Abstract
Objective
Total laminectomy (TL) is an effective surgical technique for the treatment of cervical ossification of the posterior longitudinal ligament (OPLL) along multiple levels. However, kyphosis and probable neurological deterioration have been frequently reported after laminectomy. We analyzed the changes in the cervical curvature after TL and subsequent changes in neurological status.
Methods
We retrospectively reviewed the records of 14 patients who underwent TL for the treatment of cervical OPLL between Jan. 1998 and Dec. 2003. TL was selected according to the previously determined criteria. The curvature of the cervical spine was visualized on a lateral cervical spine X-ray and measured using Ishihara's Curvature Index (CI) before the operation and at the last follow-up examination. Perioperative neurological status was estimated using the modified Japanese Orthopedic Association score and the Improvement Rate (IR) at the same time as the images were evaluated.
Results
The mean age of the patients was 57 years, the male/female ratio was 10:4, and the mean follow-up period was 41 months. The mean number of OPLL was 4.9, and the mean number of operated levels was also 4.9. The CI decreased after TL (p=0.002), which was indicative of a kyphotic change. However, this kyphotic change showed no correlation with the length of the follow-up period, number of operated levels and preoperative CI. Neurological examination at the last follow-up showed an improved neurological status in all patients (p=0.001). There was no neurological deterioration in any case during the follow-up period. Moreover, there was no correlation between IR and the degree of kyphotic change. Postoperative complications, such as C5 radiculopathy and epidural bleeding, resolved spontaneously without neurological sequelae.
Conclusion
Kyphotic change was observed in all but one patient who underwent TL for the treatment of cervical OPLL. However, we did not find any contributing factors to kyphosis or evidence of postoperative neurological deterioration.
Keywords: Total laminectomy (TL), Cervical, Ossification of posterior longitudinal ligament (OPLL), Kyphotic change, Neurological status
INTRODUCTION
The use of surgery for the treatment of cervical myelopathy with ossification of the posterior longitudinal ligament (OPLL) has been controversial. In general, anterior cervical decompression and fusion (ACDF) has shown better results than posterior decompression5). However, the rate of fusion decreases and the rate of complication increases11) with ACDF in cases of multiple level involvement, especially in patients with more than three levels of vertebral body involvement23,24). Thus, much attention has been paid to laminectomy. Although laminectomy is an indirect surgical approach and the direct removal of the ossified ligament is impossible with laminectomy, it has been proven to be effective in the treatment of multi-level spondylosis. Laminectomy has been associated with complications and alignment changes in some patients. In particular, kyphosis is alignment change that has been known to follow laminectomy13). Thus, laminoplasty was developed in 1977, and many types of surgical techniques for reducing kyphosis have been introduced. Studies aimed at decreasing kyphosis have identified a few causes of kyphosis, such as wide facetectomy or capsule resection, age, posterior soft tissue preservation, and so on.
Why does post-laminectomy kyphosis in the cervical spine attract the interest of many researchers? The reason is that kyphosis has the potential to deteriorate a patient's neurological status. However, whether it gives rise to neurological deterioration or not has yet to be determined. The neurological effects of kyphosis differ from those of other lesions, such as OPLL, herniated intervertebral discs, and so on. Other lesions provoke neurological problems mainly by direct injury to the spinal cord and ischemia with vessel compression in some areas. On the other hand, kyphosis itself is thought to raise problems gradually through traction of the spinal cord and ischemia due to the stretching and flattening of small vessels.
The authors analyzed the postoperative changes in the cervical curvature. They also sought to identify subsequent changes in neurological status as well as factors that contribute to the curvature and clinical results.
MATERIALS AND METHODS
Patient selection
We retrospectively reviewed the records of all patients who underwent surgery for cervical OPLL between January 1998 and December 2003 in our institute. Surgery was indicated for those who suffered from myelopathy and radiculopathy after taking medication for more than 3 months. Total laminectomy (TL) was performed in patients with OPLL of the continuous type with involvement of more than 4 levels of vertebral body or 3 levels of intervertebral disc spaces. Patients who were followed up at an outpatient clinic for at least 24 months after TL and in whom complete medical records and imaging data were available were included in the study. Patients with severe comorbidity, another cerebral disease with symptoms and signs resembling cervical myelopathy, problems in the thoracic or lumbar spine, those who underwent a circumferential operation, or experienced postoperative complications, except for neurological problems, were excluded.
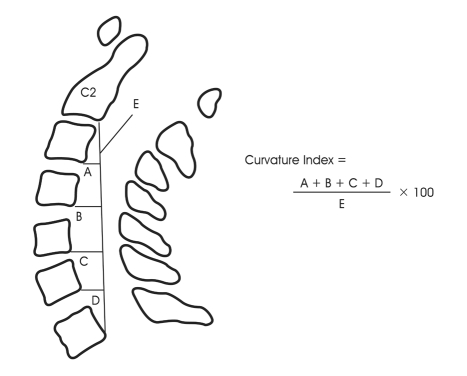
Evaluation of kyphosis
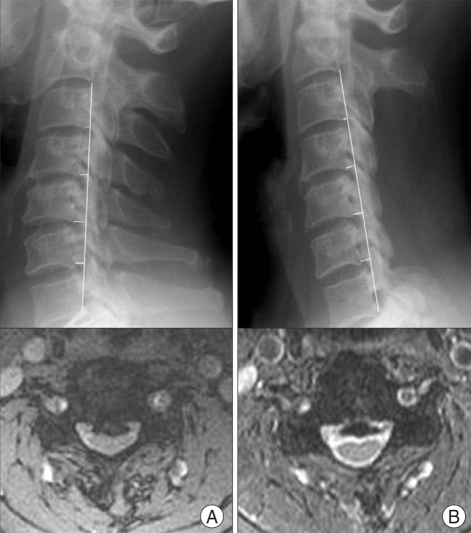
The curvature of the cervical spine was evaluated using the Ishihara's Curvature Index (CI)10) (Fig. 1). The CI was defined on lateral simple X-ray in the standing position (Fig. 2A-1, B-1): (A+B+C+D) / E × 100, as the CI decreases, the curvature becomes kyphotic. 'A' was defined as the distance from the posteroinferior edge of the C3 vertebral body to line 'E', B' was the distance from the posteroinferior edge of C4 to line 'E', 'C' was the distance from the posteroinferior edge of C5, and 'D' was the distance from the posteroinferior edge of C6. 'E' was defined as the distance from the posterior/inferior edge of the C2 vertebral body to that of the C7 vertebral body. Pre- and postoperative CI values were calculated using lateral simple X-rays before the operation and at the last follow-up. The degree of kyphotic change (%) was calculated as : {(postoperative CI- preoperative CI)/preoperative CI} × 100. The follow-up period, number of operated levels and preoperative CI values were also evaluated in order to identify factors that contribute to kyphotic change.
Fig. 1.
Curvature Index (CI) on lateral cervical spine X-ray.
Fig. 2.
A-1, A-2 : Preoperative cervical spine X-ray and magnetic resonance (MR) image. B-1, B-2 : Postoperative cervical spine X-ray and MR image taken at the last follow-up examination. Pre- and postoperative curvature index values were calculated from lateral simple X-rays. The pre- and postoperative status of the cervical lesion and spinal cord were evaluated on MR images if there were other predisposing factors of neurological complications.
Neurological assessment
Neurological status was evaluated along with simple X-ray and MR images, just before the operation and at the last follow-up examination, using the modified Japanese Orthopedic Association (mJOA) score1). The mJOA scoring system yields a score of 17 points in patients with normal neurological function and 0 points in patients with the most severe myelopathy. To evaluate the relationship between kyphotic change and neurological status, improvement rate (IR) was defined2) as follows: IR =(postoperative mJOA score - preoperative mJOA score)/(17- preoperative mJOA score) × 100. The results obtained were categorized as follows : an IR of 75% or more=excellent, 50% to 74%= good, 25% to 49%=fair, less than 25%=poor.
Statistical analysis
Statistical analyses were performed using SPSS® (version 10.0, SPSS Inc., Chicago, IL, USA). Non-parametric analysis was carried out using the Wilcoxon signed rank test. Non-parametric correlation analysis was performed using Kendall's tau-b or Spearman's rho. All values are expressed as means with 95% confidence intervals.
RESULTS
General characteristics
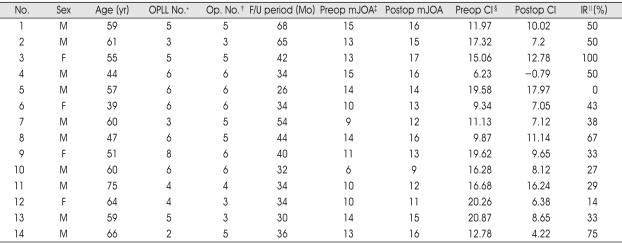
A total of 14 patients were finally selected. The male/female ratio was 10 to 4, the mean patient age was 57 years (range 39-75), and the mean follow-up period was 41 months (range 26-68 months). The mean number of OPLL levels was 4.9 (range 2-8 levels), and the mean number of operated levels was 4.9 (range 3-6 levels). Two patients who had less than 3 levels of OPLL were included because the OPLL lesion was the main cause of cervical myelopathy in these patients, and if the neighboring HIVD lesion had not been treated along with the OPLL lesion, the spinal cord could have been strangled. The presenting symptoms and signs included posterior neck pain, weakness and sensory changes in the upper and lower extremities, changes in voiding habits, and increases in deep tendon or pathologic reflexes. Patient information is listed in Table 1.
Table 1.
Summary of patient information
*The number of ossification of the posterior longitudinal ligament levels, †The number of operated levels, ‡Modified Japanese Orthopedic Association score, §Curvature Index, ‖Improvement rate
Change of curvature after TL
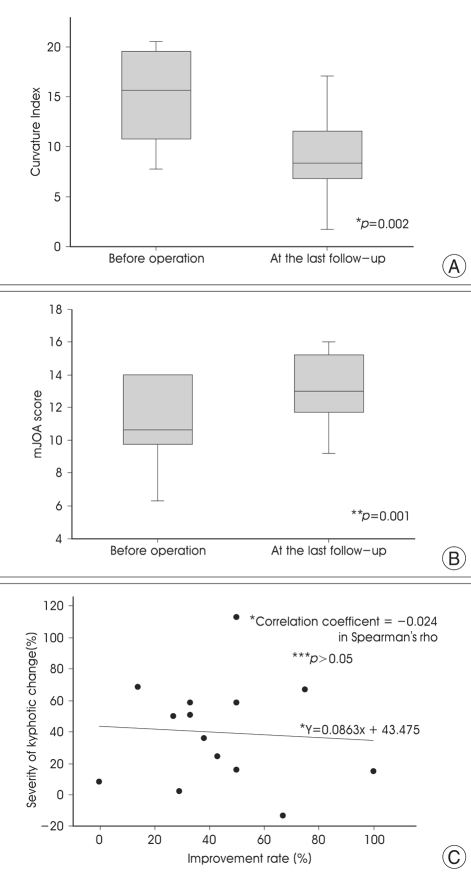
Comparison of the pre- and postoperative CI values revealed that the CI decreased significantly postoperatively (Fig. 3A, p=0.002 in Wilcoxon signed rank test), which is indicative of a kyphotic change. Postoperative CI was increased in only one case (case 8). To determine the factors that influence kyphotic changes, several factors, such as the length of the follow-up period, number of operated levels and preoperative CI, were investigated. There was no significant correlation between the degree of kyphotic change and the length of the postoperative follow-up period, number of operated levels, or preoperative CI (p>0.05 in Kendall's tau-b or Spearman's rho).
Fig. 3.
Box graph and scatter diagram. The error bars and three lines in the vertical box in the box graph represent the cut-off values for the 90th, 75th, median, 25th, and 10th percentiles. A : Comparison of pre- and postoperative curvature of the cervical spine using the Curvature Index (CI). The decrease in CI is indicative of a significant postoperative kyphotic change (*p=0.002). B : Comparison of pre- and postoperative neurological status as assessed by modified Japanese Orthopedic Association (mJOA) score shows a significant postoperative neurological improvement (**p=0.001). C : There was no significant correlation between the degree of kyphotic change and rate of improvement (***p>0.05, *correlation coefficient: -0.024 in Spearman's rho, -0.056 in Kendall's tau-b).
Change in neurological status after TL
The mean mJOA score was 11.9 (6-15 points) preoperatively and 13.9 (9-17 points) postoperatively, at the last follow-up evaluation. Deterioration of neurological status was not noted in any of the patients after the operation. Statistical analysis showed significant improvement (Fig. 3B, p=0.001 in Wilcoxon signed rank test). Neurological status was also evaluated right after the operation. There was no definite change, with the exception of a few cases, in which the associated postoperative complications were transient and resolved spontaneously. Comparison of the pre- and postoperative MR images confirmed sufficient decompression and no change in cord signal (Fig. 2A-2, B-2). In addition, there was no correlation between IR and the degree of kyphotic change (Fig. 3C, p>0.05 in Kendall's tau-b or Spearman's rho), indicating that there is no relationship between the degree of neurological improvement and the degree of kyphotic change.
Postoperative complications
Just after the operation, one case of epidural bleeding and three cases of C5 radiculopathy (consisting of shoulder pain, paresthesia and weakness of shoulder abduction) were identified. All of these complications were transient and resolved spontaneously without sequelae.
DISCUSSION
Preference for posterior decompression
Anterior decompression has been reported to be superior to posterior decompression in the treatment of cervical myelopathy5,15). However, when dealing with multiple levels, the rate of fusion may decrease3,23,24). Due to the failure of fusion at multiple levels, posterior decompression, including laminectomy and laminoplasty, has been introduced for multi-level stenosis. We also selected TL for posterior decompression in multi-level cases. Although posterior decompression is an indirect solution, this modality has proved to be effective at multiple levels28,29). Posterior decompression is associated with the so-called "total decompressing effect", which results from a posterior shift of the spinal cord7). However, if a patient has a movable pathologic segment or an anteriorly compressing lesion, whole or partial anterior decompression should be accepted, even in multilevel cases.
Laminectomy and kyphotic change
The incidence of kyphotic change after multi-level laminectomy in the cervical spine is approximately 20%13). The reported causes of post-laminectomy kyphosis include preoperative kyphosis, young age, extent of facetectomy or capsule resection, aggressiveness of posterior soft tissue resection, multiplicity of laminectomy level, and irradiation history. Facet injury is the most considerable cause of postoperative kyphosis. Extension of facetectomy and capsule resection of more than 50% are thought to cause significant kyphosis and instability30). In Pal et al.'s experiment with a cadaver20), 36% of the total load was transmitted through the vertebral body and disc, and 32% was transmitted in each of two facets. Finite element analysis of cervical spine biomechanics under physiologic loading18) demonstrated that the facet was responsible for anterior shear, extension, lateral bending, and torsion. Therefore, facetectomy was found to weaken resistance to torsional and extensive stress so that instability and angular deformity toward anterior flexion could develop.
In our result, kyphotic change occurred in 13 of 14 cases (93%), which is much higher than the results of previous reports. The reason for the discrepancy between the rate of kyphotic change in this study and those reported in the previous studies may be due to different definition of kyphosis used in this study from that used in the previous studies. In other reports, a certain degrees of kyphotic change in the spinal curvature was defined as kyphosis. However, in our report, we regarded it as a kyphotic change if the curvature showed even a slight kyphotic change (curvature index changed smaller).
In addition, we did not find any contributing factors, such as the number of operated levels, preoperative curvature and the length of the follow-up period. We tried to preserve the facet capsule during TL. However, because one clinician did not consistently examine the facet capsule in all cases and because this report is retrospective, the frequency with which facet injury occurred and whether it was related to kyphotic change cannot be estimated.
As postoperative kyphotic change may result in neurological deficits, a variety of surgical techniques and precautions have been mentioned in many reports. However, there is no definite evidence regarding the clinical outcome and degree of spinal kyphosis6,13). Only a presumptive pathophysiology has been suggested as follows2) : as kyphotic deformity progresses, the spinal cord may become draped over the posterior plane of the vertebral body, resulting in the flattening of small feeding vessels around the cord. In our results, there was no evidence of neurological deterioration related with kyphotic change after TL. For theses reasons, it is better to consider kyphotic change as a probable risk factor for neurological deterioration after TL rather than a definite risk factor. According to a report by Matsugana et al.16), pathological compression by the ossified ligament above a certain critical point may be the most important factor of myelopathy in cervical OPLL. Below the critical point, dynamic factors, such as trauma and sudden or recurrent increases in the cervical range of motion, may be more important.
Laminectomy and laminoplasty in postoperative kyphosis and neurological deterioration
Although laminectomy effectively decompresses the spinal cord in patients with cervical OPLL or multi-level cervical spondylotic myelopathy, it may result in instability, progressive kyphosis and late neurological deterioration. Thus, laminoplasty or laminectomy with fixation has been proposed and used8,14,19,25,26). A review of the literature regarding laminoplasty and related complications, especially kyphotic change12,14,21), revealed that the general result in the long-term follow-up of laminoplasty patients is similar to that in laminectomy patients9,17). In our institute, surgeons try to preserve the facet in all patients, and the choice of surgical technique is optional, depending on the surgeon's preference and the patient's status. A comparative study between laminoplasty and laminectomy is currently underway.
C5 radiculopathy
We experienced three cases of transient C5 radiculopathy after TL, presenting as shoulder pain, paresthesia and weakness of shoulder abduction. Although C5 radiculopathy occurs intermittently after posterior decompression, the mechanism by which this occurrence remains to be elucidated. The intradural tethering effect is one possible explanation. As the spinal cord shifts posteriorly after posterior decompression, the intradural portion of the anterior rootlets may be stretched at the fixed root sleeve. The extradural tethering effect is another possible explanation. As the dura mater expands posteriorly after the operation, the extradural portion of the root sleeve may be stretched27). Therefore, longitudinal durotomy or additional foraminotomy has been introduced as a surgical technique for preventing C5 radiculopathy22,27). Even though we had not applied these techniques before and C5 radiculopathy was temporary, when posterior decompression was selected, C5 neural foraminotomy, durotomy to release the tethering effect, or the removal of bony portions compressing the root after laminoplasty can be considered.
CONCLUSION
Kyphotic changes occurred in the majority of patients who underwent TL for the treatment of cervical myelopathy with OPLL. No contributing factors were identified. The neurological status of all patients improved postoperatively. Moreover, there was no evidence that kyphotic change influenced neurological status. However, TL is not considered as a standard treatment, but rather an alternative option, because OPLL remains and has the potential to grow larger. Apart from kyphotic changes and their neurological effect, patients, especially those with many risk factors, should be regularly followed up for a long period of time after TL.
References
- 1.Benzel EC, Lancon J, Kesterson L, Hadden T. Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J Spinal Disord. 1991;4:286–295. doi: 10.1097/00002517-199109000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Breig A, el-Nadi F. Biomechanics of the cervical spinal cord. Relief of contact pressure on and overstretching of the spinal cord. Acta Radiol Diagn (Stockh) 1966;4:602–624. doi: 10.1177/028418516600400602. [DOI] [PubMed] [Google Scholar]
- 3.Connolly PJ, Esses SI, Kostuik JP. Anterior cervical fusion : outcome analysis of patients fused with and without anterior cervical plates. J Spinal Disord. 1996;9:202–206. [PubMed] [Google Scholar]
- 4.Emery SE, Bohlman HH, Bolesta MJ, Jones PK. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am. 1998;80:941–951. doi: 10.2106/00004623-199807000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Epstein NE. The surgical management of ossification of the posterior longitudinal ligament in 43 north Americans. Spine. 1994;19:664–672. doi: 10.1097/00007632-199403001-00005. [DOI] [PubMed] [Google Scholar]
- 6.Gregorius FK, Estrin T, Crandall PH. Cervical spondylotic radiculopathy and myelopathy. A long-term follow-up study. Arch Neurol. 1976;33:618–625. doi: 10.1001/archneur.1976.00500090024005. [DOI] [PubMed] [Google Scholar]
- 7.Hirabayashi K, Bohlman HH. Multilevel cervical spondylosis. Laminoplasty versus anterior decompression. Spine. 1995;20:1732–1734. doi: 10.1097/00007632-199508000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine. 1988;13:870–876. doi: 10.1097/00007632-198807000-00032. [DOI] [PubMed] [Google Scholar]
- 9.Hukuda S, Ogata M, Mochizuki T, Shichikawa K. Laminectomy versus laminoplasty for cervical myelopathy : brief report. J Bone Joint Surg Br. 1988;70:325–326. doi: 10.1302/0301-620X.70B2.3346317. [DOI] [PubMed] [Google Scholar]
- 10.Ishihara A. [Roentgenographic studies of the normal pattern of the cervical curvature] Nippon Seikeigeka Gakkai Zasshi. 1968;42:1033–1044. [PubMed] [Google Scholar]
- 11.Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004;4:624–628. doi: 10.1016/j.spinee.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine : more than 10 years follow up. J Neurosurg. 2002;96(2 Suppl):180–189. [PubMed] [Google Scholar]
- 13.Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg. 2000;93(2 Suppl):199–204. doi: 10.3171/spi.2000.93.2.0199. [DOI] [PubMed] [Google Scholar]
- 14.Kawai S, Sunago K, Doi K, Saika M, Taguchi T. Cervical laminoplasty (Hattori's method). Procedure and follow-up results. Spine. 1988;13:1245–1250. [PubMed] [Google Scholar]
- 15.Kim YS, Chin DK, Cho YE, Jin BH, Yoon YS, Park JP, et al. Surgical treatment for ossification of the posterior longitudinal ligament of the cervical spine. J Korean Neurosurg Soc. 1997;26:1237–1245. [Google Scholar]
- 16.Matsugana S, Kukita M, Hayashi K, Shinkura R, Koriyama C, Sakou T, et al. Pathogenesis of myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg. 2002;96(2 Suppl):168–172. doi: 10.3171/spi.2002.96.2.0168. [DOI] [PubMed] [Google Scholar]
- 17.Nakano N, Nakano T, Nakano K. Comparison of the results of laminectomy and open-door laminoplasty for cervical spondylotic myeloradiculopathy and ossification of the posterior longitudinal ligament. Spine. 1988;13:792–794. doi: 10.1097/00007632-198807000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Ng HW, Teo EC, Lee KK, Qiu TX. Finite element analysis of cervical spinal instability under physiologic loading. J Spinal Disord Tech. 2003;16:55–65. doi: 10.1097/00024720-200302000-00010. [DOI] [PubMed] [Google Scholar]
- 19.O'Brien M, Peterson D, Casey AT, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine. 1996;21:474–483. doi: 10.1097/00007632-199602150-00012. discussion 484. [DOI] [PubMed] [Google Scholar]
- 20.Pal GP, Sherk HH. The vertical stability of the cervical spine. Spine. 1988;13:447–449. doi: 10.1097/00007632-198805000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Sasai K, Saito T, Akagi S, Kato I, Ogawa R. Cervical curvature after laminoplasty for spondylotic myelopathy-involvement of yellow ligament, semispinalis cervicis muscle, and nuchal ligament. J Spinal Disord. 2000;13:26–30. doi: 10.1097/00002517-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Sasai K, Saito T, Akagi S, Kato I, Ohnari H, Iida H. Preventing C5 palsy after laminoplasty. Spine. 2003;28:1972–1977. doi: 10.1097/01.BRS.0000083237.94535.46. [DOI] [PubMed] [Google Scholar]
- 23.Sasso RC, Ruggiero RA, Jr, Reilly TM, Hall PV. Early reconstruction failures after multilevel cervical corpectomy. Spine. 2003;28:140–142. doi: 10.1097/00007632-200301150-00009. [DOI] [PubMed] [Google Scholar]
- 24.Saunders RL, Pikus HJ, Ball P. Four-level cervical corpectomy. Spine. 1998;23:2455–2461. doi: 10.1097/00007632-199811150-00022. [DOI] [PubMed] [Google Scholar]
- 25.Shaffrey C, Wiggins GC, Piccirilli CB, Young JN, Lovell LR. Modified open-door laminoplasty for treatment of neurological deficits in young patients with congenital spinal stenosis : analysis of clinical and radiographic data. J Neurosurg. 1999;90(2 Suppl):170–177. doi: 10.3171/spi.1999.90.2.0170. [DOI] [PubMed] [Google Scholar]
- 26.Takayasu M, Takagi T, Nishizawa T, Osuka K, Nakajima T, Yoshida J. Bilateral open-door cervical expansive laminoplasty with hydroxyapatite spacers and titanium screws. J Neurosurg. 2002;96(1 Suppl):22–28. doi: 10.3171/spi.2002.96.1.0022. [DOI] [PubMed] [Google Scholar]
- 27.Tsuzuki N, Abe R, Saiki K, Zhongshi L. Extradural tethering effect as one mechanism of radiculopathy complicating posterior decompression of the cervical spinal cord. Spine. 1996;21:203–211. doi: 10.1097/00007632-199601150-00008. [DOI] [PubMed] [Google Scholar]
- 28.Wada E, Suzuki S, Kanazawa A, Matsuoka T, Miyamoto S, Yonenobu K. Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy : a long-term follow-up study over 10 years. Spine. 2001;26:1443–1447. doi: 10.1097/00007632-200107010-00011. discussion 1448. [DOI] [PubMed] [Google Scholar]
- 29.Yonenobu K, Hosono N, Iwasaki M, Asano M, Ono K. Laminoplasty versus subtotal corpectomy : a comparative study of results in multisegmental cervical spondylotic myelopathy. Spine. 1992;17:1281–1284. [PubMed] [Google Scholar]
- 30.Zdeblick TA, Abitbol J-J, Kunz DN, McCabe RP, Garfin S. Cervical stability after sequential capsule resection. Spine. 1993;18:2005–2008. doi: 10.1097/00007632-199310001-00013. [DOI] [PubMed] [Google Scholar]