Abstract
We report a rare case of delayed cement displacement after balloon kyphoplasty in patient with Kümmell's desease. A 78-year-old woman with Kümmell's desease at T12 level received percutaneous balloon kyphoplasty. Two months after surgery, the patient complained of progressive severe back pain. Computed tomographic scans revealed a breakdown of the anterior cortex and anterior displacement of bone cement. Although this complication is very rare, it is likely to occur in treatment of Kümmell's desease accompanying anterior cortical defect.
Keywords: Kümmell's desease, Balloon kyphoplasty, Bone cement displacement
INTRODUCTION
Percutaneous vertebroplasty and balloon kyphoplasty are image-guided procedures, that involve the percutaneous injection of polymethylmethacrylate (PMMA) into a fractured vertebra. Both procedures have been shown to relieve pain with acceptable safety in patients with osteoporotic compression fractures and malignant tumors. In addition, these have been reported to effectively treat compression fractures with intravertebral vacuum clefts, as the pain and instability associated with intravertebral movement at the location of the clefts resolved after they were filled with cement3). Despite of its higher costs, balloon kyphoplasty has advantages of deformity correction and decreased PMMA extravasation. In addition to pain relief, balloon kyphoplasty affords the opportunity to improve sagittal balance and reduce the cement leaks over vertebroplasty7). But, it is not free of complications, and many of the complications of PMMA injection are directly related to cement leaks. We report a rare case of delayed cement displacement after balloon kyphoplasty in patient with Kümmell's disease. Knowledge of this complication and its pathophysiology are of seminal importance in ensuring that the necessary precautions are taken when using these procedures for the treatment of patients with Kümmell's disease and for improving the safety and efficacy of the procedures.
CASE REPORT
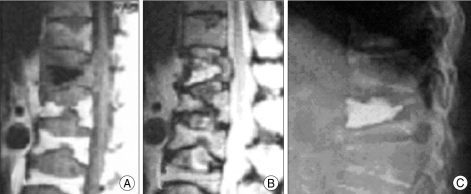
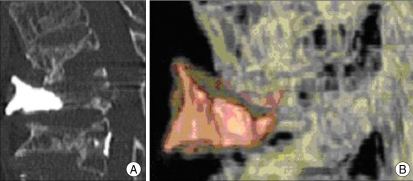
A 78-year-old woman suffered from persistent severe back pain since she slipped down 3 months before medical consult. The findings on neurologic examination were within normal limits. Magnetic resonance imaging (MRI) studies of the thoracolumbar spine revealed collapse of the vertebral body with formation of a cavitary lesion at T12 level. High signal on T2-weighted MRI revealed a fluid-filled intravertebral cleft. She had severe osteoporosis (T-score on bone marrow densitometry : -5.8) and there was no evidence of soft tissue mass or paravertebral abscess. Benign osteoporotic compression fracture with avascular necrosis was confirmed (Fig. 1A, B). Because of the intractable back pain, which had been unrelieved by conservative treatment, balloon kyphoplasty was performed. About 9.8 cc PMMA was injected into vacuum space of vertebral body. Postoperative roentgenographic image revealed that bone cement was well localized in the cystic cavity on T12 vertebral body (Fig. 1C). Two months after surgery, the patient complained of progressive severe back pain. Computed tomographic scans revealed a breakdown of the anterior cortex of the T12 vertebral body, with anterior displacement of the bone cement (Fig. 2).
Fig. 1.
Imaging studies obtained from a 78-year-old woman with T12 compression fracture. A, B : Sagittal T1-and T2-weighted images showing the fracture cavity as discrete areas of abnormally low and high signal intensity, respectively. C : Lateral radiograph of the spine in a weight-bearing position obtained immediately after balloon kyphoplasty reveals effective filling of cystic fracture cavity.
Fig. 2.
A, B : Two months after surgery, computed tomography scans reveals a breakdown of the anterior cortex with anterior displacement of bone cement.
DISCUSSION
Vertebral compression fractures due to osteoporosis increase with aging. Management of symptomatic osteoporotic vertebral compression fractures by vertebroplasty or kyphoplasty with PMMA has become increasingly popular7). Among them, balloon kyphoplasty is being increasingly adopted for the treatment of osteoporotic compression fracture. In addition to pain relief, kyphoplasty affords the opportunity to improve sagittal balance and reduce the extravasation rate by low pressure injection and increased viscosity during the injection11). Despite of these advantages, balloon kyphoplasty may result in several complications. Many of the complications of PMMA injection are mainly related to cement leaks. Cement extravasation during kyphoplasty ranges between 4% and 9%, a much lower incidence than with vertebroplasty7). However, because of the potential complications of cement in or around the spinal canal, and egress of cement outside the vertebral body is extremely concerning2). Often, collapsed vertebral bodies associated with osteoporosis have shown intravertebral vacuum clefts in the preprocedural evaluation5,6). However, recent studies have shown that these clefts are frequent and probably, represent fracture nonunion with dynamic mobility. In 1978, Maldague, et al.8) reported the presence of a vacuum cleft within vertebral fractures and suggested that this finding represented focal bone ischemia associated with nonhealing vertebral collapse. These clefts may be indicative of bone nonunion and can demonstrate the movement of the bone with changes in position or respiration10). The cleft or cavity must be completely filled with bone cement in order to treat these fractures adequately. In order to restore vertebral height and minimize the risk of direct cement extrusion into the canal through cortical defects or enlarged venous sinusoids, balloon kyphoplasty has been recommended. As experience with kyphoplasty has increases, it has become apparent that the intravertebral cavity created by the inflatable bone tamps allows placement of more viscous, partially cured PMMA. However, injection of viscous cement with low pressure decreases the penetration of the cement into the microstructure of cancellous bone1). Krause et al.4) reported that doughy cement on an unclean surface resulted in a very low interface strength compared to a low-viscosity cement made to penetrate a cleaned bone surface. Thermal necrosis of the surrounding tissue caused by the high polymerization temperature and the nonunion of fibrous tissue on the surface of the fractured cancellous bone disrupt the interdigitation of PMMA to achieve a mechanical interlock4,9). The current case showed a delayed post-traumatic vertebral collapse with intravertebral vacuum cleft which has long been considered as pathognomonic for avascular necrosis. Injection of PMMA into a cystic cavity would be expected to have far less interdigitation with the surrounding bone than would injection into partially intact trabecular bone9). Although, vertebroplasty is limited in its ability to restore kyphotic deformities and possibility of uncontrolled high-pressure injection, it may be more advantageous than balloon kyphoplasty because it can result in the formation of a compact trabecular pattern of opaque cement interspersed throughout the hollow trabecular space of the entire vertebral body in Kümmell's disease. However, because of the preexistent cleft, it is not necessary to use balloons to create a cavity because the patient already had a vacuum. Strict postoperative spinal bracing and the control of osteoporosis can be also helpful to prevent this delayed complication. The integrity of the anterior cortex is also important consideration of anterior displacement. The anterior cortex defect may increase the chance of anterior displacement of the cement under weight bearing.
CONCLUSION
Although a rare complication, the possibility of anterior displacement of PMMA after balloon kyphoplasty should be kept in mind as this complication may occur in treatment of Kümmell's disease.
References
- 1.Askew MJ, Steege JW, Lewis JL, Ranieri JR, Wixson RL. Effect of cement pressure and bone strength on polymethylmethacrylate fixation. J Orthop Res. 1984;1:412–420. doi: 10.1002/jor.1100010410. [DOI] [PubMed] [Google Scholar]
- 2.Greene DL, Isaac R, Neuwirth M, Bitan FD. The eggshell technique for prevention of cement leakage during kyphoplasty. J Spinal Disord Tech. 2007;20:229–232. doi: 10.1097/01.bsd.0000211276.76024.30. [DOI] [PubMed] [Google Scholar]
- 3.Kim DY, Lee SH, Jang JS, Chung SK, Lee HY. Intravertebral vacuum phenomenon in osteoporotic compression fracture : report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg. 2004;100(1 Suppl):24–31. doi: 10.3171/spi.2004.100.1.0024. [DOI] [PubMed] [Google Scholar]
- 4.Krause WR, Krug W, Miller J. Strength of the cement-bone interface. Clin Orthop Relat Res. 1982;163:290–299. [PubMed] [Google Scholar]
- 5.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft : a sign of ischemic vertebral collapse. Radiology. 1978;129:23–29. doi: 10.1148/129.1.23. [DOI] [PubMed] [Google Scholar]
- 6.Malghem J, Maldague B, Labaisse MA, Dooms G, Duprez T, Devogelaer JP, et al. Intravertebral vacuum cleft : changes in content after supine positioning. Radiology. 1993;187:483–487. doi: 10.1148/radiology.187.2.8475295. [DOI] [PubMed] [Google Scholar]
- 7.Mathis JM, Ortiz AO, Zoarski GH. Vertebroplasty versus kyphoplasty : a comparison and contrast. AJNR Am J Neuroradiol. 2004;25:840–845. [PMC free article] [PubMed] [Google Scholar]
- 8.McKiernan F, Faciszewski T. Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum. 2003;48:1414–1419. doi: 10.1002/art.10984. [DOI] [PubMed] [Google Scholar]
- 9.Tsai TT, Chen WJ, Lai PL, Chen LH, Niu CC, Fu TS, et al. Polymethylmethacrylate cement dislodgment following percutaneous vertebroplasty : a case report. Spine. 2003;28:E457–E460. doi: 10.1097/01.BRS.0000096668.54378.25. [DOI] [PubMed] [Google Scholar]
- 10.Van Eenenaam DP, el-Khoury GY. Delayed post-traumatic vertebral collapse (Kümmell's desease): case report with serial radiographs, computed tomographic scans, and bone scans. Spine. 1993;18:1236–1241. [PubMed] [Google Scholar]
- 11.Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine. 2005;30:2806–2812. doi: 10.1097/01.brs.0000190885.85675.a0. [DOI] [PubMed] [Google Scholar]