT, Souheil FH, Kenneth AF. Management options in thoracolumbar burst fractures. Surg Neurol. 1998;49:619–627. doi: 10.1016/s0090-3019(97)00527-2. [DOI] [PubMed] [Google Scholar]
- 35.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop. 1986;203:7–17. [PubMed] [Google Scholar]
- 36.Roy-Camille R, Saillant G, Salgado V. Osteogenesis of thoracolumbar spine fractures with metal plates screwed through the vertebral pedicle. Reconstr Surg Traumatol. 1976;15:2–16. [PubMed] [Google Scholar]
- 37.Sanderson PL, Fraser RD, Hall DJ, Cain CMJ, Osti OL, Potter GR. Short-segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999;8:495–500. doi: 10.1007/s005860050212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sasso RC, Costler HB. Posterior Instrumentation and fusion for unstable fractures and fracture-dislocations of the thoracic and lumbar spine. Spine. 1993;18:450–460. [PubMed] [Google Scholar]