Abstract
Objective
We assessed the surgical results of percutaneous balloon compression in 50 patients with idiopathic trigeminal neuralgia.
Methods
Fifty patients with follow-up period of more than 12 months were retrospectively analyzed. The mean follow-up period was 42 months (range, 12-82). The mean age was 65.8 years (range, 27-83). Seventeen patients (34%) had other previous surgical procedures. The balloon was inflated by injecting radio-contrast media under brief general anesthesia according to Mullan's technique. The mean inflating time was 88 seconds (range, 60-120). The whole procedure took about 20 minutes.
Results
We reported excellent and good results in 70% of the cases, poor in 6% as annoying dysesthesia, recurrence in 16%, and 8% failure due to technical deficiencies. Forty-six patients (92%) were initially relieved of their pain. There were permanent motor weakness of the masseter muscle in 4% of patients and transitory diplopia in 8%. Neither anesthesia dolorosa nor keratitis occurred. Almost all patients (92%) were discharged postoperatively within two days.
Conclusion
These results indicate that balloon compression would be an effective method with acceptable morbidity, technically, it can be performed rapidly and simply in the treatment of idiopathic trigeminal neuralgia.
Keywords: Trigeminal neuralgia, Percutaneous balloon compression
INTRODUCTION
Percutaneous balloon compression (PBC) of the trigeminal ganglion with a balloon catheter was introduced by Mullan and Lichtor9) in 1983. The technique derived from mechanical injury to the trigeminal ganglion originally performed during temporal craniotomies in the 1950s by Shelden and Pudenz3,9). As with radiofrequency rhizotomy and glycerol rhizotomy, balloon compression uses a controlled injury to interfere with the nerve's ability to transmit signals3) . Each procedure has its own attributes and limitations, and the procedure must be selected based on the individual patient's medical status currently. Little is known about PBC for trigeminal neuralgia in Korea1) . We reviewed our results in 50 cases of idiopathic trigeminal neuralgia associated with use of the balloon compression technique and compared its merits to those of other percutaneous procedures.
MATERIALS AND METHODS
From March 2000 through December 2006, 54 patients with idiopathic trigeminal neuralgia refractory to medical treatment or failure of a surgical procedure were operated on using PBC of the trigeminal ganglion. All patients had classical and unilateral pain. Computed tomography (CT), magnetic resonance image and skull basal X-ray studies were obtained. No patient had evidence of tumor, vascular malformation, multiple sclerosis, or related conditions. Four patients who were lost to follow-up were excluded from the study. Fifty patients with follow-up of more than 12 months were then retrospectively analyzed either by reviewing their medical records or by means of telephone interviews. The mean follow-up period was 42 months (range 12-82). The patient population consisted of 22 males and 28 females, with ages ranging from 27 to 83 years (mean 65. 8 years). Thirty-seven patients had pain on their right side. Twenty-three patients had more than one division affected; seven patients had V1 and V2 divisions, fourteen patients had pain on V2 and V3 divisions, and all three divisions were affected in remaining two patients. The projection of pain was most commonly seen in the second division (16 cases) followed by the third division (9 cases), and lastly the first division (2 cases). Seventeen patients had undergone the following procedures : previous peripheral block (5 cases), radiofrequency rhizotomy (4 cases), microvascular decompression (5 cases), glycerol rhizotomy (1 case), radiosurgery (1 case), and microvascular decompression and radiosurgery (1 case).
Facial axial CT using the orbitomeatal plane was performed preoperatively. We measured on the site of the preauricular landmark, that is, the zygomatic point in relation to external auditory meatus using CT5). The entire procedure was performed under general anesthesia with intratracheal intubation. The air space of a No. 4 Fogarty catheter was filled with radiographic contrast to check the patency of the balloon. The catheter was then inserted into the needle to a point marked on the shaft, to indicate when it reached the tip of the needle. The patient was placed in the neutral supine position. A portable imaging unit was positioned for a lateral view of the skull. Hartel guidelines were used for the needle insertion. The percutaneous puncture needle was directed at the zygomatic point on a plane with the zygomatic arch determined by a CT. Entry point on the cheek was 2.5 to 3.0 cm lateral to the corner of the mouth. On the lateral view of a C-arm fluoroscope, external of soft tissue was first punctured by a K wire needle. After the K wire entered the foramen ovale, a 14-gauge cannula was passed along the pathway of the K wire, the K wire was then removed and replaced with a blunt obturator replaced it. Penetration beyond the foramen margins was avoided with the 14-gauge needle. Then, the No.4 French Fogarty balloon catheter was inserted through the 14-gauge cannula until 10 to 17 mm of the catheter lay beyond the needle tip. The balloon catheter was inflated by slowly injecting 0.7-1.0ml of radio-opaque contrast using a 1 ml syringe. The shape and position of the balloon were checked with respect to neighboring bone landmarks; if not correct, the balloon was immediately deflated and the catheter was repositioned until a small nipple protruded into the posterior fossa through the porus trigemini. The duration of compression was between 60 and 120 seconds. We did not measure intraluminal balloon pressure. After compression, the balloon catheter and cannula were removed and the cheek was compressed for a few minutes. The patients were usually discharged the day following the procedure.
We used the chi-square test to investigate the outcome. Analysis of the results was performed using the statistical package for the social sciences software (SPSS) (Ver. 12.0; Inc, Chicago, IL). A p-value less than 0.01 was regarded as statistically significant.
RESULTS
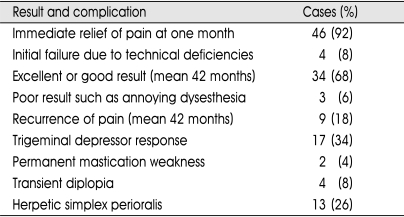
Complications and results are listed in Table 1. Outcomes are divided into five categories as follows: 1) "Excellent" denotes patients who are pain free, and off medication 2) "Good" denotes patients who are in occasional pain controlled with or without medication 3) "Poor" denotes patients complaining of severe dysesthesia, not adequately controlled with medication ; 4) "Failure"describes patients with no postsurgical pain relief within one month postoperatively; and 5) "Recurrence" indicates failure to control pain with the return of symptoms after a remission. It was possible to penetrate the foramen ovale and achieve balloon inflation in all patients. We reported an excellent result in 54% of the cases, good in 16%, poor result in 6%, 8% had initial failure due to technical deficiencies, 16% experienced recurrence with a mean follow-up period of 42 months. Forty-six cases (92%) were initially relieved of their pain. The mean time until recurrence was 18 months. Fifty patients underwent 58 procedures. Six patients required repeated procedure, two required one more, and four required two more. Five patients were initially relieved of their pain but annoying dysesthesia occurred in one case. The repeat procedure did not cause any additional technical difficulties. Two patients with recurrence received MVD. One patient with typical symptoms showed a good outcome. The other patient with annoying dysesthesia had a poor outcome with no apparent improvement at the other hospital. There were immediate, mild to moderate sensory complications of hypesthesia, dysesthesia and motor complication-difficulty of mastication in 94% of patients. The immediate motor and sensory complications gradually diminished and disappeared or were much improved after three months. Motor weakness of the masseter muscle was permanent in two patients with a dental prosthesis who complained of some malocclusion. Annoying dysesthesia occurred in three patients (6%). Two cases of annoying dysesthesia occurred with a pear-shaped balloon that was inflated for between 75 and 90 seconds. The other occurred with a one minute compression of a double-shaped balloon. Anesthesia dolorosa and loss of the corneal reflex did not occur in any patient. Four patients (8%) had transient diplopia that resolved within three months. Tri-geminal depressor response with hypotension and bradycardia or hypertension occurred in 34% of patients. Labial herpetic eruptions developed in 26% of cases. Most patients (92%) were discharged postoperatively within two days. The others were discharged within five days postoperatively.
Table 1.
Results and complications in 50 patients after percutaneous ballooing compression
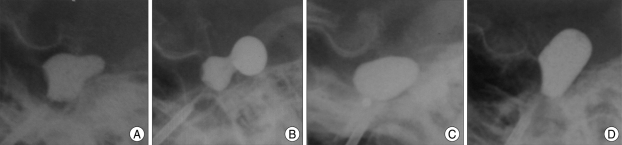
We obtained inflated balloons in four shape types that were pear, dumb-bell, oval, and cylindrical (Fig. 1). Table 2 shows results from analysis of the correlation between the different balloon shapes and resulting outcomes. The various balloon shapes did have statistically meaningful significance (p=0.00), the pear shape in particular had the most positive influence on excellent and good outcomes (28/33). In 75% of patients with initial failure the cylindrical type balloon was used (3/4) and the oval shape (1/9) was not as effective as expected (p=0.00). In view of the results so far achieved, we can state that there is a positive relationship between outcomes and shape of balloon judging from statistical values. Thus, patients having pear and dumb-bell type balloon shapes had a higher chance for excellent or good satisfaction of postoperative result and the oval shape was less effective in terms of satisfactory postoperative results.
Fig. 1.
The shape of ballooning. A, typical pear shape. B, dumb-bell shape. C, round or oval shape. D, cylindrical shape.
Table 2.
Incidence of balloon shape in lateral radiographs associated with clinical outcomes
DISCUSSION
The present retrospective analysis of a series of 50 PBCs with a mean follow-up period of 42 months contributes to our understanding of the outcome and complication rates associated with this treatment. Our procedure provided a satisfactory result in 70% of patients, poor result in 6%, 8% had technical deficiencies, 16% experienced recurrence. Neither anesthesia dolorosa nor keratitis occurred. In overall, these results are similar to those who have reported this to be a highly effective method of relieving trigeminal neuralgia6-8,10). Others have noted that 86% of patients were satisfactory with their pain relief with a mean follow-up of three years4). In one recent report, the recurrence rate was about 20% within five years and about 30% over ten years with an initial success rate of above 90%10).
All procedures share risk of complications and surgical results in these cases are related to needle placement, catheter location, balloon shape, and the compression time of the balloon6,7,10). Most of the surgical complications in this study, such as severe dysesthesia6), early failures7), and diplopia11) could be also related to avoidable technical errors. Unlike other percutaneous procedures, the needle should not pass through the foramen ovale4,9). The balloon also should reach the porus without going beyond the clival line9). When properly positioned at the Meckel's cave entrance, the balloon compresses the retrogasserian trigeminal nerve against the petrous bone and the firm medial edge of the dura, which will have a pear shape. It has been reported that the pear-shaped appearance is very predictive of success, but the ideal pear shape is not always attained. We observed four shapes in the inflated balloon : pear (66%), dumb-bell (8%), oval (18%), and cylindrical (4%). A pear shape was seen during compression in 74 % by Brown4). The catheter tip can enter the posterior fossa and inflate in a dumb-bell fashion, partly within the posterior fossa and partly within the cave7). Even if it this is done successfully the migration of the catheter into the posterior fossa is always a concern as is the fear, that, annoying dysestehsia may result from maximal compression of the retrogasserian fibers. To achieve optimum results, the catheter was withdrawn slightly or compression time was decreased for one minute. An oval shape may appear due to the large size of the cave, adhesion in the ganglion in adequate inflation of the balloon or a wrong position of the catheter tip1,6,7). A cylindrical shape can appear from the intradural placement of the catheter7). With oval or round cylindrical shapes, the balloon compresses the ganglion minimally. Subtemporal placement of the catheter is possible if it is positioned laterally to Meckel's cave. A cylindrical -shaped appearance is probably predictive of failure due to technical error. This could be avoided by using an anteroposterior image to lateralize the catheter placement3). A biplane imaging unit could be used instead of a portable monoplane unit to successfully enter the cave. Frameless stereotaxy using a navigating system is helpful for cannulation of the foramen ovale2). The catheter may have to be repositioned one or more times until the characteristic pear shape appears. It cannot be easily repositioned though if a pear shape is not obtained. After three weeks, the opening in the dura heals, and the procedure may be repeated4,9).
The optimal compression time was not firmly established, but we found that favorable results could be achieved with a range of 1-1.5 minutes compression time3,6,10). In our cases, the severe dysesthesia did not occurr following compression for one minute with the pear-shaped balloon. With the double balloon shape, however, one minute compression caused severe dysesthesia in 25% of cases. Severe dysesthesia did not occur with the oval and cylindrical-shaped balloon only after 90 seconds. This may be related to the fact that compression time or balloon shape is critical to the development of adverse annoying dysesthesia. Compression with duration longer than one minute with the pear-shaped balloon probably increased numbness and probably also increased the incidence risk of dysesthesia10). Although initial jaw weakness usually disappeared in a few months, it was permanent in 4 % of patients with a dental prosthesis linked with malocclusion in this study. That can be a particular problem for someone who already has chewing difficulties on the other side of the jaw such as temporomandibular joint problems.
Although there is a greater chance of jaw-muscle weakness, less selectivity by location, and a need for brief general anesthesia in contrast to other percutaneous procedures, corneal numbness and anesthesia dolorosa are very unlikely with balloon compression6,8,10). Compression is especially helpful for first-division pain and also useful for multidivisional pain3,10). The procedure itself is also painless for the patient. It can eliminate the risk of a small but definite incidence of serious complications of intracranial needle penetration which applies to other percutaneous procedures4,6). The procedure can be repeated for recurrence without greater technical difficulty7). All these factors make it an attractive choice in the treatment of trigeminal neuralgia.
CONCLUSION
We conclude that the balloon compression seems to be an effective method in the treatment of idiopathic trigeminal neuralgia with a low risk of causing severe hypesthesia or dysesthesia or corneal reflex impairment. Careful advancement of the needle and catheter with the help of anatomic landmarks and radiological guidance may minimize the risk of technical problems and postsurgical morbidity. We also emphasize that the surgeon should make every possible effort to obtain the pear-shaped balloon with one minute compression time for favorable results.
Acknowledgement
This work was presented as a oral presentation at the spring meeting of Korean Neurosurgical Society in 2007.
References
- 1.Ahn KS, Lee MK, Hwang SH, Lee JE, Cho CW, Kim DJ. Percutaneous Balloon Compression of Trigeminal Ganglion for the treatment of idiopathic Trigeminal Neuralgia. J Korean Neurosurg Soc. 2004;36:213–217. doi: 10.3340/jkns.2008.43.4.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bale RJ, Laimer I, Martin A, Schlarger A, Mayr C, Rieger M, et al. Frameless stereotactic cannulation of the foramen ovale for ablative treatment of trigeminal neuralgia. Neurosurgery. 2006;59:ONS394–ONS401. doi: 10.1227/01.NEU.0000232770.97616.D0. [DOI] [PubMed] [Google Scholar]
- 3.Brown JA. Percutaneous technique. In: Youmans JR, editor. Neurological Surgery. ed 5. Vol 3. New York: Saunders; 2004. pp. 2996–3004. [Google Scholar]
- 4.Brown JA. Trigeminal neuralgia-Percutaneous trigeminal nerve compression. In: Follett KA, editor. Neurosurgical Pain Management. Elsevier: Saunders; 2004. pp. 214–218. [Google Scholar]
- 5.Hwang SH, Lee MK, Park JW, Lee JE, Cho CW, Kim DJ. A morphometric analysis of the foramen ovale and the zygomatic points determined by a computed tomography in patients with idiopathic trigeminal neuralgia. J Korean Neurosurg Soc. 2005;38:202–205. [Google Scholar]
- 6.Lichtor T, Mullan JF. A 10-year follow-up review of percutaneous microcompression of the trigeminal ganglion. J Neurosurg. 1990;72:49–54. doi: 10.3171/jns.1990.72.1.0049. [DOI] [PubMed] [Google Scholar]
- 7.Lobata RD, Rivas JJ, Sarabia R, Lamas E. Percutaneous microcompression of the gasserian ganglion for trigeminal neuralgia. J Neurosurg. 1990;72:546–553. doi: 10.3171/jns.1990.72.4.0546. [DOI] [PubMed] [Google Scholar]
- 8.Lopez BC, Hamlyn PJ, Zakrzewska JM. Systemic review of ablative neurosurgical techniques for the treatment of trigeminal neuralgia. Neurosurgery. 2004;54:973–982. doi: 10.1227/01.neu.0000114867.98896.f0. discussion 982-983. [DOI] [PubMed] [Google Scholar]
- 9.Mullan S, Lichtor T. Percutaneous microcompression of the trigeminal ganglion for trigeminal neuralgia. J Neurosurg. 1983;59:1007–1012. doi: 10.3171/jns.1983.59.6.1007. [DOI] [PubMed] [Google Scholar]
- 10.Skirving DJ, Dan NG. A 20-year review of percutaneous balloon compression of the trigeminal ganglion. J Neurosurg. 2001;94:913–917. doi: 10.3171/jns.2001.94.6.0913. [DOI] [PubMed] [Google Scholar]
- 11.Urculo E, Alfaro R, Arrazola M, Astudillo E, Rejas G. Trochlear nerve palsy after repeated percutaneous balloon compression for recurrent trigeminal neuralgia : Case report and pathologenic considerations. Neurosurgery. 2004;54:505–508. doi: 10.1227/01.neu.0000103675.32713.a9. discussion 508-509. [DOI] [PubMed] [Google Scholar]