Abstract
Spontaneous spinal epidural hematoma (SSEH) is a relatively rare but significant spinal condition. Urgent surgical evacuation of a hematoma is generally indicated to prevent serious permanent neurological deficits. We encountered three cases of spontaneous spinal epidural hematomas associated with motor weakness that were treated successfully by surgical intervention.
Keywords: Spinal epidural hematana, Laminectomy
INTRODUCTION
Spontaneous spinal epidural hematoma (SSEH) is a relatively rare disease. Its incidence as estimated by Holtas et al was 0.1 per 100,000 people and less than 1% of people with the condition, the spinal epidural space was occupied by lesions3). The usual clinical presentation of SSEH is sudden neck or back pain that progresses toward paraparesis or quadriparesis, depending on the level of the lesion. Its etiology is related to coagulopathy, vascular malformation, neoplasms, infections, minor vertebral traumas and idiopathic causes. The authors encountered three cases of SSEH that were treated successfully through surgical intervention.
CASE REPORT
Case 1
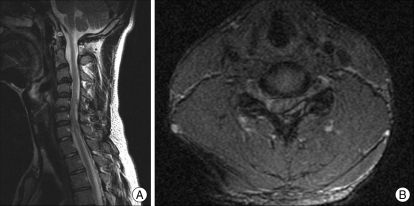
A 19-year-old man was admitted to the hospital because of posterior neck pain, left upper extremity sensory changes, and mild weakness that developed 4 hours prior to admission. He denied any past medical history or trauma. MRI of the cervical spine revealed a flat and oval shaped lesion in the dorsal and left lateral side of the epidural space from the C3 to C7 levels showing mildly high signal intensity on T1-weighted images and heterogeneous signal intensity on T2-weighted images (Fig. 1A). A definite signal change in the spinal cord was not seen on MRI (Fig. 1B). Spinal angiography was checked, but no vascular abnormality was observed. We could not find any abnormal laboratory data, such as coagulopathy or, infection.
Fig. 1.
Preoperative T2-weighted image shows an spontaneous spinal epidural hematoma located from C3 to C7 (A) and spinal cord compression on the dorsal and left lateral sides (B).
We performed partial hemilaminectomy of C3, 4, 5 and removed the epidural hematoma compressing the spinal cord. The patient was discharged without any further neurological problems.
Case 2
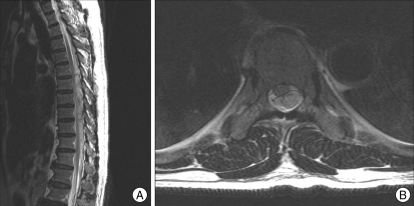
A 64-year-old man was admitted to the hospital because of low back pain and weakness in both legs (grade IV) that developed 2 hours prior to admission. He did not have a specific past medical history or trauma. No abnormal laboratory data were found. MRI of the thoracolumbar spine showed an elongated dorsal epidural mass lesion with slightly high signal intensity on T1-weighted images and heterogenous low signal intensity on T2-weighted images from T5 to L2 (Fig. 2A). The lesion displaced the spinal cord toward the right side (Fig. 2B). No definite vascular abnormalities were noted on spinal angiography.
Fig. 2.
Preoperative T2-weighted image shows an spontaneous spinal epidural hematoma located from T5 to L2 (A) and spinal cord compression on the dorsal and left lateral sides (B).
We performed a total laminectomy from T6 to T10 and could identify a dark brownish epidural hematoma compressing the spinal cord, which was then removed. He was discharged without any further neurological problems.
Case 3
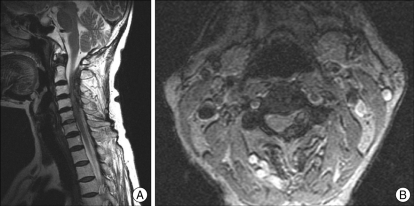
A 69-year-old woman was admitted to the hospital because of posterior neck pain and left upper extremity weakness (grade III) that developed 2 hours prior to admission. She had a history of hypertension and had taken aspirin for 5 years. Laboratory data and PT and, aPTT were in the normal range. An elongated spindle shaped lesion at the left dorsolateral epidural space of the upper cervical level was identified on cervical spine MRI (Fig. 3A). There was no definite signal change in the spinal cord on MRI even though the lesion displaced the spinal cord toward the right side (Fig. 3B).
Fig. 3.
Preoperative T2-weighted image showing an spontaneous spinal epidural hematoma located from C2 to C5 (A) and spinal cord compression on the dorsal and left lateral sides (B).
A partial hemilaminectomy of C2, 3, and 4 was performed. We identified an epidural hematoma compressing the spinal cord and removed it. Her left arm weakness improved from grade III to grade IV.
DISCUSSION
A spinal epidural hematoma is a rare but significant neurological condition. The spontaneous development of spinal epidural hematomas is most frequent after the fourth or fifth decade5). However, it has been reported to occur in all age groups, and it is a very rare clinical entity in children. Only 30 pediatric cases of SSEH have been documented in the medical literature10,15). The male/female ratio is 1.4 : 17). Certain precipitating factors, including anticoagulant therapy for prosthetic cardiac valves, therapeutic thrombolysis for acute myocardiac infarction, hemophilia B, factor XI deficiency, long-term aspirin using as a platelet aggregation inhibitor, and vascular malformation, are suggested to be correlated with spontaneous spinal epidural hematomas1,13). It is also a rare occurrence during pregnancy, with only six cases reported in the literature2). Statistically, idiopathic cases account for approximate 40% of all cases7). The most common site of a spontaneous spinal epidural hematoma is the cervicothoracic region or thoracolumbar region5,12).
Up to now, there have been disputes about the origin of these hematomas. Most researchers assert that SSEHs arise from the epidural venous plexus in the spinal epidural space because it lacks venous valves, and undulating pressure from the thoracic and abdominal cavities can impact it directly5,7,11). Several authors have prop-osed the spinal epidural arteries as a source of hemorrhage13). A more likely explanation is that pressure from arterial bleeding compresses the spinal cord, because the intra-thecal pressure is higher than the venous pressure5,9).
The usual clinical presentation of a spontaneous spinal epidural hematoma is sudden stabbing neck or back pain that progresses toward paraparesis or quadriparesis, depending on the level of the lesion and the nerve root6). Children often suffer from additional symptoms of irritability, and occasionally urinary retention10). In high cervical region, SSEHs could cause spinal shock, leading to fatal condition3).
Currently, MRI is considered as the first choice diagnostic method for SSEH8,8,14). It typically shows biconvex hematomas in the epidural space with welldefined borders tapering superiorly and inferiorly4). Subacute hematomas show characteristic high signal intensity on T1-weighted images4). A CT scan should be obtained if MRI is unavailable11).
The differential diagnosis of spontaneous spinal epidural hematoma includes an acute herniated intervertebral disc, acute ischemia of the spinal cord, epidural tumor or abscess, spondylitis, transverse myelitis, or even a dissecting aortic aneurysm and acute myocardial infarction.
Early surgical intervention is the general treatment for spontaneous spinal epidural hematomas8). The procedure includes decompressive laminectomy and hematoma removal. If the exact location of the hematoma cannot be detected and confirmed by MRI, the dura should be opened to exclude the subdural hematoma. In cases with incomplete neurological deficits, the operation should be performed within 48 hours of the onset of the initial symptoms7). If the initial neurological deficits are complete, the operation should be performed within 36 hours7). Conservative treatment has also been documented, and it was employed only when neurological deficits improved in the early phase or with the coexistence of coagulopathy15). Multilevel acute epidural hematomas may be difficult to treat operatively in patients with coagulopathy16). Although the functional recovery of these patients may not be complete, the SSEH can be treated without surgery, and the patient should be protected from the significant risk of surgical intervention15).
CONCLUSION
We report three rare cases of spontaneous spinal epidural hematomas. For the treatment of SSEHs, operation should be considered as soon as possible unless the neurological deficit takes a favorable turn in the earlier period or the patient also has coagulopathy.
References
- 1.Bisson EF, Dumont T, Tranmer B. Spontaneous Spinal Epidural Hematoma in a Child with Hemophilia B. Can J Neurol Sci. 2007;34:488–490. doi: 10.1017/s0317167100007423. [DOI] [PubMed] [Google Scholar]
- 2.Bose S, Ali Z, Rath GP, Prabhakar H. Spontaneous spinal epidural hematoma : a rare cause of quadriplegia in the post-partum period. Br J Anaesth. 2007;99:855–857. doi: 10.1093/bja/aem265. [DOI] [PubMed] [Google Scholar]
- 3.Chan DT, Boet R, Poon WS, Yap F, Chan YL. Spinal shock in spontaneous cervical spinal epidural haematoma. Acta Neurochir(Wien) 2004;146:161–1162. doi: 10.1007/s00701-004-0347-8. discussion 1162-1163. [DOI] [PubMed] [Google Scholar]
- 4.Fujiwara H, Oki K, Momoshima S, Kuribayashi S. PROPELLER diffusion-weighted magnetic resonanace imaging of acute spinal epidural hematoma. Acta Radiol. 2005;46:539–542. doi: 10.1080/02841850510021553. [DOI] [PubMed] [Google Scholar]
- 5.Guzel A, Simsek O, Karasalihoglu S, Kucukugurluoglu Y, Acunas B, Tosun A, et al. Spontaneous spinal epidural hematoma after seizure : a case report. Clin Pediatr (Phila) 2007;46:263–265. doi: 10.1177/0009922806289427. [DOI] [PubMed] [Google Scholar]
- 6.Hangping Y, Shunwu F, Huilin Y, Tiansi T, Feng Z, Xing Z. Early diagnosis and treatment of acute or subacute spinal epidural hematoma. Chin Med J. 2007;120:1303–1308. [PubMed] [Google Scholar]
- 7.Liu Z, Jiao Q, Xu J, Wang X, Li S, You C. Spontaneous spinal epidural hematoma:analysis of 23 cases. Surg Neurol. 2008;69:253–260. doi: 10.1016/j.surneu.2007.02.019. discussion 260. [DOI] [PubMed] [Google Scholar]
- 8.Matsumura A, Namikawa T, Hashimoto R, Okamoto T, Yanagida I, Hoshi M, et al. Clinical management for spontaneous epidural hematoma : diagnosis and treatment. Spine J. 2007;8:534–537. doi: 10.1016/j.spinee.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Park J, Lee JB, Park JY, Lim DJ, Kim SD, Chung YK. Spinal cord infarction after decompressive laminectomy for spontaneous spinal epidural hematoma. Neurol Med Chir(Tokyo) 2007;47:325–327. doi: 10.2176/nmc.47.325. [DOI] [PubMed] [Google Scholar]
- 10.Poonai N, Rieder MJ, Ranger A. Spontaneous spinal epidural hematoma in an 11-month-old girl. Pediatr Neurosurg. 2007;43:121–124. doi: 10.1159/000098385. [DOI] [PubMed] [Google Scholar]
- 11.Riaz S, Jiang H, Fox R, Lavoie M, Mahood JK. Spontaneous spinal epidural hematoma causing Brown-Sequard syndrome : case report and review of the literature. J Emerg Med. 2007;33:241–244. doi: 10.1016/j.jemermed.2007.02.032. [DOI] [PubMed] [Google Scholar]
- 12.Shin JJ, Kuh SU, Cho YE. Surgical management of spontaneous spinal epidural hematoma. Eur spine J. 2006;15:998–1004. doi: 10.1007/s00586-005-0965-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solheim O, Jorgensen JV, Nygaard OP. Lumbar epidural hematoma after chiropractic manipulation for lower back pain : Case Report. Neurosurgery. 2007;61:E170–E171. doi: 10.1227/01.neu.0000279740.61048.e2. discussion E171. [DOI] [PubMed] [Google Scholar]
- 14.Song KJ, Lee KB. The poor outcome of the delayed diagnosis of acute spontaneous spinal epidural hematoma : two cases report. J Korean Med Sci. 2005;20:331–334. doi: 10.3346/jkms.2005.20.2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tailor J, Dunn IF, Smith E. Conservative treatment of spontaneous spinal epidural hematoma associated with oral anticoagulant therapy in a child. Childs Nerv Syst. 2006;22:1643–1645. doi: 10.1007/s00381-006-0220-6. [DOI] [PubMed] [Google Scholar]
- 16.Ziyal IM, Aydin S, Inci S, Sahn A, Ozagen T. Multilevel acute spinal epidural hematoma in a patient with chronic renal failure- case repor. Neurol Med Chir (Tokyo) 2003;43:409–412. doi: 10.2176/nmc.43.409. [DOI] [PubMed] [Google Scholar]