Abstract
Objective
To evaluate the clinical characteristics and surgical outcomes of the patients with cervical spondylotic myelopathy associated with athetoid cerebral palsy.
Methods
The authors reviewed the clinical and neurodiagnostic findings, surgical managements and outcomes in six consecutive patients with cervical spondylotic myelopathy associated with athetoid cerebral palsy who had been treated with surgical decompression and fusion procedures between January 1999 and December 2005. The mean age of the 6 patients (four women and two men) at the time of surgery was 42.8 years (range, 31-55 years). The mean follow-up period was 56.5 months (range, 17-112 months). The neurological outcome was evaluated before and after operations (immediately, 6 months after and final follow-up) using grading systems of the walking ability, brachialgia and deltoid power.
Results
At immediate postoperative period, after 6 months, and at final follow-up, all patients showed apparent clinical improvements in walking ability, upper extremity pain and deltoid muscle strength. Late neurological deterioration was not seen during follow-up periods. There were no serious complications related to surgery.
Conclusion
Surgical decompression and stabilization in patients with cervical spondylotic myelopathy associated with athetoid cerebral palsy have been challenging procedure up to now. Our results indicate that early diagnosis and appropriate surgical procedure can effectively improve the clinical symptoms and neurological function in patients with cervical spondylotic myelopathy and athetoid cerebral palsy, even in those with severe involuntary movements.
Keywords: Cerebral Palsy, Spinal Cord Compression, Decompression, Instrumentation
INTRODUCTION
Patients with athetoid cerebral palsy (CP) show various involuntary movements of their neck, face, arms and upper body. Early onset of degeneration of the cervical spine, deformity and instability due to sustained abnormal muscular tonicity or excessive movement of the neck are found in patients with athetoid type of cerebral palsy10,11). Cervical spondylotic myelopathy, associated cerebral palsy, is a serious secondary disability for the people who already have this congenital handicap19). But, it is not easy to determine whether new neurological symptoms are as a result of the cervical spinal disorder with myelopathy6). Preexisting spastic weakness of the extremities and abnormal movement may interfere with identification of progressive myelopathy. There have been a few reports on variable operative managements in patients with adult cervical spondylotic myelopathy associated with athetoid cerebral palsy2,8,9,18). In Korea, however, there have been only a few reports on operative management in patient with adult cervical spondylotic myelopathy associated with athetoid cerebral palsy.
In this study, we analysed the patient's clinical courses, the radiologic findings and the surgical results of the techniques after operative treatment for cervical spondylotic myelopathy in athetoid cerebral palsy.
MATERIALS AND METHODS
Patient population & surgical procedures
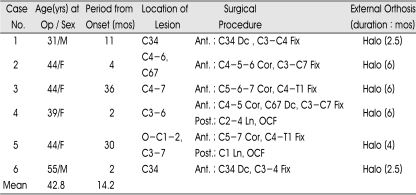
Between January 1999 and December 2005, six patients with cervical spondylotic myelopathy secondary to athetoid cerebral palsy underwent surgical decompression and fusion at our hospital. The mean age of the 6 patients (four women and two men) at the time of surgery was 42.8 years(range 31-55 years). Before the onset of myelopathy, 3 patients could walk without assistance; one could walk with a cane and two could not ambulate at all. At the time of admission, three patients could not walk, two could walk only with assistance, and one could walk without assistance. Upper extremity pain was classified as Grade 4 in 2 patients, Grade 5 in four patients, according to the Denis Pain Scale5). An manual muscle test (MMT) revealed deltoid muscle weakness in all patients (four Grade 3, two Grade 4). The mean duration of deterioration, beginning with numbness in the extremities and continuing with a decline in muscular or walking abilities that led to surgery, was 14.2 months (range 2-36 months) (Table 1).
Table 1.
Case summary
Op : Operation, yrs : years, Mos : Months, Ant. : Anterior, Post. : Posterior, Dc : Discectomy, Fix : Fixation, Cor : Corpectomy, Ln : Laminectomy, Ocf : Ociipito-cervical fusion
Surgical procedures performed included one level anterior discectomy with fusion (two patient), three level anterior corpectomy with fusion (two patients) and two or three level anterior corpectomy, anterior fusion and staged posterior decompression with occipi tocervical fusion (two patients). Post operative immobilizations were attained with halo-vests at the all patients (range : 2.5-6 months).
Clinical evaluation
Six patients were followed for more than 17 months (mean follow up 56.5 months, range 17-112 months). Preoperative and postoperative clinical evaluation were done by questionnaires in which the patients were asked about upper extremity pain, and neurological examination to evaluate walking ability and deltoid muscle function. Ambulation was classified into three grades : Grade 1, able to ambulate without help; Grade 2, able to ambulate using a cane or other assistance; and Grade 3, unable to ambulate and requiring a wheelchair19). Upper extremity pain was rated according to the Denis Pain Scale5). Deltoid muscle strength was evaluated using Manual Muscle Test (MMT). Neulologic evaluations were evaluated by estimation of the upper and lower extremity motor power, upper extremity pain. Each parameters were assessed using the walking ability grading (on lower extremity motor power), deltoid power grading by the MMT (on upper extremity power) and upper extremity pain scale (Denis pain scale). Surgery-related results were assessed as excellent (improvement of more than two grades), good (improvement of one grade), or poor (no improvement or deterioration).
RESULTS
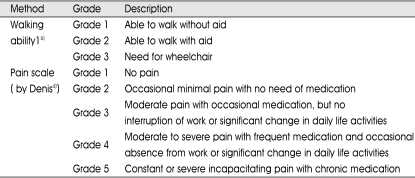
Walking ability
Two patients who were not able to ambulate since childhood were not improved. Function in one patient who was able to walk without assistance preoperatively was maintained after surgery. In other patient, status improved from Grade 3 to 1 in whom result was judged to be excellent. Additionally, outcome in two were classified as good in those improving one grade (from Grade 2 to 1) (Table 2 and 3).
Table 2.
Methods of the clinical evaluation
Table 3.
Clinical Results
F/up : Follow up, mo:month, pre : preoperative, 6 months : 6 months after operation, final : final follow up
Pain status
In six patients with preoperative upper extremity pain, relief at final follow-up examination was excellent in five (improving two or three grades) and good in one (improving one grade).
Deltoid muscle strength status
Of the six patients in whom deltoid muscle weakness was demonstrated preoperatively, postoperative improvement was excellent in one and good in three patient. Two patients with muscle strength of Grade 3 and 4 experienced no improvement. Results at the final follow-up examination did not differ appreciably from those at 1 year.
Surgical complications
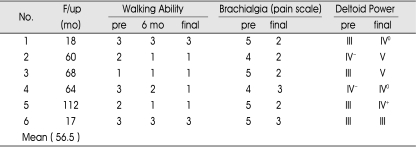
There were no serious complications related to surgery. Aggravation of weakness and spasticity of the lower extremities were seen in one patient in whom anterior decompression for the diseased upper level was not adequate, was relieved with posterior extended decompression and fusion (Fig. 1).
Fig. 1.
This 39-year-old woman developed progressive quadriparesis and intractable upper extremity pain in the one month before admission. An preoperative lateral x-ray (A) and MR sagittal image (B) of the cervical spine demonstrate degenerative changes and severe cord compression at C3-4, C5-6, and C6-7. She underwent anterior C4, 5 corpectomy and C6-7 discectomy, C3-C7 anterior plating with fusion (C). Her symptoms was improved immediately after operation. Two days after operation, progressive quadriplegia was developed. Follow up MRI shows severe, focal compression with signal change of the cord at the upper portion of the operative area (D). Laminectomy and occipitocervical fusion by posterior approach followed by halo vest apply was done. After second operation, her walking ability was slowly gained, she walked independantly 1 month later. Lateral x-ray film obtained 68 months postoperatively (E).
Transient worsening of the paresthesia and pain was seen in the two cases.
Neither breakages of the plates and rods nor fractures of the screws occurred.
Slight inferior screw backout occurred in two patients, but screw dislodgments were not progressed by maintenance external fixation with halovest and posterior wide fixation procedure, and the screws remained at the same positions.
In 4 patients of them, loosening and/or infection of the insertion sites of screws of the halovest were observed several times due to persistant, involuntary neck motion. Characteristically, other 2 cases, performed anterior and occipitocervical fusion, were not associated with the complication related with application of the halo device (Figs. 1, 2).
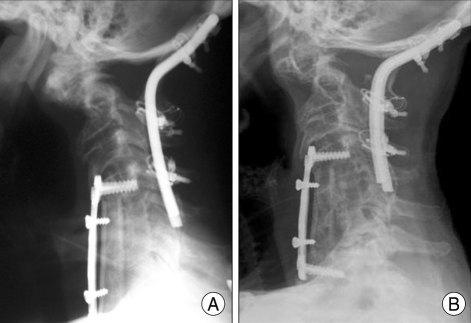
Fig. 2.
This case was a 44-year-old woman with cerebral palsy. She presented with gradual deterioration of the ambulation ability, severe pain and weakness at the both shoulders for over 30 months. Combined anterior and posterior decompression with instrumentations were done for the C1-2 instability and multilevel cervical stenosis (Occiput-C1-2, C4-T1), and then halovest application was done for 4 months. There were no screw loosening and pin site infection of the halovest. A : Plain radiographs, one month after operation. B : Plain radiographs, 112 months after operation. Cervical lateral x-ray shows fusion of occiput-T1 and no any instrument related failure.
DISCUSSION
Early onset of degeneration of the cervical spine and instability due to sustained abnormal tonicity or abnormal movement of the neck are found in patients with cerebral palsy10,11). Dystonic athetoid neck movements may cause excessive axial neck rotation as well as flexion and extension movements of the spine. These repetitive exaggerated movements may result in early degenerative changes of the vertebrae which may enhance the myeloradiculopathy11). Although adult athetoid cerebral palsy patients associated with the late onset of functional deterioration are related with variable causes, an unexplained change or deterioration of neurological function in patients with cerebral palsy should merit the consideration of the possibility of cervical myelopathy due to early degeneration or instability of the cervical spine14,15). In addition to compression against neural elements by canal stenosis from excessive spondylotic changes, severe dynamic instability of the spine induced by sustained involuntary movements and malalignment of the cervical spine due to the long-lasting strain of cervical muscle imbalance are the main pathologic factors leading to the serious disability. As well as the adequate decompression of the compressed neural elements (cord and/or roots), stabilization of the cervical spine and correction of the malalignment are the most important surgery-related goals in cases of this disease, and therefore extremely rigid fixation should be required19,28).
Clinically, there are many characteristic features in patients with athetoid cerebral palsy compared with other patients without this disease11). Onset of the clinical symptoms and signs of the myelopathy are usually seen in the earlier ages than other patients2,19,20,28). In our studies, average age at the time of surgery was 40.4 years (range, 31-40.4 years). The most characteristic feature of this pathology is that in most patients the lesions ocucur at several intervertebral levels and they are often caused by severe dynamic instability, mostly between C3 and C4, and between C4 and C54,19,28). Moreover, dysfunction such as weakness of the muscles and atrophy in the upper extremities considered to be a disorder of the anterior horn of the spinal gray matter and/or roots of the C5 segment, are also frequently associated with the cervical lesions19).
Since the first report of cervical spondylotic myelopathy in patients with athetoid cerebral palsy, by Anderson et al. in 19621), surgical results have often be poor, because of the unusual operation conditions, such as the patient's involuntary movements and instability, that made conservative treatments , such as cervical orthosis, cervical halter traction, and medication. But, conservative treatment are usually not effective and may be dangerous because patient cannot maintain neck immobilization1,19).
In earlier era of the operation for cervical spondylotic myelopathy associated cerebral palsy, laminectomy was performed. But, laminectomy frequently caused spinal instability and consequent recurrence of symptoms in the relatively early postoperative period; subsequently, laminectomy was thought to be contraindicated in athetoid cerebral palsy1,15,27,28). Thereafter, anterior21,22) and/or posterior spinal fusions of several methods have been reported, and their short-term or mid-term results do not seem unsatisfactory. However, most of the reports are small cases and long-term follow-up studies are very rare.
Several reports have shown that multilevel anterior decompression and fusion may lead to good clinical results if bony fusion could be obtained without such complications as significant graft extrusion and hardwarerelated complications and kyphotic deformity21,22). But, several physicians, who carried out the long-term followup studies, reported that considerable patients had shown recurrence of symptoms9). These patients showed instability of the upper cervical spine including atlantoaxial lesion in addition to degenerative changes at the levels adjacent to the fused vertebra. They showed development of kyphosis first, followed by atlantoaxial instability26). It seems that loss of midcervical spine motion by fusion increases the shearing force further, and in kyphotic curvature the anterior shearing force increases still more. Despite the risk of late deterioration, anterior decompression and fusion still may be indicated under some conditions; severe unstable slippage, large disc herniation, or severe kyphosis in which the surgical effect of laminoplasty seems questionable24).
Multilevel anterior cervical fusion is associated with significant graft extrusion and vertebral body fracture rates and pseudoarthrosis13). In athetoid cerebral palsy patients, who have the difficulty in maintenance of the fixation due to sustained involuntary movement of the neck and whole body, prevention of the these complications are mainstay of the postoperative management till completion of the bony union. In our study, partial pulled-out of the inferior screws were observed in two cases in postoperative 2-3 days. We conducted the posterior decompression, occipitocervical fusion and application of the halo vest for the case showing remaining cord compression of the upper level and halo vest only for the other case. Further pull-out didn't occur in both of them for the follow up period.
For the effective immobilization of the neck and fast fusion, we applied halo-vest for all the patients (range 2.5-6 months). In 4 cases who underwent anterior decompression and fixation only, recurrent skeletal fixation screw dislodgement and infection were developed due to sustained involuntary movement of the neck and body. In other 2 cases with combined anterior and posterior stabilization procedures, failure of the halo devices was not seen. These results imply that combined anterior/posterior fusion for the cervical spondylotic myelopathy in patients with athetoid cerebral palsy may provide the advantage of maintaining neck immobility and reduction of the complications related to the graft and hardware failure.
Onari et al. and Epstein et al. reported good surgical outcomes in the athetoid cerebral palsy patients who received combined anterior-posterior fusion. It seems that combined approaches may have several advantages; the prevention of the failures of the graft and hardware, stabilization of the dynamic instability as main pathology causing cervical myelopathy, and reducing dependency on the postoperative halo fixation7,9,13,19,20).
In two patients of our series, occipitocervical fusions with posterior and/or anterior decompression were performed with good clinical and radiological outcomes postoperatively not causing surgery-related and halo device-related complication. Anterior or posterior decompression with whole cervical spine fusion, which extends from the occipital bone to the upper thoracic spine, may be another way to avoid the harmful influence of the local fusion (delayed atlantoaxial instability or kyphotic deformity), especially in cases needed long-level upper cervical decompression and fusion2) (Fig. 2). However, there has been a debate on the application as the first procedure because complete loss of neck motion may cause discomfort to the patient.
Recently, Traynelis et al., and Racette et al., reported good results after anterior fusion and appliance of the halo device following botulism toxin-induced neck muscle denervation for overcome the problem of the postoperative sustained neck motion. These muscle tension-releasing methods may be effective in terms of increasing bone union rates. However, it seems that usefulness of the toxin is limited the questionable long-term effectiveness, necessity of the repeated injection, high cost, and possibility of the serious complication of the toxin injection3,23,25).
Several study groups suggested laminoplasty as a better choice than anterior decompression and fusion because patients with athetoid cerebral palsy often show multilevel disc degeneration and spinal canal stenosis. However, laminoplasty, similar to the posterior fusion, shows a tendency to decrease range of motion of the cervical spine and may pose a harmful influence of local fusion. Also, other reports indicated that pain and muscular decline in the upper extremities could not be alleviated by laminoplasty2,24). But, recently, Ueda et al. reported that cervical laminoplasty combined with muscle (splenius capitis, semispinalis, sternocleidomastoid muscles) release can improve clinical outcomes 1 year after surgery27).
CONCLUSION
Surgical decompressions and stabilizations in patients with cervical spondylotic myelopathy associated with athetoid cerebral palsy have been challenging procedure up to now. Our study results indicate that early diagnosis and appropriate surgical procedure can effectively improve the clinical symptoms and neurological function in patients with cervical spondylotic myelopathy associated athetoid cerebral palsy, even in those with severe involuntary movements. It seems that more extensive decompression is effective for relief of the neurologic symptoms and signs and prevention of the unexpected complications related with remaining constriction of the cord. Also, combined anterior-posterior fixation with fusion can effectively reduce the complications related with application of the halo vest, accelerate fusion and provide stability of the lesion site. However, long-term follow up evaluation is necessary in any type of operation because these patients undergo operation at a younger age and have a potential risk of late cervical deformity or neurological deterioration by their athetoid neck movements.
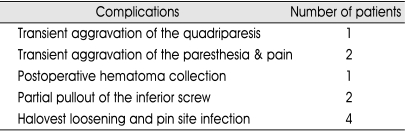
Table 4.
Surgical complications
References
- 1.Anderson WW, Wise BL, Itabashi HH, Jones M. Cervical spondylosis in patients with athetosis. Neurology. 1962;12:410–412. doi: 10.1212/wnl.12.6.410. [DOI] [PubMed] [Google Scholar]
- 2.Azuma S, Seichi A, Ohnishi I, Kawaguchi H, Kitagawa T, Nakamura K. Long-Term Results of Operative Treatment for Cervical Spondylotic Myelopathy in Patients With Athetoid Cerebral Palsy. An Over 10-Year Follow-Up Study. Spine. 2002;27:943–948. doi: 10.1097/00007632-200205010-00011. discussion 948. [DOI] [PubMed] [Google Scholar]
- 3.Basciani M, Intiso D, Cioffi RP, Tonali P. Preoperative treatment with botulinum A toxin in patients with cervical disk herniation secondary to dystonic cerebral palsy. Neurol Sci. 2000;21:63. doi: 10.1007/s100720070122. [DOI] [PubMed] [Google Scholar]
- 4.Cho YJ, Lee MH, Chang SK. Cervical Radiographic Study in Adolescence Cerebral Palsy. J Korean Acad Rehabil Med. 1998;22:543–551. [Google Scholar]
- 5.Denis F, Armstrong GW, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res. 1984;189:142–149. [PubMed] [Google Scholar]
- 6.Duruflé A, Pétrilli S, Le Guiet JL, Brassier G, Nicolas B, Le Tallec H, et al. Cervical spondylotic myelopathy in athetoid cerebral palsy patients about five cases. Joint Bone Spine. 2005;72:270–274. doi: 10.1016/j.jbspin.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Epstein NE. Circumferential cervical surgery for spondylostenosis with kyphosis in two patients with athetoid cerebral palsy. Surg Neurol. 1999;52:339–344. doi: 10.1016/s0090-3019(99)00117-2. [DOI] [PubMed] [Google Scholar]
- 8.Fuji T, Yonenobu K, Fujiwara K, Yamashita K, Ebara S, Ono K, et al. Cervical radiculopathy or myelopathy secondary to athetoid cerebral palsy. J Bone Joint Surg Am. 1987;69:815–821. [PubMed] [Google Scholar]
- 9.Haro H, Komori H, Okawa A, Shinomiya K. Surgical treatment of cervical spondylotic myelopathy associated with athetoid cerebral palsy. J Orthop Sci. 2002;7:629–636. doi: 10.1007/s007760200113. [DOI] [PubMed] [Google Scholar]
- 10.Chambers Henry G. Advances in cerebral palsy. Curr Opin Ortho. 2002;13:424–431. [Google Scholar]
- 11.Kidron D, Steiner I, Melamed E. Late-onset progressive radiculomyelopathy in patients with cervical athetoid-dystonic cerebral palsy. Eur Neurol. 1987;27:164–166. doi: 10.1159/000116150. [DOI] [PubMed] [Google Scholar]
- 12.Kikkawa J, Shirado O, Saito F, Takahashi K, Oda H. Quadriparesis Due to Intraspinal Cyst After Failed Posterior Occipitocervical Fusion in a Patient With Athetoid Cerebral Palsy. Spine. 2006;31:E980–E983. doi: 10.1097/01.brs.0000248125.30498.f3. [DOI] [PubMed] [Google Scholar]
- 13.Kim JG, Kim SW, Lee SM, Shin H. Surgical Result of the Combined Anterior and Posterior Approach in Treatment of Cervical Spondylotic Myelopathy. J Korean Neurosurg Soc. 2006;39:188–191. [Google Scholar]
- 14.Kim JS, Ryu KH, Yang SH. Management of Cervical Myelopathy in Athetoid Cerebral Palsy : Case report. J Korean Acad Rehabil Med. 1998;22:1136–1140. [Google Scholar]
- 15.Ko HY, Park-Ko I. Spinal cord injury secondary to cervical disc herniation in ambulatory patients with cerebral palsy. Spinal Cord. 1998;36:288–292. doi: 10.1038/sj.sc.3100607. [DOI] [PubMed] [Google Scholar]
- 16.Levine RA, Rosenbaum AE, Waltz JM, Scheinberg LC. Cervical spondylosis and dyskinesias. Neurology. 1970;20:1194–1199. doi: 10.1212/wnl.20.12.1194. [DOI] [PubMed] [Google Scholar]
- 17.McCluer S. Cervical spondylosis with myelopathy as a complication of cerebral palsy. Paraplegia. 1982;20:308–312. doi: 10.1038/sc.1982.58. [DOI] [PubMed] [Google Scholar]
- 18.Nishihara N, Tanabe G, Nakahara S, Imai T, Murakawa H. Surgical treatment of cervical spondylotic myelopathy complicating athetoid cerebral palsy. J Bone Joint Surg Br. 1984;66:504–508. doi: 10.1302/0301-620X.66B4.6746682. [DOI] [PubMed] [Google Scholar]
- 19.Onari K, Kondo S, Mihara H, Iwamura Y. Combined anterior and posterior fusion for cervical spondylotic myelopathy in patients with athetoid cerebral palsy. J Neurosurg. 2002;97(1 Suppl):13–19. doi: 10.3171/spi.2002.97.1.0013. [DOI] [PubMed] [Google Scholar]
- 20.Onari K. Surgical treatment for cervical spondylotic myelopathy associated with athetoid cerebral palsy. J Orthop Sci. 2000;5:439–448. doi: 10.1007/s007760070021. [DOI] [PubMed] [Google Scholar]
- 21.Pollak L, Schiffer J, Klein C, Mirovsky Y, Copeliovich L, Rabey JM. Neurosurgical intervention for cervical disk disease in dystonic cerebral palsy. Mov Disord. 1998;13:713–717. doi: 10.1002/mds.870130418. [DOI] [PubMed] [Google Scholar]
- 22.Pollak L, Schiffer J, Klein C, Mirovsky Y, Copeliovich L, Rabey JM. Neurosurgical intervention for cervical disk disease in dystonic cerebral palsy. Mov Disord. 1998;13:713–717. doi: 10.1002/mds.870130418. [DOI] [PubMed] [Google Scholar]
- 23.Racette BA, Lauryssen C, Perlmutter JS. Preoperative treatment with botulinum toxin to facilitate cervical fusion in dystonic cerebral palsy. J Neurosurg. 1998;88:328–330. doi: 10.3171/jns.1998.88.2.0328. [DOI] [PubMed] [Google Scholar]
- 24.Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, et al. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine. 2001;26:479–487. doi: 10.1097/00007632-200103010-00010. [DOI] [PubMed] [Google Scholar]
- 25.Traynelis VC, Ryken T, Rodnitzky RL, Menezes AH. Botulinum toxin enhancement of postoperative immobilization in patients with cervical dystonia. Technical note. J Neurosurg. 1992;77:808–809. doi: 10.3171/jns.1992.77.5.0808. [DOI] [PubMed] [Google Scholar]
- 26.Tsirikos AI, Chang WN, Shah SA, Miller F. Acquired Atlantoaxial Instability in Children With Spastic Cerebral Palsy. J Pediatr Orthop. 2003;23:335–341. [PubMed] [Google Scholar]
- 27.Ueda Y, Yoshikawa T, Koizumi M, Iida J, Miyazaki K, Nishiyama S, et al. Cervical Laminoplasty Combined With Muscle Release in Patients With Athetoid Cerebral Palsy. Spine. 2005;30:2420–2423. doi: 10.1097/01.brs.0000184691.49314.41. [DOI] [PubMed] [Google Scholar]
- 28.Wong AS, Massicotte EM, Fehlings MG. Surgical Treatment of Cervical Myeloradiculopathy Associated with Movement Disorders ; Indications, Technique, and Clinical Outcome. J Spinal Disord Tech. 2005;18:S107–S114. doi: 10.1097/01.bsd.0000128693.44276.86. [DOI] [PubMed] [Google Scholar]