Abstract
Objective
The aim of the present study was to assess the safety and efficacy of the dynamic stabilization system in the treatment of degenerative spinal diseases.
Methods
The study population included 20 consecutive patients (13 females, 7 males) with a mean age of 61±6.98 years (range 46-70) who underwent decompression and dynamic stabilization with the Dynesys system between January 2005 and August 2006. The diagnoses included spinal stenosis with degenerative spondylolisthesis (9/20, 45%), degenerative spinal stenosis (5/20, 25%), adjacent segmental disease after fusion (3/20, 15%), spinal stenosis with degenerative scoliosis (2/20, 10%) and recurrent intervertebral lumbar disc herniation (1/20, 5%). All of the patients completed the visual analogue scale (VAS) and the Korean version of the Oswestry Disability Index (ODI). The following radiologic parameters were measured in all patients : global lordotic angles and segmental lordotic angles (stabilized segments, above and below adjacent segments). The range of motion (ROM) was then calculated.
Results
The mean follow-up period was 27.25±5.16 months (range 16-35 months), and 19 patients (95%) were available for follow-up. One patient had to have the implant removed. There were 30 stabilized segments in 19 patients. Monosegmental stabilization was performed in 9 patients (47.3%), 9 patients (47.3%) underwent two segmental stabilizations and one patient (5.3%) underwent three segmental stabilizations. The most frequently treated segment was L4-5 (15/30, 50%), followed by L3-4 (12/30, 40%) and L5-S1 (3/30, 10%). The VAS decreased from 8.55±1.21 to 2.20±1.70 (p<0.001), and the patients' mean score on the Korean version of the ODI improved from 79.58%±15.93% to 22.17%±17.24% (p<0.001). No statistically significant changes were seen on the ROM at the stabilized segments (p=0.502) and adjacent segments (above segments, p=0.453, below segments, p=0.062). There were no patients with implant failure.
Conclusion
The results of this study show that the Dynesys system could preserve the motion of stabilized segments and provide clinical improvement in patients with degenerative spinal stenosis with instability. Thus, dynamic stabilization systems with adequate decompression may be an alternative surgical option to conventional fusion in selected patients.
Keywords: Dynamic, Stabilization system, Degenerative spinal disorder, Lumbar vertebra
INTRODUCTION
Fusion is the conventional surgical treatment for degenerative spine disease proven unresponsive to nonoperative therapy6). With the recent developments in fusion techniques, successful radiographically confirmed fusion rates have exceeded 95%, but this has not been accompanied by an increase in successful clinical outcomes. Furthermore, fusion has been associated with several undesirable effects such as loss of motion, chronic lower back pain, and adjacent segmental degeneration5). Based on studies in which patients with partial fusion showed the same clinical outcomes as patients with solid fusion, it might be hypothesized that a reduction in, rather than an elimination of, segmental motion results in the alleviation of pain1,4,9,10). These findings suggest the need for alterative procedures and techniques that do not require fusion for the treatment of painful degenerative spine disease. Therefore, various kinds of dynamic stabilization systems have recently been developed. Of these, a pedicle-based dynamic stabilization system was designed to stabilize the segment while preserving motion and unloading the disc and facet joint16).
The Dynesys system was introduced as the first pedicle-based dynamic stabilization system in 1994. It is composed of titanium alloy (Protasul 100) pedicle screws, polyester (Sulene-PET) cords and polycarbonate-urethane (Sulene-PCU) spacers (Fig. 1). It is fixed in place by using standard pedicle screws made of a titanium alloy, and the entire system is stabilized by polyester cords that connect the screw heads through a hollow spacer and hold the screws in place12). To date, over 13,000 implantations have been performed worldwide for unstable segmental conditions, usually combined with spinal stenosis and degenerative discopathy.
Fig. 1.

Photograph of the Dynesys stabilization system on a spine model.
Several clinical studies have shown better outcomes with the Dynesys system than with conservative treatment alone2,12,16,17). Those results were comparable to those of conventional fusion; however, treatment failure, such as screw loosening, screw malposition or adjacent segmental degeneration, was reported in 17 to 19% of patients3,8). Thus, there has been some controversies on the use of the Dynesys system rather than fusion in the treatment of patients with degenerative spine disease. Furthermore, there are no reports concerning the application of this dynamic stabilization system in Korean patients, who have a slightly different lifestyle than western patients. In this study, the authors present the clinical and radiological outcomes of the application of the dynamic stabilization system for the treatment of patients with degenerative spine disease, with the primary objective of determining the safety and effectiveness of the system.
MATERIALS AND METHODS
Patient selection : inclusion criteria
The study population included 20 consecutive patients (13 females, 7 males), with a mean age of 61±6.98 years (range 46-70), who underwent decompression and dynamic stabilization with the Dynesys system performed by one surgeon between January 2005 and August 2006.
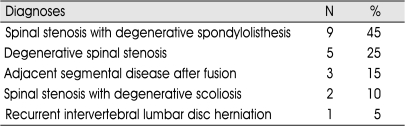
The diagnoses were spinal stenosis with degenerative spondylolisthesis (9/20, 45%), degenerative spinal stenosis (5/20, 25%), adjacent segmental disease after fusion (3/20, 15%), spinal stenosis with degenerative scoliosis (2/20, 10%) and recurrent intervertebral lumbar disc herniation (1/20, 5%) (Table 1).
Table 1.
Diagnoses of patients
All patients had neurogenic claudication, and 17 patients (85%) had additional low-back and buttock pain. The patients experienced symptoms for an average 74.8±105.73 months (range 8-360 months), and their symptoms were resistant to any conservative treatment. Ten patients (50%) had hypesthesia or parasthesia on the affected sensory dermatomes, and 5 patients (25%) had mild weakness in the affected lower extremities.
Four patients (20%) underwent a previous spinal operation : 3 patients underwent decompression and fusion, and 1 patient underwent discectomy. There were 5 patients with osteopenia who took Alendronate and CaCO3 for 6 months before the operation. There was no past medical history which affected the result of operation preoperatively.
Patients with osteoporosis (T-score at or below -2.5), malignancy, active local and/or systemic infection and degenerative scoliotic or kypotic deformities were excluded.
Preoperative evaluation
The preoperative evaluation included history taking, physical examination, neurological examination and imaging studies, including MRI, CT and DEXA (Dual-energy x-ray absorptiometry) bone densitometry. The patients completed the VAS and Korean version of the ODI. Anteroposterior and lateral standing dynamic (flexion and extension views) radiographs of the lumbar spine were taken in all patients before surgery and after surgery until the last follow-up. The global and segmental lordotic angles (stabilized segments, above and below adjacent segments) were measured by Cobb's method with the PACS program (M-view. Ver.5.4, Infinitt Technology). The global lordotic angles were measured from the upper endplate of T12 to the upper endplate of the sacrum. The segmental lordotic angles (stabilized segments and adjacent segments) were measured from between the upper end plates of the corresponding segments. After measuring the angles, the ROM in the stabilized segments and adjacent segments were calculated. The degree of spondylolisthesis was measured by slippage percentage based on the posterior vertebral margin of the lower vertebra.
Follow-up evaluation
The following data were collected : VAS, Korean version of the ODI, pain medication, complications and patient satisfaction. The plain radiographs (anteroposterior and lateral standing) and dynamic radiographs (flexion and extension views) were measured at the designated times until the last follow-up.
Surgical procedure
All operations were performed by one surgeon with the patient in a neutral position using standard surgical procedure for posterior lumbar spine surgery. In some cases, however, bilateral paraspinal (Wiltse) incisions were used in order to minimize muscle disruption. Central and foraminal decompression without any damage to facet joints were performed in all patients, not only at the stabilized segments, but also at the adjacent segments as needed. After adequate decompression, the titanium alloy pedicle screws were inserted, and their correct positions were controlled by anteroposterior and lateral fluoroscopy. Care was taken to place the screws lateral to the facet joints at 30°-45° lateromedial and parallel to the upper end plate of the corresponding segment. The polycarbonate urethane spacers were cut to the appropriate size by measuring the distance between the two pedicle screws and then installed along with the polyester cord. The system was tightened with the specified preload. No further distractive or compressive force was applied to the segment, and no attempt was made to reduce spondylolisthesis.
RESULTS
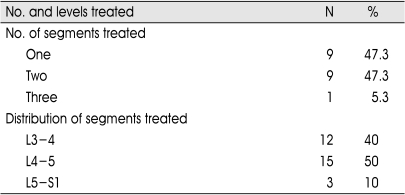
The mean follow-up duration was 27.25±5.16 months (range 14-33 months), and 19 patients (95%) were available for follow-up. One patient had to have the implant removed (described later). There were 30 stabilized segments in 19 patients. Monosegmental stabilization was performed in 9 patients (47.3%), two segmental stabilizations were performed in 9 patients (47.3%) and three segmental stabilizations were performed in 1 patient (5.3%). The most frequently treated segment was L4-5 (15/30, 50%), followed by L3-4 (12/30, 40%) and L5-S1 (3/30, 10%) (Table 2).
Table 2.
Instrumented segments
The mean operating time was 180±46.18 minutes (range 110-290), and the mean blood loss was 125±39.31 cc (range 100-200). The mean hospital stay was 8.75±4.55 days (range 5-21).
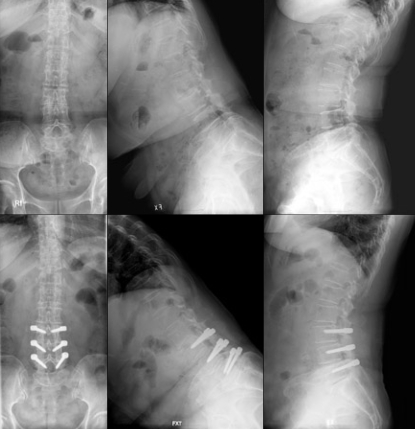
Fig. 2 shows the pre- and postoper-ative radiographs showing the typical pathologies for which the Dynesys was applied.
Fig. 2.
A case of 61 years old female patient with spinal stenosis at L3-4 and L4-5. Preoperative (upper row) and postoperative (lower row) anteroposterior, flexion and extension view. Postoperative dynamic lateral radiographs show preservation of segmental motion at stabilized segments.
Complications
There were 6 patients with dural tear during decompressive procedure, which were found and repaired intraoperatively. There was no cerebrospinal fluid leakage postoperatively. Three of 20 patients required reoperation during the follow-up period. The implant in one patient needed to be removed due to a delayed allergic reaction 10 months after the operation. There was no elevation of serum ESR and CRP before the operation. Intraoperatively, although there was a white discharge around the PCU spacer, there was no bacterial growth in an aspirated fluid culture. Two patients needed additional surgery. One patient with the Dynesys implantation at L3-4 and L4-5 had persistent back pain and radiating pain in the left L4 dermatome at 3 months postoperative. The symptom was improved by an additional total laminectomy of L3-4. The other patient with the Dynesys implantation at L4-5 had unsolved persisting pain due to foraminal stenosis at the lower level. Therefore, foraminal decompression and interbody fusion (L5-S1) was added to increase the height of the foramen.
One patient developed dysarthria and facial palsy at 8 days postoperative and was diagnosed with an acute infarction of the left corona radiata of the cerebrum.
There were no implant failures, such as pedicle fracture, screw loosening or screw malposition, as of the last follow-up.
Clinical outcome
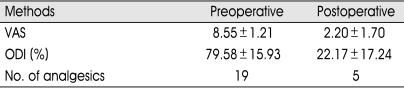
The VAS for back and leg pain decreased from a preoperative mean value of 8.55±1.21 (range 6-10) to a postoperative mean value of 2.20±1.70 (range 0-5) (p<0.001) (Table 3). The number of patients using pain medication decreased from 19 patients (100%) preoperatively to 5 patients (26.3%) postoperatively. After the operation, 14 patients (78.7%) did not use analgesics and 11 patients (57.8%) were completely free of back and leg pain. There were no newly developed neurologic deficits or aggravation of neurological symptoms. Five patients continued to experience hypesthesia, and 1 patient showed no improvement in lower extremity weakness.
Table 3.
Clinical outcome
The preoperative Korean version of the ODI was 79.58%±15.93% (range 22-89%), indicating that the average patient had a severe disability. At follow-up, it was 22.17%±17.24% (range 2-57%), which corresponds to moderate disability. This improvement was also statistically significant (p<0.001). At the last follow-up, 17 patients (89.5%) were satisfied with the result of surgery, but 2 patients (10.5%) were not.
Radiologic follow-up
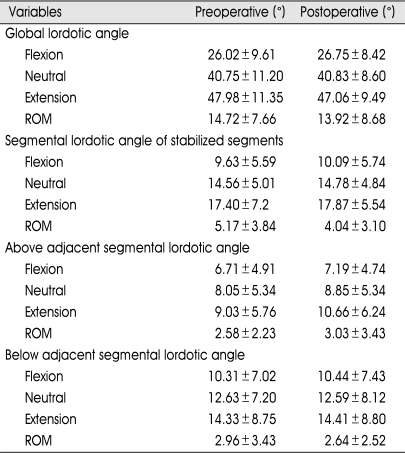
The global lordotic angles and segmental lordotic angles (stabilized segments, above and below adjacent segments) were measured by lateral standing radiographs, including flexion and extension views, of patients standing in a neutral position (Table 4).
Table 4.
Radiological outcome
Rom : Range ot motion
The ROM of the global levels was 14.72°±7.66° before the operation and 13.92°±8.68° at the last follow-up. This change was not statistically significant (p=0.002). The ROM in the stabilized segments was 5.17°±3.84° preoperatively and 4.04°±3.10° postoperatively (p=0.502). The ROM in the upper segments was 2.58°±2.23° preoperatively and 3.03°±3.43° postoperatively (p=0.453). The ROM in the lower segments was 2.96°±3.43° preoperatively and 2.64°±2.52° postoperatively (p=0.062). There was no statistically significant change in the ROM.
There were 9 patients with a degenerative spondylolisthesis, all grade I. The change of slippage was from 16.29% (range 9-20) to 14.62% (range 9-17.75).
DISCUSSION
Various forms of degenerative lumbar spine disease require surgical stabilization. As an alternative to fusion, dynamic stabilization systems have various advantages, such as allowing for greater physiologic function and reducing the inherent disadvantages of rigid instrumentation and fusion. The dynamic stabilization system appears to stabilize the spinal segments without fusion across the intervertebral disc or the facet joints. These stabilized segments seem to retain some mobility, which may help to reduce pain and prevent further degeneration of adjacent segments. Dynesys implantation with preservation of the disc and facet may create a favorable environment in the motion segment by unloading these joints and allowing more normal motion. The resumption of mobility in the moderately degenerated disc and facet joint may also slow the degenerative spinal process11,14).
Several clinical studies of the Dynesys system have been published. Previous studies of patients who had similar indications for surgery as the patients in the present study showed significant reduction in pain and disability scores2,12,16,17). The authors suggest that the Dynesys system could be an alternative to conventional fusion. However, Grob et al. reported less satisfactory clinical outcomes, which may have been related to a lack of surgical decompression in some of the patients8). In addition, Cakir et al. concluded that the small sample size and consequent lack of any statistical analyses make it difficult to prove that the Dynesys system is safe and efficient in the treatment of degenerative spine disease3).
The clinical outcomes of the present study improved significantly during the follow-up period. The VAS decreased from 8.55±1.21 to 2.20±1.70. The mean Korean version of the ODI score improved from 79.58%±15.93% to 22.17%±17.24%. There were 11 patients (57.8%) who were completely free of back and leg pain. Seventeen patients (89.5%) were satisfied with the results of the treatment as of the last follow-up.
The ROM in the global and segmental (stabilized segments, above and below adjacent segments) segments showed no statistically significant changes. The dynamic stabilization system seems to not only preserve segmental motion, but also maintain the patient's own lumbar kinematics. Although it is hard to conclude whether the dynamic stabilization system can prevent adjacent segmental degeneration or not at this time, but this preservation of ROM may prevent the acceleration of adjacent segmental degeneration. There was no definite progression of spondylolisthesis or kyphosis, and radiological evaluation revealed that there was no loosening or breakage of screws.
The dynamic stabilization system has been in clinical use for more than 10 years in Europe. However, there were no reports on the use of the Dynesys system in Korea to date. Despite the different lifestyle in Korea, our clinical and radiological outcomes favorably agree with the published data on dynamic stabilization systems.
The preoperative data did not provide any clue as to the limitations of using the Dynesys, and age, gender, duration of symptoms, and comorbidities did not influence the patient outcome12). However, it can be assumed that patients with severe osteoporosis are not suitable for the use of the Dynesys because the anchorage of pedicle screws to the bone is crucial for the pedicular system, and it places a great demand on spinal implants10). Though some investigators have mentioned complications related to implantation, such as a pedicle fracture, screw loosening, sign of screw loosening on radiograph and screw malposition, there has been no implant failure as of the last follow-up in the present study. DEXA bone densitometries were performed as a preoperative assessment in all patients. Therefore, patients with osteoporosis (T-score at or below -2.5SD) were excluded from the Dynesys implantation. If necessary, these patients were treated for osteoporosis before the operation.
The clinical and radiological outcome of dynamic stabilization system with the Dynesys is comparable to that reported in the literature regarding fusion in that it allows for stabilization with the preservation of dynamic nature of the spine and improves the clinical outcome.
CONCLUSION
This study revealed that the dynamic stabilization system could preserve segmental motion with stability and clinical improvement. Thus, it is considered safe and effective to apply the dynamic stabilization system instead of conventional fusion after adequate decompression in selected patients with degenerative spinal stenosis with instability. The long-term effects and kinematic changes associated with dynamic stabilization need to be evaluated in further studies.
References
- 1.Bastian L, Lange U, Knop C, Tusch G, Blauth M. Evaluation of the mobility of adjacent segments after posterior thoracolumbar fixation : a biomechanical study. Eur Spine J. 2001;10:295–300. doi: 10.1007/s005860100278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bordes-Monmeneu M, Bordes-Garcia V, Rodrigo-Baeza F, Saez D. [System of dynamic neutralization in the lumbar spine : experience on 94 cases.] Neurocirugia (Astur) 2005;16:499–506. [PubMed] [Google Scholar]
- 3.Cakir B, Ulmar B, Koepp H, Huch K, Puhl W, Richter M. [Posterior dynamic stabilization as an alternative for dorso-ventral fusion in spinal stenosis with degenerative instability] Z Orthop Ihre Grenzgeb. 2003;141:418–424. doi: 10.1055/s-2003-41568. [DOI] [PubMed] [Google Scholar]
- 4.Chou WY, Hsu CJ, Chang WN, Wong CY. Adjacent segment degeneration after lumbar spinal posterolateral fusion with instrumentation in elderly patients. Arch Orthop Trauma Surg. 2002;122:39–43. doi: 10.1007/s004020100314. [DOI] [PubMed] [Google Scholar]
- 5.Fritzell P, Hagg O, Nordwall A. Complications in lumbar fusion surgery for chronic low back pain : comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J. 2003;12:178–189. doi: 10.1007/s00586-002-0493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion : a comparison of three surgical techniques : a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine. 2002;27:1131–1141. doi: 10.1097/00007632-200206010-00002. [DOI] [PubMed] [Google Scholar]
- 7.Garner MD, Wolfe SJ, Kuslich SD. Development and preclinical testing of a new tension-band device for the spine : the Loop system. Eur Spine J. 2002;11(Suppl 2):S186–S191. doi: 10.1007/s00586-002-0463-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine : surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine. 2005;30:324–331. doi: 10.1097/01.brs.0000152584.46266.25. [DOI] [PubMed] [Google Scholar]
- 9.Guigui P, Wodecki P, Bizot P, Lambert P, Chaumeil G, Deburge A. [Long-term influence of associated arthrodesis on adjacent segments in the treatment of lumbar stenosis: a series of 127 cases with 9-year follow-up] Rev Chir Orthop Reparatrice Appar Mot. 2000;86:546–557. [PubMed] [Google Scholar]
- 10.Lehmann TR, Spratt KF, Tozzi JE, Weinstein JN, Reinarz SJ, el-Khoury GY, et al. Long-term follow-up of lower lumbar fusion patients. Spine. 1987;12:97–104. doi: 10.1097/00007632-198703000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Putzier M, Schneider SV, Funk JF, Tohtz SW, Perka C. The surgical treatment of the lumbar disc prolapse : nucleotomy with additional transpedicular dynamic stabilization versus nucleotomy alone. Spine. 2005;30:E109–E114. doi: 10.1097/01.brs.0000154630.79887.ef. [DOI] [PubMed] [Google Scholar]
- 12.Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine. 2006;31:442–449. doi: 10.1097/01.brs.0000200092.49001.6e. [DOI] [PubMed] [Google Scholar]
- 13.Schwarzenbach O, Berlemann U, Stoll TM, Dubois G. Posterior dynamic stabilization systems : DYNESYS. Orthop Clin North Am. 2005;36:363–372. doi: 10.1016/j.ocl.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Sengupta DK. Point of view : Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine. 2006;31:450. doi: 10.1097/01.brs.0000200051.24623.33. [DOI] [PubMed] [Google Scholar]
- 15.Sengupta DK, Mulholland RC. Fulcrum assisted soft stabilization system: a new concept in the surgical treatment of degenerative low back pain. Spine. 2005;30:1019–1029. doi: 10.1097/01.brs.0000160986.39171.4d. discussion 1030. [DOI] [PubMed] [Google Scholar]
- 16.Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine : a multi-center study of a novel non-fusion system. Eur Spine J. 2002;11(Suppl 2):S170–S178. doi: 10.1007/s00586-002-0438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Welch WC, Cheng BC, Awad TE, Davis R, Maxwell JH, Delamarter R, et al. Clinical outcomes of the Dynesys dynamic neutralization system : 1-year preliminary results. Neurosurg Focus. 2007;22:E8. doi: 10.3171/foc.2007.22.1.8. [DOI] [PubMed] [Google Scholar]