Abstract
Objective
The purpose of this study was to introduce our surgical experiences of scoliosis and to evaluate the effectiveness of anterior correction and fusion in adolescent idiopathic scoliosis (AIS).
Methods
Between August 2004 and August 2007, four patients with AIS were treated with anterior segmental fusion and fixation at our hospital. Mean follow-up period was 9 (6-12) months. The average age was 14.0 (13-15) years. According to Lenke classification, three patients showed Lenke 1 curve and one patient with Lenke 5 curve. Single rod instrumentation was performed in one patient, dual rod instrumentation in one patient and combined rod instrumentation in two patients. Coronal Cobb measurements were performed on all curves in thoracic, thoracolumbar and, lumbar spine and the angle of hump was measured by a scoliometer pre- and postoperatively.
Results
The average operative time was 394 minutes (255-525) with an average intraoperative blood loss of 1,225 ml (1,000-1,700). The mean period of hospital stay was 19.3 days and there was no complication related to the surgery. The mean Cobb angle was reduced from 43.3° to 14.8° (65.8% correction) postoperatively and the rib hump corrected less than 5°. All patients and their parents were satisfied with the deformity correction.
Conclusion
Anterior spinal correction and fusion of AIS with Lenke 1 and 5 curve showed excellent deformity correction without any complications. In particular, we recommend anterior dual rod instrumentation because of mechanical stability, better control of kyphosis, and a higher fusion rate.
Keywords: Adolescent idiopathic scoliosis, Anterior correction and fusion, Rod instrumentation
INTRODUCTION
Adolescent idiopathic scoliosis (AIS) is the most common type of scoliosis occupying approximately 50% of all scoliosis6). The incidence of AIS has been reported from 3.7 to 0.08% of general population according to screening test and radiographic studies6,13). However, AIS that needs surgical treatment is relatively rare in Korean people compared to Caucasian and still an unfamiliar disease entity for Korean neurosurgeon even though surgical trials for the territory of deformity are being done.
A variety of surgical approaches for AIS have been introduced anteriorly or posteriorly. Recently, anterior correction with instrumentation is known to have specific advantages, such as an easy correction and short segment fusion levels, in some types of AIS.
The main purpose of this study was to introduce the surgical experiences and to evaluate the effectiveness of short segment anterior correction in AIS. Emphasizing the role of neurosurgeon to expand the surgical horizon into the deformity surgery area was another additional purpose of this study.
MATERIALS AND METHODS
Between August 2004 and August 2007, four patients with AIS were treated with anterior segmental fusion and fixation at our hospital. Mean follow-up period was 9 (6-12) months. All patients were female. The average age was 14.0 (13-15) years. According to Lenke classification, three patients showed Lenke 1 curve (single thoracic curve) and one patient had Lenke 5 curve (thoracolumbar scoliosis)11). Standing posteroanterior and lateral radiographs of the entire spine were taken pre- and postoperatively for measurement of scoliosis in all patients. Supine lateral bending films were taken to check the change and flexibility of major and compensatory curves. Magnetic resonance image and 3-dimensional computed tomography were taken for the evaluation of the vertebral structure, the alignment, and the degree of rotation. Pulmonary function test was done for thoracotomy operation in all patients.
The degree of deformity was evaluated using coronal Cobb angle, thoracic kyphosis, major spinal rotation and severity of rib hump elevation3,17,19). Bone maturation was estimated using Risser grade18). Coronal Cobb angle was measured on all curves in thoracic, thoracolumbar and, lumbar spine and the angle of hump was measured by a scoliometer pre- and postoperatively.
Surgical technique
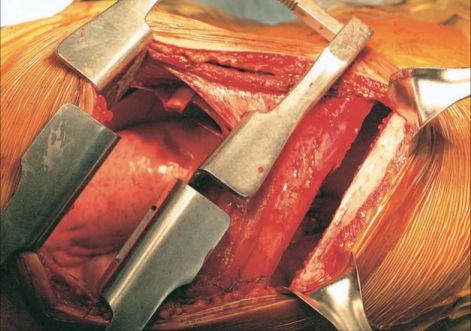
The surgical position was lateral decutibus position maintaining the apex of curve up and right side up in all the patients. An anterior transthoracic approach was used with the rib resection corresponding to the proximal level of the thoracic fusion. In case of one thoracolumbar scoliosis, diaphragmatic incision was performed for combined retroperitoneal approach. In one patient whose seven thoracic levels were fused, a single skin incision with double thoracotomy approach was used for access to all thoracic levels to be instrumented and fused (Fig. 1). The segmental vessels were isolated and ligated on the anterolateral aspect of vertebral bodies. Complete annulectomy and discectomy were performed at each vertebral level to be fused and instrumented. Monoaxial screws were placed bicortically at all levels to be included in the fusion. Intervertebral bone grafting was carried out using resected rib fragments. A rod with appropriate length was contoured into the desired coronal and sagittal alignment. The rod was engaged in all of the screws, and locking plugs were loosely applied. The rod was rotated and compressed until the appropriate coronal and sagittal alignment were achieved. When the rod rotation was completed, the apical screw was tightened, and intersegmental compression was applied beginning at the apex and progressing toward the ends. For dual rod fixation, secondary rod was applied after main correction using first rod. Intraoperative radiographs were obtained before wound closure. A complete closure of parietal pleura and diaphragm were performed before the insertion of chest tube drains. The patients were closely observed postoperatively at the intensive care unit for one day. All patients put on a thoracolumbosacral orthosis (TLSO) for 3 months. Standing posteroanterior and lateral radiographs were taken 1, 3, 6, and 12 months after surgery.
Fig. 1.
A single skin incision with double thoracotomy approach.
RESULTS
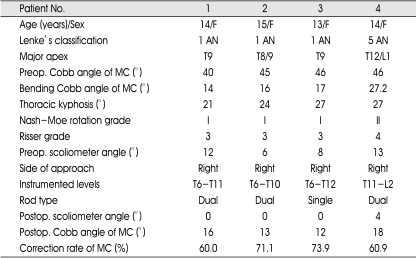
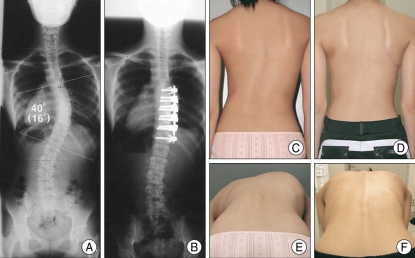
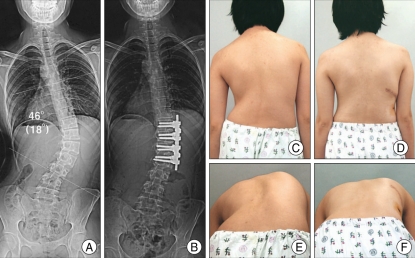
Demographic characteristics of all patients are described in Table 1. In three patients with Lenke type 1 curve, the apex of curve was the disc at T8/9 or the vertebral body at T9. The mean coronal Cobb angle of the main thoracic curve was 43.7° and the Cobb angles of the compensatory curves on thoracolumbar or lumbar region were less than 20°. On scoliometer measurement of the rib hump averaged 18.5°. On the lateral bending film the mean Cobb angle of main thoracic curve was corrected to 15.7° (Fig. 2). In one patient with Lenke type 5, the apex of curve was the disc T12/L1. The Cobb angle was 46.0° and the angle of the rib hump was 13.0°. On the lateral bending film the Cobb angle of main thoracolumbar curve was corrected to 18.0° (Fig. 3). Bone maturation evaluated using Risser grade showed about grade 3-4.
Table 1.
Demographic characteristics of patients
No : number, F : female, MC : main curve
Fig. 2.
A 14-years old female with Lenke type 1AN curve (patient No.1). A : Preoperative coronal Cobb angle (T6-T12) was 40° for thoracic curve. B : Anterior dual rod instrumentation from T6-T11 was performed and Cobb angle was corrected to 16°. C, D : Preoperative and postoperative upright clinical photographs show the marked improvement in the preoperative trunk shift after anterior correction. E, F : Preoperative and postoperative forward bending photographs show the complete correction of the rib hump after anterior correction.
Fig. 3.
A 14-years old female with Lenke type 5AN curve (patient No. 4). A. Preoperative coronal Cobb angle (T7-L3) was 46° for thoracolumbar curve. B. Anterior dual rod instrumentation from T11-L2 was performed and Cobb angle was corrected to 18°. C, D. Preoperative and postoperative upright clinical photographs show the marked improvement in the preoperative trunk shift after anterior correction. E, F. Preoperative and postoperative forward bending photographs show the satisfactory correction of the rib hump after anterior correction.
For the decision of fusion level, transitional and neutral vertebrae around the apex as well as surgical feasibility were considered. First of all, upper and lower end of rod was reached to the neutral vertebrae. Therefore, from 5 to 7 vertebrae were used for anterior fixation. Single or dual rods were used in one or three patients, respectively. In dual rods fixation, only one screw was fixed at the both end of fusion level and screw fixation became much easier through limited thoracotomy opening
The average operative time was 394 min (255-525) with an average intraoperative blood loss of 1,225 ml (1,000-1,700). Chest tube insertion was kept for about 10 days after surgery and removed when the daily amount of fluid discharge was below 100 ml for two consecutive days. The mean periods of hospital stay was 19.3 days and there was no complication related to the surgery. TLSO brace was applied for 3 months after surgery.
The mean Cobb angle of major curve was reduced from 43.3° to 14.8° (65.8% correction) postoperatively and the rib hump corrected less than 5°. All patients and their parents were satisfied with the deformity correction.
DISCUSSION
Scoliosis is defined as lateral deviation of the spinal column, minimum Cobb angle 10° with concordant vertebral rotation. One of the most popular categories, idiopathic scoliosis (no associated abnormalities and diseases) is subdivided by age at onset: infantile, juvenile, adolescent. Among them, AIS is the most common subtype of scoliosis. AIS itself is not a rare disease but shows relatively lower incidence in Korean people than Caucasian.
The aim of spinal surgery for AIS is to make a spine that is balanced in both sagittal and coronal planes and that has an appearance acceptable to the patients and their families. However, scoliosis surgery is not to make a beautiful X-ray image, but to make a functional improvement such as the prevention of cardiopulmonary dysfunction and deformity progression. In scoliosis surgery, the approach can be divided into anterior or posterior. Classically, posterior instrumentation and fusion represents the gold standard in the treatment of AIS. However, selective anterior fusion technique can be used in AIS with Lenke type 1 (main thoracic curves) and 5 curve (thoracolumbar/lumbar curves). In the late 1960s, Dwyer first developed anterior spinal instrumentation consisted of the cable and screw system and used it for myelomeningocele scoliosis5). In spite of good correction of scoliosis, the system was kyphogenic and had a high failure rate5). In the mid 1970s, Zielke developed an anterior rod-screw system and used if for idiopathic thoracolumbar and lumbar scoliosis. However, in Zielke system, high rate of kyphosis and rod breakage were reported due to lack of structural stiffness7,21). Since Turi et al. developed the first solid rod-screw anterior system and treated thoracolumbar idiopathic scoliosis in the early 1990s, there have been reports in the literature indicating good results of anterior instrumentation and fusion in terms of a better three-dimensional curve correction and a short segment fusion with preservation of spinal motion9,10,12,14,16,20).
In posterior scoliosis surgery, standard principle is that the fusion level should include beyond the transitional vertebrae and long segment fusion can not be inevitable. One of serious complications associated with long posterior fusion is progressive increase in rotational deformity of the spine after posterior fusion in skeletally immature patients (Crankshaft phenomenon)4). Short segment fusion reaching the neutral vertebrae is enough for the anterior surgery. Moreover, the curve correction during the anterior surgery is easier than posterior correction because derotating and compressing forces can be applied directly to the major curve composed of vertebral bodies. Intervertebral body fusion shows higher fusion rate than posterior fusion14). During short segment fusion hyperkyphosis can be prevented by derotation of the bent rod2. In our series, we used only 5-7 vertebral body fixations to get an acceptable major curve correction. We did not have any surgery-associated wound problem. Usually, anterior spine surgery shows low incidence of postoperative wound infection rate. Surgeon can avoid postoperative pulmonary complication by preoperative pulmonary function test. To obtain the best results from short anterior correction, we think surgeons should consider the balance between spine function and correction and shoulder balance after operation. Limitations of short segment anterior correction are double structured curves excluding Lenke type 1 and 5 curve, a large curve over 60 degree, and sometimes in long structural curve.
The studies of single rod surgery compared with dual rods have reported that the use of double rods than single rod is recommended8). The Harms Spine Study Group began using a single solid rod anterior system for AIS in mid 1990s1 and Kaneda et al. developed a dual-rod dual screw anterior system10). Currently, both systems are being used and there is no specific agreement as to the indication for single versus double rod system. Good radiographic and clinical outcomes have been reported in both studies for single and double rod system9,10,12,14). However, dual rod is stiffer and shows lower pseudoarthrosis or intraoperative screw pull-out than single rod8,9). In addition, anterior single rod instrumentation is contraindicated for a hypokyphotic thoracic spine8,15). We prefer dual rod instrumentation due to biomechanical stability. For surgery with single rod, larger diameter is recommended and careful attention should be paid on bicortical purchase of screws14). In our series, there was no pulmonary complication, pseudoarthrodesis/implant failures, or postoperative hyperkyphosis and good clinical result was obtained in all patients.
For anterior surgery, thoracotomy is needed to fix the screws and to apply rods. Not uncommonly, the size of wound opening is not adequate to insert the screws into upper and lower end vertebrae of major curve. In one patient of our series, we used double thoracotomy under single skin incision, and each thoracotomy should be located at both upper and lower sides of the curve. With a limited wound opening, surgery with dual rods is more complicated than single rod, which needs more surgical time and wider opening. To overcome this problem, we used another method of single screw at both ends of the fusion levels. In two patients we performed modified method of dual rods instrumentation around apex combined with distal single rod and obtained excellent results (Fig. 4). The main force of deformed curve has effect around the apex, and we believe that single screw at the end of curve is enough to maintain the corrected spinal column.
Fig. 4.

A modified dual rod instrumentation combined with dual rod around apex and distal single rod.
Our study was performed in only four cases; further data may be needed through additional surgeries of AIS. However, we emphasize an importance of study is that this is a first report in Korean neurosurgical spine surgery about anterior surgical treatment of AIS. Korean neurosurgeons have been doing a lot of spine surgeries with profound and enough accumulation of clinical and basic experiences. To expand the horizon of spinal deformity surgery in neurosurgical field, neurosurgeons should recognize that a fundamental understanding of spinal deformity is a basic requirement and should consistently try to expand the clinical experiences.
CONCLUSION
Anterior spinal correction of AIS with Lenke 1 and 5 curves enabled excellent deformity correction without any complication. In particular, we recommend anterior dual rod instrumentation because of mechanical stability, better control of kyphosis, and a higher fusion rate. This study is the first report in Korean neurosurgical spine surgery about anterior surgery of AIS. We hope, in the future, more attempts with much enthusiasm to expand the horizon of the field of scoliosis surgery will be made by Korean neurosurgeons.
References
- 1.Betz RR, Harms J, Clements DH, Lenke LG, Lowe TG, Shufflebarger HL, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine. 1999;24:225–239. doi: 10.1097/00007632-199902010-00007. [DOI] [PubMed] [Google Scholar]
- 2.Bitan FD, Neuwirth MG, Kuflik PL, Casden A, Bloom N, Siddiqui S. The use of short and rigid anterior instrumentation in the treatment of idiopathic thoracolumbar scoliosis: a retrospective review of 24 cases. Spine. 2002;27:1553–1557. doi: 10.1097/00007632-200207150-00014. [DOI] [PubMed] [Google Scholar]
- 3.Bunnell WP. The natural history of idiopathic scoliosis before skeletal maturity. Spine. 1986;11:773–776. doi: 10.1097/00007632-198610000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Dubousset J, Herring JA, Shufflebarger H. The crankshaft phenomenon. J Pediatr Orthop. 1989;9:541–550. doi: 10.1097/01241398-198909010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Dwyer AF, Newton NC, Sherwood AA. An anterior approach to scoliosis. A preliminary report. Clin Orthop Relat Res. 1969;62:192–202. [PubMed] [Google Scholar]
- 6.Goldberg CJ, Moore DP, Fogarty EE, Dowling FE. Scoliosis: a review. Pediatr Surg Int. 2007;24:129–144. doi: 10.1007/s00383-007-2016-5. [DOI] [PubMed] [Google Scholar]
- 7.Horton WC, Holt RT, Johnson JR, Leatherman KD. Zielke instrumentation in idiopathic scoliosis : late effects and minimizing complications. Spine. 1988;13:1145–1149. doi: 10.1097/00007632-198810000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Hurford RK, Jr, Lenke LG, Lee SS, Cheng I, Sides B, Bridwell KH. Prospective radiographic and clinical outcomes of dual-rod instrumented anterior spinal fusion in adolescent idiopathic scoliosis : comparison with single-rod constructs. Spine. 2006;31:2322–2328. doi: 10.1097/01.brs.0000238966.75175.2b. [DOI] [PubMed] [Google Scholar]
- 9.Kaneda K, Shono Y, Satoh S, Abumi K. Anterior correction of thoracic scoliosis with Kaneda anterior spinal system. A preliminary report. Spine. 1997;22:1358–1368. doi: 10.1097/00007632-199706150-00015. [DOI] [PubMed] [Google Scholar]
- 10.Kaneda K, Shono Y, Satoh S, Abumi K. New anterior instrumentation for the management of thoracolumbar and lumbar scoliosis. Application of the Kaneda two-rod system. Spine. 1996;21:1250–1261. doi: 10.1097/00007632-199605150-00021. discussion 1261-1262. [DOI] [PubMed] [Google Scholar]
- 11.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis : a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83:1169–1181. [PubMed] [Google Scholar]
- 12.Liljenqvist UR, Bullmann V, Schulte TL, Hackenberg L, Halm HF. Anterior dual rod instrumentation in idiopathic thoracic scoliosis. Eur Spine J. 2006;15:1118–1127. doi: 10.1007/s00586-005-0020-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lonstein JE, Bjorklund S, Wanninger MH, Nelson RP. Voluntary school screening for scoliosis in Minnesota. J Bone Joint Surg Am. 1982;64:481–488. [PubMed] [Google Scholar]
- 14.Lowe TG, Alongi PR, Smith DA, O'Brien MF, Mitchell SL, Pinteric RJ. Anterior single rod instrumentation for thoracolumbar adolescent idiopathic scoliosis with and without the use of structural interbody support. Spine. 2003;28:2232–2241. doi: 10.1097/01.BRS.0000085028.70985.39. discussion 2241-2242. [DOI] [PubMed] [Google Scholar]
- 15.Lowe TG, Enguidanos ST, Smith DA, Hashim S, Eule JM, O'Brien MF, et al. Single-rod versus dual-rod anterior instrumentation for idiopathic scoliosis : a biomechanical study. Spine. 2005;30:311–317. doi: 10.1097/01.brs.0000152376.09501.ae. [DOI] [PubMed] [Google Scholar]
- 16.Min K, Hahn F, Ziebarth K. Short anterior correction of the thoracolumbar/lumbar curve in King 1 idiopathic scoliosis : the behaviour of the instrumented and non-instrumented curves and the trunk balance. Eur Spine J. 2007;16:65–72. doi: 10.1007/s00586-006-0075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nash CL, Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969;51:223–229. [PubMed] [Google Scholar]
- 18.Risser JC. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111–119. [PubMed] [Google Scholar]
- 19.Stokes IA. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine. 1994;19:236–248. [PubMed] [Google Scholar]
- 20.Sweet FA, Lenke LG, Bridwell KH, Blanke KM, Whorton J. Prospective radiographic and clinical outcomes and complications of single solid rod instrumented anterior spinal fusion in adolescent idiopathic scoliosis. Spine. 2001;26:1956–1965. doi: 10.1097/00007632-200109150-00005. [DOI] [PubMed] [Google Scholar]
- 21.Zielke K, Berthet A. VDS-ventral derotation spondylodesis-preliminary report on 58 cases. Beitr Orthop Traumatol. 1978;25:85–103. [PubMed] [Google Scholar]