Abstract
A cerebrospinal fluid hydrothorax is a very rare complication following ventriculoperitoneal (VP) shunt and usually reported in children. We report a case of 47-year-old woman who developed massive hydrothorax and respiratory distress following intrathoracic migration of distal shunt catheter. After the confirmation of catheter in thoracic cavity using radionuclide shuntogram, the patient was successfully treated with laparoscopic shunt catheter reposition.
Keywords: Hydrothorax, Ventriculoperitoneal shunt, Hydrocephalus
INTRODUCTION
The most of complications after ventriculoperitoneal (VP) shunt are shunt infection and malfunction2,6,8). The intrathoracic complications of the VP shunt are rare but can be life threatening. Diagnosis of this case, migration of shunt catheter, was confirmed by the presence of intrathoracic catheter using shuntogram. It was repositioned using laparascopy. The authors report a case of hydrothorax after VP shunt with rewiew of pertinent literature on the mode of thoracic migration of shunt catheter.
CASE REPORT
A 47-year-old woman visited our emergency room due to mild fever, dyspnea and chest pain. One month prior to admission, the patient underwent VP shunt for the treatment of communicating hydrocephalus after spontaneous subarachnoid hemorrhage caused by the ruptured basilar bifurcation aneurysm. On physical examination, diminished breath sounds were observed on the left lower chest field. Other findings were unremarkable including good-reboundness of shunt reservoir. No ventriculomegaly was observed on brain CT scan. On chest radiograph, pleural effusion on left lower lung field was noted, and the distal shunt catheter was located at the left costophrenic angle (Fig. 1A). At first, we had considered patient's condition as pneumonia or shunt infection. Cerebrospinal fluid analysis was unremarkable. Thus, we started empirical antibiotic therapy for the treatment of pulmonary infection. After 5 days, the patient complained of worsening of dyspnea and left pleural effusion was aggrevated on chest x-ray. It was then speculated that the shunt distal catheter had migrated into left thoracic cavity (Fig. 1B). After shuntogram, we confirmed that distal shunt catheter tip was located not within the abdominal cavity but in the intrathoracic cavity (Fig. 2). The distal shunt catheter reposition was performed via a laparoscopic approach (Fig. 1C). During the procedure, shunt cather was spontaneously retrived into abdominal cavity while putting away overlying omentum. However, laparascopist could not find diaphragmtic opening into the thoracic cavity that distal catheter had passed. No attempt was made to inspect the inferior surface of the diaphragm or a perforation, because this would have required a repair the opening of the diaphragm.
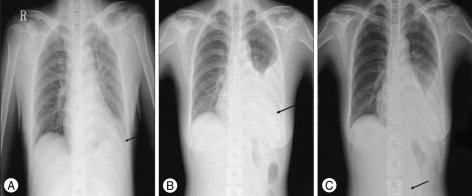
Fig. 1.
Serial chest X-ray. A : The shunt catheter is located in left upper quadrant of abdominal cavity and mild blunting of the left costophrenic angle is observed after initial ventriculoperitoneal shunt, B : The left pleural effusion with the suspicion of catheter migration into thoracic cavity is shown at second admission, C : After laparoscopic catheter reposition, the catheter is located in abdominal cavity and pleural effusion is lessened.
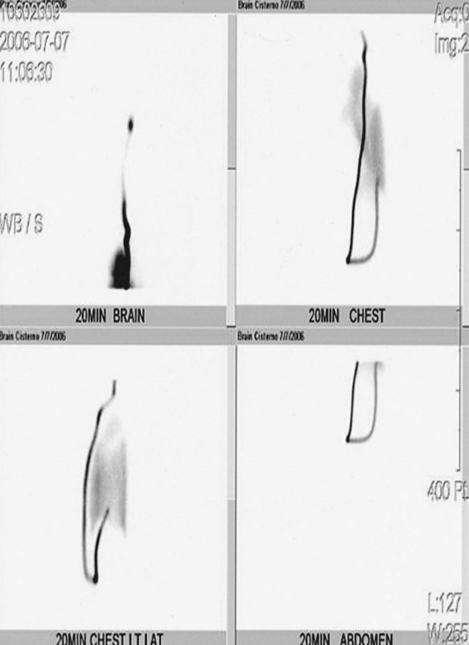
Fig. 2.
Shuntogram demonstratingcerebral spinal fluid drainage into intrathoracic cavity.
Her symptoms subsided after laparoscopy. She recovered uneventfully and discharged. One year after laparoscopic reposition of catheter, other specific respiratory symptoms have not been recurred.
DISCUSSION
The complications of the ventriculoperitoneal shunt include the blockage of the catheter (15.3%), infection (8.2%), seizure (7.1%) and the other complications related to shunt device (6.1%).2,8) Common thoracic complications after VP shunt include pleural effusion, bronchial perforation, pneumothorax, and pneumonia.
In 1994, Taub and Lavyne proposed possible mechanisms of intrathoracic complications into three types : 1) thoracic trauma during placement of a shunt, 2) migration of the distal catheter into the thoracic cavity through the diaphragmaic hole, and 3) pleural effusion accompanying CSF ascites without migration of the catheters into the thoracic cavities, often in chidren4,9,10).
Intrathoracic migrations of distal shunt catheters are classified into two types : supradiaphragmatic and transdiaphragmatic migration. In supradiphragmatic migration, the site of entry to the chest is an incorrect subcutaneous passage formed during distal tunneling procedure, frequently at supraclavicular fossa. So, the catheter may unconsciously be passed into and out of the thoracic cavity. During respirations, negative inspiratory pressure would then have slowly drawn the entire distal shunt catheter into chest.1) In cases of transdiaphragmatic intrathoracic migration of a peritoneal catheter, the presence of congenital diaphragmatic hiatuses, foramen of Morgagni or foramen of Boschdalek, might allow a prolapse of the peritoneal catheter into the thoracic cavity3,7). These two locations are the weak points of the diaphragm. Other authors suggested that the catheter could migrate as a result of an inflammatory process facilitating erosion and perforation of the diaphragm and prolapse of the catheter into the thoracic cavity5).
In the present case, the catheter was located at left upper quadrant of abdomen until re-admission. Thereby, we inferred that catheter would migrate as a result of an inflammatory process irritating erosion and making small opening of the diaphragm by the catheter tip. Through this case and rewiew of related cases, meticulous surgical technique and prudent diagnostic consideration about the thoracic complication should be considered during VP shunt operation.
CONCLUSION
We present a case of hydrothorax developed after VP shunt placement. Respiratory distress after VP shunt placement should be considered as an unusual but important thoracic complication. It is important to keep in mind the possibility of VP shunt catheter migration into the thoracic cavity. As in this case, we recommend laparascoy as the method of catheter reposition.
References
- 1.Akyuz M, Ucar T, Goksu E. A thoracic complication of ventriculoperitoneal shunt : symptomatic hydrothorax from intrathoracic migration of a ventriculoperitoneal shunt catheter. Br J Neurosurg. 2004;18:171–173. doi: 10.1080/02688690410001681046. [DOI] [PubMed] [Google Scholar]
- 2.Beach D, Manthey DE. Tension hydrothorax due to ventriculopleural shunting. J Emerg Med. 1998;16:33–36. doi: 10.1016/s0736-4679(97)00238-2. [DOI] [PubMed] [Google Scholar]
- 3.Cooper JR. Migration of ventriculoperitoneal shunt into the chest. Case report. J Neurosurg. 1978;48:146–147. doi: 10.3171/jns.1978.48.1.0146. [DOI] [PubMed] [Google Scholar]
- 4.Dickman CA, Gilbertson D, Pittman HW, Rekate HL, Daily WJ. Tension hydrothorax from intrapleural migration of a ventriculoperitoneal shunt. Pediatr Neurosci. 1989;15:313–316. doi: 10.1159/000120489. [DOI] [PubMed] [Google Scholar]
- 5.Doh JW, Bae HG, Lee KS, Yun IG, Byun BJ. Hydrothorax from intrathoracic migration of a ventriculoperitoneal shunt catheter. Surg Neurol. 1995;43:340–343. doi: 10.1016/0090-3019(95)80059-p. [DOI] [PubMed] [Google Scholar]
- 6.Gaudio D, De Tommasi A, Occhiogrosso M, Vailati G. Respiratory distress caused by migration of ventriculoperitoneal shunt catheter into the chest cavity : report of a case and review of the literature. Neurosurgery. 1988;23:768–769. doi: 10.1227/00006123-198812000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Hadzikaric N, Nasser M, Mashani A, Ammar A. CSF hydrothorax-VP shunt complication without displacement of a peritoneal catheter. Childs Nerv Syst. 2002;18:179–182. doi: 10.1007/s003810100504. [DOI] [PubMed] [Google Scholar]
- 8.Hu C, Han YP, Hong SK, Pyen JS, Kim HJ. The Analysis of Complications after Ventriculoperitoneal Shunt for Hydrocephalus. J Korean Neurosurg Soc. 1987;16:781–790. [Google Scholar]
- 9.Lourie H, Bajwa S. Transdiaphragmatic migration of a ventriculoperitoneal catheter. Neurosurgery. 1985;17:324–326. doi: 10.1227/00006123-198508000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Taub E, Lavyne MH. Thoracic complications of ventriculoperitoneal shunts : Case report and review of the literature. Neurosurgery. 1994;34:181–183. doi: 10.1097/00006123-199401000-00028. discussion 183-184. [DOI] [PubMed] [Google Scholar]