Abstract
The crossing laminar screw fixation might be the most recently developed approach among various fixation techniques for C2. The new construct has stability comparable to transarticular or transpedicular screw fixation without risk of vertebral artery injury. Quantitative anatomical studies about C2 vertebra suggest significant variation in the thickness of C2 lamina as well as cross sectional area of junction of lamina and spinous process. We present an elderly patient who underwent an occipito-cervical stabilization incorporating crossed C2 laminar screw fixation. We preoperatively recognized that she had low profiles of C2 lamina, and thus made a modification of trajectory for the inferiorly crossing screw. We introduce a simple modification of crossing C2 laminar screw technique to improve stability in patients with low laminar profiles.
Keywords: Laminar screw, Occipitocervical fixation
INTRODUCTION
The axial laminar fixation using screws based on Brooks's idea of neural arch stabilization is straightforward, however overcome high nonunion rate in wiring methods1,9). Stability of the technique is comparable to transarticular screw or pedicle screw and intraosseous placement of laminar screw is not related with vertebral artery injury3,5,8,11). About 18-23% of C2 pars/pedicle do not have sufficient size to accept 3.5 mm-diametered screw6,7). In such patients, the technique comes to a reliable alternative for C2 fixation. Quantitative studies on anatomical parameters of C2 have demonstrated significant variations on the laminas as well as pars/pedicle10,13). In our opinion, asian women with low profiles of C2 laminas should be carefully assessed preoperatively about cross sectional area of junction of lamina and spinous process if each of two laminar screws can cross out of contact. To determine if cross sectional area of the junction accommodates two crossing screws with at least 1 mm tolerance on each is as important as to determine the thickness of lamina.
We present a patient with complex injuries at craniovertebral junction, who had low profiles of C2 lamina. We preoperatively assessed anatomical parameters of C2 lamina and thought that modification of trajectory of laminar screw was required to have two crossing screws keeping bony tolerance on each other. Here, we introduce a modified laminar screw fixation, double bicortical purchase of the inferiorly crossing laminar screw, and suggest that the height of crossing plan of two laminar screws is a practical parameter for the crossing C2 laminar screw fixation.
CASE REPORT
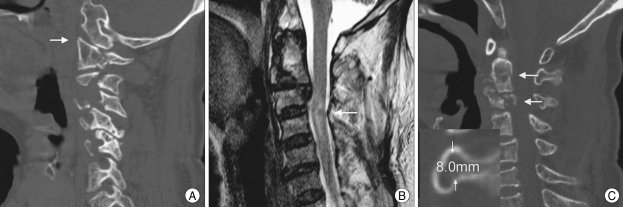
This 81-year-old female was brought to emergency room (ER) with upper cervical injuries. Cervical computed tomography (CT) obtained at ER demonstrated bilateral lateral mass fractures of C1. Particularly on the left side, the fracture of lateral mass was communited and extended to the transverse process causing fracture/subluxation of the left atlanto-occipital joint (Fig. 1A). She also had type III odontoid process fracture and fractures of C3 body and lamina causing subluxation at the C3/C4 (Fig. 1C). The Cervical magnetic resonance image (MRI) showed signal change on T2 weighted images at C2-C4 with mild compression of the spinal cord by displaced C2-C3 segments (Fig. 1B). Neurological examination demonstrated complete paralysis of the left extremities and grade II weakness on the right side. The anal tone and perineal sensation were impaired.
Fig. 1.
Preoperative radiologic findings. A: The fracture of the left lateral mass on initial computed tomography is communited and causes fracture/subluxation of the left atlanto-occipital joint(arrow). B: The cervical magnetic resonance image showing signal change on T2 weighted image at C2-C4 level with mild compression of the spinal cord by displaced C2-C3 segments (arrow). C : The Type 3 odontoid process fracture with communition and fractures of C3 body and lamina causing subluxation at the C3/C4 (arrows). The junctional height of bilateral laminae and spinous process is 8.0 mm.
We carefully assessed C2 anatomical parameters and planned occipito-cervical stabilization incorporating crossed C2 laminar screw fixation because of the left narrow pedicle. Then, there was an issue of small cross sectional area at the junction of bilateral laminas and spinous process where two screws would cross each other (Fig. 1C). The thickest part of lamina is mid-level, so the screw should be placed in the mid-level of the lamina. We recognized that purchase of screws in parallel with opposite screw at the crossing plan would minimize the risk of unexpected screw contact so that screws would have bony tolerance on each other.
Operation
The patient was positioned prone and had the Mayfield tongs placed. The posterior occipito-cervical region was then shaved and draped in a sterile fashion. The incision was carried down from the external occipital protuberance to the C7 level and care was taken to perform a subperiosteal dissection. There was a fracture of C3 lamina noticed on preoperative CT scanning. The posterior elements were fully exposed.
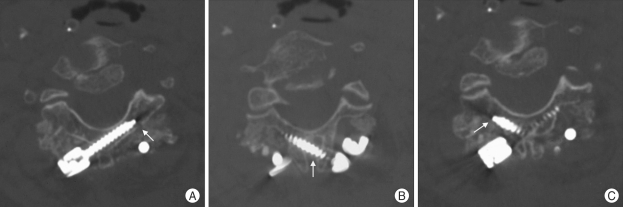
A laminectomy was performed at C3. After decompression of the level of noted signal change on preoperative MRI, the lateral masses were marked. The 14 mm lateral mass screws (Vertex, Medtronic Sofamor Danek, TN, USA) were placed in the lateral masses of C4 and C5 using a hand drill and hand tap under fluoroscopic guidance. Then, 4×6 mm screws and 4.5×8 mm screws were placed using a burr drill and hand tap to fix the occipital plate. Next, our attention was turned towards C2 posterior elements for laminar screw fixation. For the superiorly crossing laminar screw, a high-speed drill was used to open a small entry window at the left side of the C2 spinous base and a small exit window at the junction of the right facet and lamina (Fig. 2A). The exit window gave us confirmation that the pedicle finder or screw did not violate the inner cortex of the lamina, allowed us to obtain bicortical screw purchase, and enabled us to measure the appropriate screw length. We could place 3.5×24 mm screw with one or two threads of screw tip into the exit window, giving bicortical purchase (Fig. 2A). For the inferiorly crossing second laminar screw, the right side of wide and bifid inferior base of C2 spinous process was pierced for double bicortical trajectory. A small exit window was opened again at the junction of the left facet and lamina. A 3.5 mm tapper was advanced through two windows of spinous process to the exit window. We confirmed intact inner cortical lamina using a round-tip probe and bony tolerance to the superiorly crossing screw (Fig. 2C). The second 3.5×24 mm screw was inserted through two whole of bifid base of spinous process to the lamina (Fig. 2B). The screw tips were placed at exit windows (Fig. 3A, C).
Fig. 2.
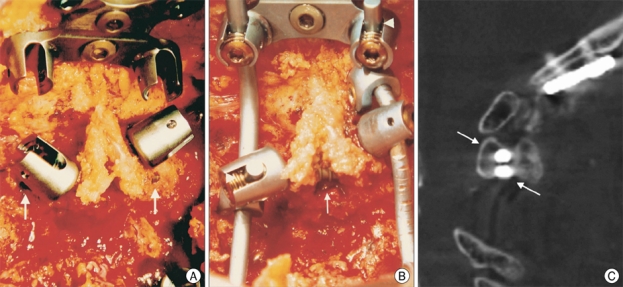
A: Intraoperative photograph shows two exit windows to identify correctly placed tip of the screw (arrows). B : Intraoperative photograph shows double bicortical purchase of the inferiorly crossing screw through the bifid spinous process (arrow). Rods assembled with C2 laminar screws using lateral connectors without difficulty (arrow heads). C : Postoperative computed tomography shows excellent intraosseous locations of two screws with intact bony barrier in spite of close proximity at the crossing plan. Arrows indicate parallel direction of the screws.
Fig. 3.
Postoperative computed tomography. A: Superiorly crossing laminar screw is intraosseously placed and identified through exit cortical window (arrow). B, C: Inferiorly crossing laminar screw shows double purchase of bifid spinous process (arrows).
Fluoroscopic images neither guided screw trajectory nor confirmed screw placement in relation to the spinal canal unlike in C2 pedicle screw purchase. All screw holes were checked for breeches prior to placement of the screw. There were no inner cortical breeches and the screws were placed accordingly.
The head of lamina screw was positioned at the side of spinous process facing lateral and the lateral connector was engaged on the head. Rods were applied in their orientation. The postoperative CT scan demonstrated excellent locations (Fig. 3).
DISCUSSION
C2 pars/pedicle screws have been widely applied for C2 stabilization. However, transpedicular approach has a risk of vertebral artery injury of 2% per screw and 18-23% incidence of pars/pedicle that can not accommodate screw purchase6,7,12). In such cases, crossing laminar screw fixation provides excellent mechanical strength comparable to C1-C2 transarticular or pedicle screw fixation8).
Accurate laminar screw placement depends on preoperative assessment on radiographic appearance of C2 neural arch. Axial sections of computed tomography scan are necessary to define the orientation and thickness of the laminas because C2 arches do not always accommodate 3.5 mm-diametered laminar screw bilaterally. Thickness of the thickest part of lamina was 3.80-6.78 mm in western women2,13). According to a cadaveric study on cross sectional area, up to 37% of specimens would be unable to accommodate a 3.5 mm screw in at least one of the laminas10). Result of these studies and our preliminary investigation with CT scans (data not shown), we speculate that the height of junction of lamina and spinous process is a practical indicator to determine whether patient's lamina can accommodate two screws crossing out of contact with each other.
According to available data an American people by Xu and colleagues13), the average height of C2 lamina of western women is 10.9±1.0 mm. Profiles of mean thickness were 3.0±1.1 mm at 2 mm below the superior margin of C2 laminas, 5.0±1.2 mm for the middle of C2 lamias and 4.8±1.2 mm at 2 mm above the inferior laminar margin. Assuming oriental women' profiles of C2 are not greater than western women, 3.5 mm-diametered threaded screw should be placed towards the middle of lamina in vertical dimension.
In our patient, thickness of the thickest part of lamina seemed sufficient for a 3.5 mm-diametered screw. However, the height of crossing plan was only 8 mm. We felt that there would be only 1 mm tolerance between two screws even if we perfectly place the screws. For this reason, we made interrupted two windows at the bifid base of the spinous process for the inferior screw.
In general, insertion of the screw to the maximum possible length is recommended. Double bicortical purchase of the inferiorly crossing laminar screw is expected to improve stability by increasing insertion length of the inferiorly crossing screw and preserving maximum tolerance between two crossing screws. We intraoperatively confirmed solid stabilization.
The approach also has drawbacks including spinal cord injury by the screw disrupting the inner cortex of lamina. By Wang's10) investigation, the laminar morphology was found to be quite variable and too small to accommodate the 3.5 mm screws, assuming 1 mm tolerance on each side, in 16 sides of the 14 cadaveric specimens. This is one reason that inner cortical disruption of C2 lamina causing spinal cord injury occurs during the approach. In such cases, cortical exit window would be useful to identify correct screw placement4).
The crossed C2 laminar fixation has been utilized as a subaxial fixation point for occipito-cervical fixation, an upper cervical fixation site for subaxial cervical fusions, or an adjunct to long occipito-cervical constructs. It has been reported that there is difficulty in connecting the rod to the C2 screw because of the medial location of the entry point and the steepness of the screw trajectory while constructing occipitocervical fixation4). However, we can be applied a rod on the laminar screw head using a lateral connector without difficulty.
CONCLUSION
Double bicortical purchase of bifid base of C2 spinous process is expected to improve safety and stability of crossing C2 laminar screws in patients with low laminar profiles. Precise preoperative assessment not only on the thickness of the lamina but also on the height of crossing plan of two screws is important. Approach oriented anatomical study for Korean is strongly recommend.
References
- 1.Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60:279–284. [PubMed] [Google Scholar]
- 2.Cassinelli EH, Lee M, Skalak Anthony, Ahn NU, Wright NM. Anatomic considerations for the placement of C2 laminar screws. Spine. 2006;31:2767–2771. doi: 10.1097/01.brs.0000245869.85276.f4. [DOI] [PubMed] [Google Scholar]
- 3.Hong JT, Lee SW, Son BC, Park CK. Posterior C1-2 stabilization using translaminar screw fixation of the axis. J Korean Neurosurg Soc. 2006;40:387–390. [Google Scholar]
- 4.Jea A, Sheth RN, Vanni S, Green BA, Levi AD. Modification of Wright's technique for placement of bilateral crossing C2 translaminar screws : technical note. Spine J. 2007 doi: 10.1016/j.spinee.2007.06.008. in press. [DOI] [PubMed] [Google Scholar]
- 5.Kim SY, Jang JS, Lee SH. Posterior atlantoaxial fixation with a combination of pedicle screws and a laminar screw in the axis for a unilateral high-riding vertebral artery. J Korean Neurosurg Soc. 2007;41:141–144. [Google Scholar]
- 6.Madawi A, Casey A, Solanki G, Tuite G, Veres R, Crockard H. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997;86:961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 7.Paramore C, Dickman C, Sonntag VKH. The anatomical suitability of the C1-2 complex for transarticular screw fixation. J Neurosurg. 1996;85:221–224. doi: 10.3171/jns.1996.85.2.0221. [DOI] [PubMed] [Google Scholar]
- 8.Reddy C, Ingalhalikar AV, Channon S, Lim TH, Torner J, Hitchon PW. In vitro biomechanical comparison of transpedicular versus translaminar C-2 screw fixation in C2-3 instrumentation. J Neurosurg Spine. 2007;7:414–418. doi: 10.3171/SPI-07/10/414. [DOI] [PubMed] [Google Scholar]
- 9.Reilly TM, Sasso RC, Hall PV. Atlantoaxial stabilization : clinical comparison of posterior cervical wiring technique with transarticular screw fixation. J Spinal Disord Tech. 2003;16:248–253. doi: 10.1097/00024720-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Wang MY. C2 crossing laminar screws : cadaveric morphometric analysis. Neurosurgery. 2006;59(1) Suppl 1:ONS84–ONS88. doi: 10.1227/01.NEU.0000219900.24467.32. [DOI] [PubMed] [Google Scholar]
- 11.Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws : case series and technical note. J Spinal Disorder Tech. 2004;17:158–162. doi: 10.1097/00024720-200404000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation : results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American association of neurological surgeons/congress of neurological surgeons. J Neurosurg. 1998;88:634–640. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]
- 13.Xu R, Burgar A, Ebraheim N, Yeasting R. The quantitative anatomy of the laminas of the spine. Spine. 1999;24:107–113. doi: 10.1097/00007632-199901150-00002. [DOI] [PubMed] [Google Scholar]