Abstract
Tubular retractor system as a minimally invasive surgery (MIS) technique has many advantages over other conventional MIS techniques. It offers direct visualization of the operative field, anatomical familiarity to spine surgeons, and minimizing tissue trauma. With technical advancement, many spinal pathologies are being treated using this system. Namely, herniated discs, lumbar and cervical stenosis, synovial cysts, lumbar instability, trauma, and even some intraspinal tumors have all been treated through tubular retractor system. Flexible arm and easy change of the tube direction are particularly useful in contralateral spinal decompression from an ipsilateral approach. Careful attention to surgical technique through narrow space will ensure that complications are minimized and will provide improved outcomes. However, understanding detailed anatomies and keeping precise surgical orientation are essential for this technique. Authors present the technical feasibility and initial results of use a tubular retractor system as a minimally invasive technique for variaties of spinal disorders with a review of literature.
Keywords: Tubular retractor, Minimally invasive surgery, Spinal disorders, Microendoscopic discectomy
INTRODUCTION
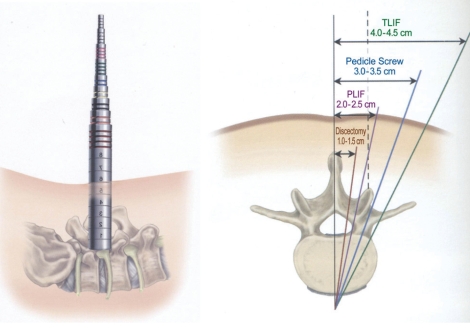
In 1997, the microendoscopic discectomy (MED) system was introduced, which allowed spine surgeons to reliably decompress a symptomatic lumbar nerve root via an endoscopic, minimally invasive surgical (MIS) approach5). METRx system (Medtronic Sofamor Danek, Memphis, TN) was the first commercially available product as a tubular retractor system (Fig. 1). Before this system was introduced, some speculum or polyethylene tube had been used as a kind of tubular dilator system9, 20). The best advantage of using this system is the application of endoscopic techniques to conventional surgery. This system enables both endoscopic images and direct surgical images to be viewed under a microscope. These can then be used according to the surgeon's purpose. Moreover, because METRx system splits the muscle instead of cutting it, it is possible to minimize postoperative back pain by reducing muscle damage.
Fig. 1.
METRx tubular retractor system.
Despite the benefits, there are some drawbacks to overcome before effective results can be achieved. First, appropriate surgical tools and manual skills are required since surgeons must work in a narrow space. Further, there may be confusion regarding anatomical structures in such a limited space. Another problem is the limitations of effective decompression. Surgeons must be aware that even though we completed the surgery effectively in a narrow space, symptoms can occur immediately if a small hematoma is generated in this space. Surgery under a microscope can provide direct surgical images like conventional surgeries, but the vision may be obstructed or disturbed by the use of tools in a narrow space with limited light. To solve these problems, the use of a high-performance microscope with excellent collimation capabilities and good lightening is recommended. Another solution is to attach a fiberoptic light source to one end of the tube for enhanced viewing, but this requires considerable additional costs because this device is expensive and its uses are limited. There is another problem not to be overlooked. The original purpose of being "less invasive" is impaired with overuse of a monopolar coagulator. Also, increased damage to the attached ligaments and muscles can occur when cleaning the operating field.
Lumbar discectomy
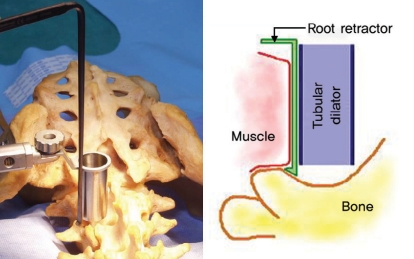
This was first used for hernination of the intervertebral disc, and even now is the method most often used. The space needed for laminectomy and discectomy for decompression is any about 15 to 20 mm. Therefore, most surgeries for herniation of the intervertebral disc can be carried out successfully with a 20-mm cylindrical tube. The narrower the tube's diameter and the longer the tube, the more difficult it is to use surgical tools and to obtain sufficient space. However, if too wide tube is used, the more potential there is to damage muscles around the spinal posterior arch. Thus, the original intent of minimally invasive surgery is impaired. In general, a tube with the diameter of 20 mm and a length of 40 to 50 mm is used. It is recommended to use a Steinman pin to first accurately check the location. However, this may possibly damage the spinal dura mater or spinal nerves, although rare. Therefore, the authors first make skin incision about 2 cm vertically near the midline and then cut the fascia also about 2 cm. After palpating the lamina while splitting the spinal muscles with index finger, progressively larger tubes are inserted starting with a small tube until the desired size is determined. We cannot achieve a good view even if we recklessly use a large tube because the lateral side of the lamina is inclined to the ventral and the facet joint is pushed backward. Using too large tube can excessively damage muscles because the muscles around the spine are pushed inside. Even after fixing the tube, the view may be blocked by the muscles pushed from the outside. If we damage the muscles too much to get the view, it may increase the possibility of postoperative backache. We may lengthen the outer side of the tube to prevent this, but its effect is doubtful. To avoid this, the authors turn the bending part of the root retractor on the outside of the tube to the outside and hook the spinal muscles to it so that the muscles will not be pushed inside. This is a very useful method (Fig. 2).
Fig. 2.
Root retractor can be effectively used for muscle retraction laterally.
After checking the correct positioning of the tube with a C-arm, the muscles around the spinal posterior arch and the ligamentum flavum are cleanly removed. Then the correct anatomical orientation of this part can be seen. For laminectomy, a high speed drill is used. To avoid damaging the spinal nerves, it is important to leave the inner cortical part of the caudal lamina and remove the remaining part with a small punch. Hence, using as large drill burrs as possible is effective and relatively safe. If drills cannot be used, Kerrison punches of various sizes can be used instead. The herniated nucleus pulposus is removed in the same way as in conventional surgery, and it is important to thoroughly control bleeding even if it is minimal. You must know the quantity and scope of the herniation of the nucleus pulposus before surgery to achieve sufficient decompression of the spinal nerves. In the case of far lateral disc herniation, you can effectively use discectomy and decompression to access both the midline and extraforaminal space through an incision in the skin20,27). When moving and positioning the tube to the extraforaminal space, it is important to understand the surrounding structures and thoroughly control bleeding because of the depth involved.
Decompression of the lumbar spine
This is a good indication for various lumbar stenosis. The foraminal stenosis is approached in the same way as for discectomy, and surgeons must be well aware of the structures of the intervertebral foramen. For central canal stenosis, both sides or one side can be accessed with, tilting the tube, and then effectively decompress the inside of the posterior arch at the opposite side using a drill, punch, chisel, curette. However, special care must be taken not to tear the dura mater because most patients with foraminal stenosis are old and the dura mater is thin. Absolute control of bleeding is crucial. Even minimal hematoma may cause serious nerve compression and may require reoperation because the operated part is narrow and deep. The most frequent causes of complications related to this surgery are incomplete decompression and dural tear.
Decompression and/or discectomy of the cervical spine
Posterior cervical foraminotomy has long been used to treat radicular pain arising from compression in the foramen, either bony stenosis or soft disc herniation24). Several authors presented microdiscectomy and decompresssion using muscle splitting minimally invasive tubular retractor system1,5,25). Hilton presented detailed surgical method of posterior cervical foraminotomy in 222 patients22). Prone position is utilized, with localization and docking of instrumentation accomplished with anterior/posterior fluorscopy. Surgery is performed with microscope-facilitated, three-dimensional visualization10).
This is a good indication for foraminal stenosis of the cervical spine. The approach is the same as for lumbar spine. It is effective to reduce the damage of the vertebral joint to approach from the ipsilateral and decompress the central canal stenosis, and to approach from the opposite side of the lesion to relieve the foraminal stenosis. After checking the accurate location of the tube, one should remove the medial part of the facet joint using a high speed drill, check the lateral of the ligamentum flavum and the up and down of the relevant nerves, and then perform decompression of the desired range10). If necessary, the herniated nucleus pulposus can be removed from the axilla or shoulder of the nerve root.
There are reports on successful surgeries for herniation of the intervertebral disc or cervical stenosis via anterior approach. When using this method, it is important to safely displace the esophagus and the carotid artery.
Transforaminal lumbar interbody fusion with instrumentation
The TLIF procedure was popularized by Harms as a method to achieve interbody lumbar fusion through a unilateral posterior approach7,8). The unilateral transforaminal interbody fusion (TLIF) allows approach to the disc space through usual paramedian approach or far-lateral approach without over retraction of the dura and preservation of the contrallateral anatomy. In spite of many advantages of TLIF, iatrogenic muscle injury can cause long-term problems that can negate the beneficial effects of the surgery itself. Schwender et al successfully performed the minimally invasive TLIF in 49 patients using the METRx tubular retractor system16). Results of this series was good but four complications were noted. Two were secondary to screw misplacement, and the remaining two were because of graft dislodgement and contralateral neural foraminal stenosis.
Tubular ratractor can be placed through paramedian muscle splitting method or between multipidus and longissimus (interfascial approach). In the case of medially placed tubular retractor, conventional laminectomy and facetectomy can be proceeded. To place an interbody device safely, enough laminectomy and facetectomy should be performed using chisels, Kerrison punches, and high speed drill. For more available space, X-tube or Quadrant retractor (Medtronic Sofamor Danek, Memphis, TN) can be used instead. Single or double cages are impacted into intervertebral space after careful complete removal of the nucleus pulposus. Autograph bone from laminectomy of iliac bone or other bone substitute are added to the interspace to augment fusion. Isaacs et al concluded this technique to be safe and exhibited a trend toward decreased intraoperative blood loss, postoperative pain, total narcotic use, and the risk of transfusion14). Pedicle screws can be easily inserted percutaneously via or interfascial route. Holly et al reported four complications from their 49 patients. Two reoperations were due to screw loosening. One ipsilateral and another contralateral postoperative radiculopathies were developed12).
Thoracic discectomy
To diminish potential complications and deficits associated with more traditional procedures for herniated thoracic discs, minimally invasive thoracic microendoscopic discectomy (TMED) was introduced15,22). The procedure is performed via a posterolateral approcach with the patient in the prone position. Main indications of this procedure are lateralized and central soft thoraic disc herniations causing radicular and myelopathic symptoms. The technique requires a transforaminal approach that minimizes muscle and bone dissection to reach thoracic disc lesions. After confirmation of the correct location. serial tubular retractor is inserted at the superior aspect of the caudal transverse process at the level of the herniated disc. A skin incision is made 3 to 4 cm lateral to the midline. The remaining approach is similar to that of a transforaminal procedure. The thoracic pedicle of the more caudal vertebral body is identified and followed to the appropriate disc level. Drilling of the superior cephalad aspect of the caudal pedicle facilitates access to the thoracic disc. After lateral disc herniations are removed under the direct vision, resection of a midline disc herniation require that a space in the disc be created and that a down-going currette or Woodson elevator then be used to push down the fragment into the disc space or removal. Bevelled endoscopic tube can be effectively used for confirmation of spinal cord decompression.
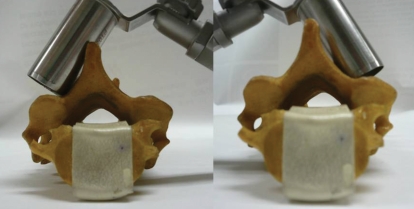
Instrumentation of the cervical spine
Lateral mass screw can be performed using tubular retractor system. Positioning the tubular retractors with the same trajectory as that of the lateral mass screws (i.e., angled superolaterally) allows the procedure to be performed in a fashion very similar to the open approach6,28). Bilateral screw insertion can be possible using midline single incision (Fig. 3). It has several advanteges. It reduces postoperative pain, but more importantly, it preserves the ligamentous attachments of the neck muscle to the laminae and spinous process. Several posterior muscle groups, in particular the semispinalis cervicis and multifidus muscle, function as dynamic stabilizers of the neck24). In the study by Fessler and Khoo, comparing their experience with open posterior cervical laminoforaminotomy, patients treated with microendoscopic foraminotomy (MEF) had a less painful recovery course4). But, this procedures has several limitations. Because of the small diameter of the tubular retractor, the working corridor is very narrow, and rod placement can be technically challenging. The Quadrant retractor system can be one solution for this problem. Bothersome venous bleeding may obscure narrow operative field but can be effectively controlled with powdered gelfoam mixed with thrombin.
Fig. 3.
Bilateral screws insertion can be possible through single midline incision.
Anterior screw fixation for odontoid fracture can be nicely performed using tubular retractor system13). Before the skin is incised, the flexible arm of the system is attached to the 18-mm tubular retractors, and the bed rail is mounted contralateral to the surgeon. Dissection down to the anterior aspect of the C5 vertebral body is undertaken in the usual fashion. Hand-held retractors are used until rostral dissection exposes the C2-3 disc space. The final dilator tip is then placed at the desired entry point, and the trajectory is confirmed using biplane fluoroscopy. The remaining steps are same as open traditional procedure.
Minimally invasive anterior approach to the upper cervical spine pathology was designed after cadaveric study using tubular dilator system6). They provide anatomic data for an anterior retropharyngeal upper cervical approach through a minimally invasive window below the hypoglossal and the superior laryngeal nerves. In two adult cadaveric cervical spines, the anterior approach using the METRx tubular retractors system through a window between the hypoglossal nerves and the superior laryngeal nerve, as well as below these two nerves, is compared in the exposure of C1 and C2 anteriorly with the aid of an operating microscope.
Various screw fixation methods are used to fuse the upper cervical vertebras, and one can effectively use tubes in this area as well. Particularly for the transarticular screwing of the first and second cervical vertebras, surgeons can effectively use a long tube to easily adjust the angle. The screw fixation and fusion of the first and second cervical vertebras can also effectively be achieved using a tube. There was a report on effective fixation of posterior C1 lateral mass and C2 pedicle screws for Os odontoideum patients17). They were alble to insert a C1 lateral mass screw and rod while positioning the tube and adjusting the angle around the C2 lateral mass. In this case, however, one must consider the fact that it may be difficult to control bleeding of the venous plexus between the first and second cervical vertebras.
There are many reports on operations using tubes for odontoid fracture9,13,23). Approaches vary by authors, but the most common procedure involve fixing the tubular retractor to the operating table and performing the surgery under fluoroscopic control while adjusting the angle as needed. In anterior transoral approach, an expandable tubular retractor can also effectively used without damaging surrounding tissues. Theoretically, posterior spinal fusion and decompression are possible for fracture with dislocation of the thoracic spine, but there are no reports on such surgeries yet. This could be due to the large area involved in such a surgery, the possibility of bleeding, and the difficulty of revision in such a narrow space.
Spinal tumors
Traditionally, an open surgical procedure consisting of laminectomy with intradural resection has been performed. These techniques have been used to achieve excellent outcomes as documented in a number of large series. However, with recent advances in minimal access technology, many spinal procedures are being performed with an emphasis on minimizing surrounding tissue damage and blood loss. Six consecutive intradural-extramedullary neoplasms were successfully removed using tubular retractor by Tredway et al26). All tumors were located intradural-extramedullary benign tumors. Extradural dumbell shaped schwannoma is nice indication for minimal invasive tubular retractors system operation.
Miscellaneous
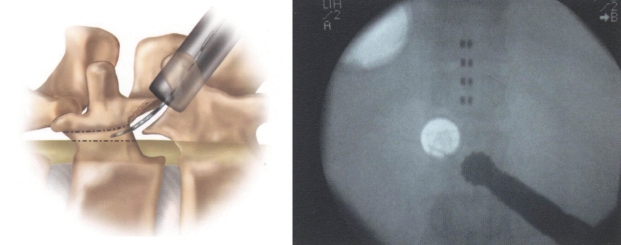
Since the early 1970s, pain relief through spinal cord stimulation has been a well-accepted treatment for selected patients with persistent neuropathic pain18,19). However, suboptimal electrode placement or recurrent dislocation can necessitate electrode revision. For functional improvement and stability, larger stimulating areas coverage is required. However, these larger plate electrodes, can presently only be inserted epidurally by means of a small open-surgical procedure involving partial laminectomy. Minimally invasive procedure like as tubular retractor system under the local anesthesia can be a good alternatives3,16). Tube placement was similar with other standard posterior cervical approach, by direction is more cephalad. To improve sight and illumination, the partial caudal hemilaminectomy and the removal of the ligamentum flavum using small Kerrisons are performed under microscopic guidance (Fig. 4). Beems et al reported successful result from their seven consecutive cases except one case after removal of dermoid using a tubular retractor system2).
Fig. 4.
Electrode lead implantation in the epidural space.
CONCLUSION
The tubular retractors system is safe and effective tools for various spinal operations in terms of minimal invasive technique. However, careful attention to surgical technique and precise anatomical knowledge are mandatory Spinal disorders including tumors can be approached with this technique, but it is limited to relatively short segment lesion. Further studies and advancement are needed in future before multiple or more extensive lesions can be treated through the tubular retractor system.
References
- 1.Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unulateral radiculopathy: results of a new technique in 100 cases. J Neurosurg. 2001;95(Suppl 1):51–57. doi: 10.3171/spi.2001.95.1.0051. [DOI] [PubMed] [Google Scholar]
- 2.Aldrich F. Posterolateral microdiscectomy for cervical monoradiculopathy caused by posterolateral soft cervical disc sequestration. J Neurosurg. 1990;72:370–377. doi: 10.3171/jns.1990.72.3.0370. [DOI] [PubMed] [Google Scholar]
- 3.Beems T, van Dongen RT. Use of a tubular ratractor as a minimally invasive technique fopr epidural plate electrode placement under local anesthesia for spinal cord stiulation: technical note. Neurosurgery. 2006;58(Suppl 1):ONS–E177. doi: 10.1227/01.NEU.0000193536.06577.D1. [DOI] [PubMed] [Google Scholar]
- 4.Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery. 2002;51(Suppl 2):S37–S45. [PubMed] [Google Scholar]
- 5.Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997;3:301–307. [Google Scholar]
- 6.Fong S, Duplessis S. Minimally invasive lateral mass plating in the treatment of posterior cervical trauma: surgical technique. J Spinal Disord Tech. 2005;18:224–228. [PubMed] [Google Scholar]
- 7.Hams JG, Jeszebszky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998;6:88–99. [Google Scholar]
- 8.Hams JG, Rollinger H. A one-stage procedure in operative treatment of spondylolisthesis: dorsal traction-reposition and anterior fusion. Z orthop Ihre Grenzeb. 1982;120:343–437. doi: 10.1055/s-2008-1051624. [DOI] [PubMed] [Google Scholar]
- 9.Hashizume H, Kawakami M, Kawai M, Tamaki T. A clinical case of endoscopically assisted anterior screw fixation for the type II odontoid fracture. Spine. 2003;28:E102–E105. doi: 10.1097/01.BRS.0000048659.96380.14. [DOI] [PubMed] [Google Scholar]
- 10.Hilton DL. Minimally invasive tubular access for posterior cervical forminotomy with three-dimensional microscopic visualization and localization with anterior/posterior imaging. Spine J. 2007;7:154–158. doi: 10.1016/j.spinee.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Hilton DL, Jr, Vardiman AB. Posterior cervical foraminotomy with three-dimensional visualization with minimally invasive tubular retractor (MITR); Oral presentation, AANS/CNS Section on Disorders of the Spine and Peripheral Nerves, 19th Annual Meeting Proceedings; Tampa. 2003. [Google Scholar]
- 12.Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion : indications, technique, and complications. Neurosurg Focus. 2006;15:E6. doi: 10.3171/foc.2006.20.3.7. [DOI] [PubMed] [Google Scholar]
- 13.Hott JS, Henn JS, Sonntag VK. A new table-fixed retractor for anterior odontoid screw fixation : technical note. J Neurosurg. 2003;98(Suppl 3):294–296. doi: 10.3171/spi.2003.98.3.0294. [DOI] [PubMed] [Google Scholar]
- 14.Issacs RE, Podichetty VK, Santiago P, Sandhu FA, Spears J, Kelly K, et al. Minimally invasive microendocopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3:98–105. doi: 10.3171/spi.2005.3.2.0098. [DOI] [PubMed] [Google Scholar]
- 15.Jho HD. Endoscopic transpedicular thoracic discectomy. Neurosurg Focus. 2000;15:E4. doi: 10.3171/foc.2000.9.4.5. [DOI] [PubMed] [Google Scholar]
- 16.Johnson MR, Tomes DJ, Treves JS, Leibrock LG. Minimally invasive implantation of epidural spinal cord neurostimulator electrodes by using a tubular retractor system : technical note. J Neurosurg. 2004;100:1119–1121. doi: 10.3171/jns.2004.100.6.1119. [DOI] [PubMed] [Google Scholar]
- 17.Joseffer SS, Post N, Cooper PR, FrempongBoadu AK. Minimally invasive atlantoaxial fixation with a polyaxial screw-rod construct : technical case report. Neurosurgery. 2006;58(Suppl 4):ONS–E375. doi: 10.1227/01.NEU.0000208955.12461.C7. [DOI] [PubMed] [Google Scholar]
- 18.Manola L, Holdheimer J. Technical performance of percutaneous and laminectomy leads analyzed by modelling. Neuromodulation. 2004;7:231–241. doi: 10.1111/j.1094-7159.2004.04207.x. [DOI] [PubMed] [Google Scholar]
- 19.Oakley JC. Spinal cord stimulation : patient selectioon, technique and outcomes. Neurosurg Clin N Am. 2003;14:365–380. doi: 10.1016/s1042-3680(03)00011-1. [DOI] [PubMed] [Google Scholar]
- 20.Obenchain TG. Speculum lumbar extraforaminal microdiscectomy. Spine J. 2001;1:415–420. doi: 10.1016/s1529-9430(01)00149-8. [DOI] [PubMed] [Google Scholar]
- 21.Palmer S, Turner R, Palmer p. Bilateral decompressive surgery in lumbar spinal stenosis associated with spondylolisthesis : unilateral approach and use of a microscopic and tubular retractor system. Neurosurg Focus. 2002;15:E4. doi: 10.3171/foc.2002.13.1.5. [DOI] [PubMed] [Google Scholar]
- 22.Perez-Cruet MJ, Kim BS, Sandhu F, Smartzis D, Fessler RG. Thoracic microendoscopic discectomy. J Neurosurg Spine. 2004;1:58–63. doi: 10.3171/spi.2004.1.1.0058. [DOI] [PubMed] [Google Scholar]
- 23.Shalyev SG, Mun IK, Mallek GS, Palmer S, Levi AD, Lasner TM, Kantrowitz AB. Retrospective analysis and modifications of retractor systems for anterior odontoid screw fixation. Neurosurg Focus. 2004;15:E14. doi: 10.3171/foc.2004.16.1.15. [DOI] [PubMed] [Google Scholar]
- 24.Shiraishi T. A new technique for exposure of the cervical spine laminae : Technical note. J Neurosurg. 2002;96(Suppl 1):122–126. doi: 10.3171/spi.2002.96.1.0122. [DOI] [PubMed] [Google Scholar]
- 25.Tomaras CR, Blacklock CB, Parker WD, Harper RL. Outpatient surgical treatment of cervical radiculopathy. J Neurosurg. 1997;87:41–43. doi: 10.3171/jns.1997.87.1.0041. [DOI] [PubMed] [Google Scholar]
- 26.Tredway TL, Santiago P, Hrubes MR, Song JK, Christie SD, Fessler RG. Minimally invasuice resection of intradural-extramedullary spinal neoplasms. Neurosuregry. 2006;59:E1152. doi: 10.1227/01.neu.0000192661.08192.1c. [DOI] [PubMed] [Google Scholar]
- 27.Vogelsang JP. The translaminar approch in combination with a tubular retractor system for the treatment of far cranio-laterally and foraminally extruded lumbar disc herniations. Zentralbl Neurochir. 2007;68:24–28. doi: 10.1055/s-2007-968165. [DOI] [PubMed] [Google Scholar]
- 28.Wang MY, Prusmack CJ, Green BA, Gruen JP, Levi AD. Minimally invasive lateral mass screws in the treatment of cervical facet dislocations : technical note. Neurosurgery. 2003;52:444–447. doi: 10.1227/01.neu.0000043814.57539.59. [DOI] [PubMed] [Google Scholar]