Abstract
Sacral insufficiency fractures are usually known to develop in elderly patients with osteoporosis without definite trauma history. It is difficult to diagnose the sacral insufficiency fracture at an early stage because lower lumbar diseases, concurrently or not, may also be presented with similar symptoms and signs. We report a rare case of sacral insufficiency fracture who was not diagnosed initially but, instead, showed progressively worsening of clinical symptoms and radiological findings after decompression surgery for upper level lumbar stenosis.
Keywords: Sacrum, Insufficiency fracture
INTRODUCTION
Sacral insufficiency fractures are usually overlooked in the elderly and other risk group of structurally weakened bone with low back and pelvic pain following no or trivial trauma10,19). They are difficult to diagnose at an early stage since there is usually no significant history of trauma, often accompanied by concurrent lower lumbar degenerative pathology, and routine radiographs of the sacrum do not demonstrate them adequately15). The precise incidence of the sacral insufficiency fracture is unknown. However, the potential prevalence of sacral insufficiency fracture is considered to be higher than the widely appreciated and sacral insufficiency fractures are remained largely overlooked causes of pain and disability within the elderly and other risk population19,21).
CASE REPORT
A 69-year old man was transferred to our clinics with a history of sudden lumbosacral back pain, radiating pain to the left leg and motor weakness of both legs since one month prior to admission. Conservative treatment was tried at the local clinics for several weeks, but there was no symptomatic improvement. On physical examination, the patient showed chronically ill-looking appearance and muscle atrophy of both legs. On neurological examination, mild hypesthesia on 4th and 5th lumbar roots territory and motor weakness (grade IV on manual muscle test) of the both legs were seen. The patient's past medical history included a total left knee replacement arthroplasty 3 years ago and the surgery for osteomyelitis of the right ankle along with total right knee replacement arthroplasty one year ago. Because of his medical conditions in the past, both long-term bed rest and medication were necessary. Laboratory examinations showed normal CRP and ESR/cESR . The results of all other routine hematological and electrolyte investigations were normal, including hemoglobin, platelet, leukocyte counts and electrolytes balance. The tests for ANA and RA factors showed negative findings. Routine plain radiographs showed degenerative changes at the lower lumbar and lumbosacral level, but did not show definite evidence of sacral insufficiency fracture (Fig. 1A). T-score of the lower lumbar spine was -4.0 on bone densitometry. Magnetic resonance imaging showed severe stenosis at the L4-5 canal (Fig. 1B) in which we performed decompressive surgery. Postoperatively, severe lumbosacral pain and tenderness remained and the patient could not stand and walk although radicular pain was improved markedly. Postoperative sacral cone lateral imaging showed discontinuity of the sacral cortex and displacement of the upper sacral segment (Fig. 2A). We suspected that these findings were related to the remaining symptom and sign. Thus, follow-up MRI, 3-dimentional CT and bone scan were done. MRI images demonstrated low signal intensity of the sacrum and sacroiliac joints (Fig. 2B, C). Three-dimentional CT scan delineated the fracture lines in the regions corresponding to low signal bands seen with MRI (Fig. 3). Bone scan showed increased activity within sacral ala and body demonstrating classical H" pattern of insufficiency fracture of the sacrum (Fig. 4). Absolute bed rest for a month was necessary along with medication including analgesics, calcium supplement and alendronate sodium, followed by physical therapy and rehabilitation program. Clinical outcome showed gradual pain relief and recovery of lower extremity neurologic signs over a 6-months period.
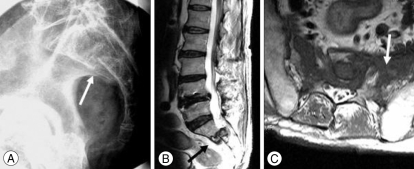
Fig. 1.
Routine study of the lumbar spine (A) does not show definite evidence of sacral insufficiency fracture. Preoperative magnetic resonance image (B) showing severe L4-5 canal stenosis with root compression (black arrow) and trivial signal changes at the interspace of upper sacrum (white arrow).
Fig. 2.
Postoperative cone view of the sacrum shows definite and aggravated fracture and displacement of the sacrum (A-arrow). Postoperative magnetic resonance imaging of the sacrum demonstrating aggravation of fracture and dislocation at the S1-S2 interspace (B-black arrow) and diffuse signal change at the sacral body and both sacral ala (C-white arrow).
Fig. 3.
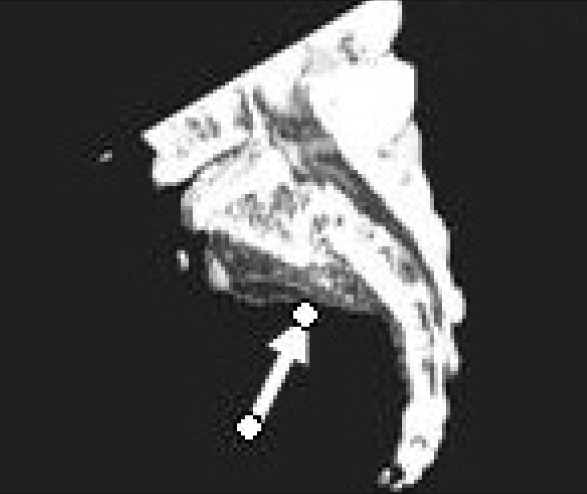
Computed tomography of the sacrum demonstrating the interruption of the both sacral cortex and displacement of the upper sacral body.
Fig. 4.
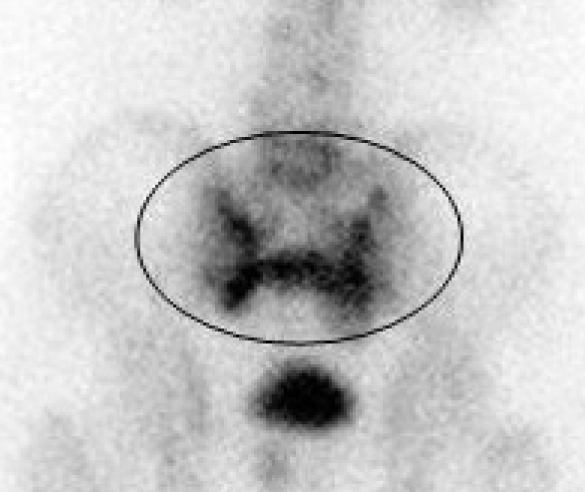
Bone scan of the pelvis. Increased uptake in both sacral ala and body of the sacrum, showing an classical H- or butterfly-shaped appearence ("H" sign, in circle).
DISCUSSION
Repetitive, prolonged muscular action on bone that has not accommodated itself to the action results in stress fractures. Stress fractures are classified into two categories, fatigue and insufficiency fractures5,16). While fatigue fractures are caused by abnormal stresses applied to normal bone itself, insufficiency fractures are developed by the effects of normal or physiologic stresses on weakened bone with decreased elastic resistance16).
Sacral insufficiency fractures have been first described as "spontaneous osteoporotic fracture of the sacrum" by Lourie in 1982. Though several case reports and small case series have been published12,19), the precise incidence of sacral insufficiency fractures remains unknown. In a prospective study for 2 years by Weber et al, incidence in women aged over 55 years who were presented to hospital with low back pain was 1.8%21). In reality, the sacral insufficiency fractures may be more common than the usually expected because of diagnostic difficulties and vague clinical symptom and signs1). It may represent commonly overlooked causes of low back pain primarily occuring in the elderly women with osteoporosis as a result of normal stress on abnormally weak bone17,19). Several pathological conditions may decrease bone resistance and predispose the development of insufficiency fractures. Among them, postmenopausal osteoporosis seem to be the most commonly associated condition9,19). Other conditions including corticosteroid induced osteopenia, radiation therapy, rheumatoid arthritis, paget's disease, osteomalacia, longstanding bed rest, hyperaldosteronism are common causes of the sacral insufficiency fractures10,14-16,19). In our patient, long-term immobilization and medications including steroid for treatment of the several orthopedic diseases might have caused severe osteoporosis and provoked sacral insufficiency fracture without traumatic insults. A few cases in pregnant and postpartum woman, athletes such as long distant runner and tennis player have also been reported previously4,11,18).
Initial diagnosis is difficult to be made. The clinical presentations including sudden or insidious, intractable low back or pelvic pain coupled with a significant reduction in mobility and independence are variable and similar to symptoms and signs of the other degenerative disease of the lower lumbar spine19). Routine plain radiographic yield of the lumbar spine is limited because it generally shows no demonstrable fracture line at the beginning of symptoms, and fecal material, vascular calcification, and bowel gas may obscure the fracture lines11). Also, in our case we could not find the fracture line at initial plain radiographs. In a suspected case of the sacral insufficiency fracture, MRI and/or CT and/or bone scan must be performed for differential diagnosis. MRI, as the imaging method of choice in diagnosing back pain, is a sensitive means of detecting alterations within the bone marrow2). It can detect signal from bone marrow edema that results from inflammatory and reparation processes of fractures19). However, these injuries might account for the negative findings on initial MRI at an earlier stage7). The findings of the radionuclide bone scan are also characteristic, although less specific3). Increased uptake bilaterally in the upper sacrum may be documented as the classical "H" sign of the sacral insufficiency fracture. But, this classical "H" sign was documented in 43% of all cases in Finiel et al. meta analysis2,6,19). Recently, FDG PET/CT which is an important tool for imaging of cancer may be diagnostic in sacral insufficiency fracture showing typical "H" shaped FDG uptake like bone scan10,20).
The majority of sacral insufficiency fractures are treated conservatively. Bed rest, pain medication, treatment for underlying osteoporosis followed by a return to normal activities over a periods of months result in the recovery of the vast majority of patients17,19). The conservative treatment requiring long term immobilization may cause deep vein thrombosis, pulmonary complications, impaired cardiac function and further aggravation of osteoporosis. For avoidance of the unwanted complication of the conservative treatment, minimally invasive percutaneous procedures such as sacroplasty, which is similar to vertebroplasty, can be performed in the treatment of painful fractures with limited morbidity and early mobilization17,19). Polymethylmethacrylate (PMMA) cement is injected into the fracture site under fluoroscopy or CT guidance. Published studies report immediate pain relief and early mobilization, and decreased analgesic dependence. However, this technique should only be applied to limited patients who failed with conservative treatment and high risk patients for systemic complication because it is still under study8,17,19).
It is difficult to instrument sacral insufficient fractures because of technical difficulties in the fixation of osteoporotic and fragile bone17). Augmentations with instrumentation are considered only for those who fail conservative treatment and have severely destabilized sacrum21).
CONCLUSION
Sacral insufficiency fractures which have vague, similar symptoms and signs with several lower lumbar degenerative disease and spinal trauma may be commonly overlooked cause of low back pain. Physicians should suspect possibility of the sacral insufficiency fracture in patients who are at risk of primary or secondary osteoporosis, presenting with sudden sacropelvic pain and tenderness with no or trivial trauma. Early diagnosis followed by proper treatment is mandatory for improving prognosis and lessening complication.
References
- 1.Boissonnault WG, Thein-Nissenbaum JM. Differential diagnosis of a sacral stress fracture. J Orthop Sports Phys Ther. 2002;32:613–621. doi: 10.2519/jospt.2002.32.12.613. [DOI] [PubMed] [Google Scholar]
- 2.Brahme SK, Cervilla V, Vint V, Cooper K, Kortman K, Resnick D. Magnetic resonance appearance of sacral insufficiency fractures. Skeletal Radiol. 1990;19:489–493. doi: 10.1007/BF00202696. [DOI] [PubMed] [Google Scholar]
- 3.Cooper KL, Beabout JW, Swee RG. Insufficiency fractures of the sacrum. Radiology. 1985;156:15–20. doi: 10.1148/radiology.156.1.4001403. [DOI] [PubMed] [Google Scholar]
- 4.Czarnecki DJ, Till EW, Minikel JL. Unique sacral stress fracture in a runner. AJR Am J Roentgenol. 1988;151:1255. doi: 10.2214/ajr.151.6.1255-a. [DOI] [PubMed] [Google Scholar]
- 5.Daffner RH, Pavlov H. Stress fractures : current concepts. AJR Am J Roentgenol. 1992;159:245–252. doi: 10.2214/ajr.159.2.1632335. [DOI] [PubMed] [Google Scholar]
- 6.Finiels H, Finiels PJ, Jacquot JM, Strubel D. [Fractures of the sacrum caused by bone insufficiency. Meta-analysis of 508 cases.] Presse Med. 1997;26:1568–1573. [PubMed] [Google Scholar]
- 7.Fredericson M, Moore W, Biswal S. Sacral stress fractures : magnetic resonance imaging not always definitive for early stage injuries : a report of 2 cases. Am J Sports Med. 2007;35:835–839. doi: 10.1177/0363546506296519. [DOI] [PubMed] [Google Scholar]
- 8.Garant M. Sacroplasty : a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol. 2002;13:1265–1267. doi: 10.1016/s1051-0443(07)61976-9. [DOI] [PubMed] [Google Scholar]
- 9.Gomez-Puerta JA, Peris P, Llusa M, Guanabens N. Sacral stress fracture as a cause of gluteal artery injury : an unusual complication of a common fracture. Joint Bone Spine. 2008;75:239–241. doi: 10.1016/j.jbspin.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Halac M, Mut SS, Sonmezoglu K, Ylmaz MH, Ozer H, Uslu I. Avoidance of misinterpretation of an FDG positive sacral insufficiency fracture using PET/CT scans in a patient with endometrial cancer : a case report. Clin Nucl Med. 2007;32:779–781. doi: 10.1097/RLU.0b013e318148b408. [DOI] [PubMed] [Google Scholar]
- 11.Karatas M, Basaran C, Ozgul E, Tarhan C, Agildere AM. Postpartum sacral stress fracture : an unusual case of low-back and buttock pain. Am J Phys Med Rehabil. 2008;87:418–422. doi: 10.1097/PHM.0b013e318164a8e6. [DOI] [PubMed] [Google Scholar]
- 12.Lourie H. Spontaneous osteoporotic fracture of the sacrum. An unrecognized syndrome of the elderly. JAMA. 1982;248:715–717. [PubMed] [Google Scholar]
- 13.Lyo IU, Kwon SC, Park JB, Sim HB. Transverse fracture and dislocation at the sacrum. J Korean Neurosurg Soc. 2008;43:31–33. doi: 10.3340/jkns.2008.43.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mattila VM, Niva M, Kiuru M, Pihlajamaki H. Risk factors for bone stress injuries : a follow-up study of 102,515 person-years. Med Sci Sports Exerc. 2007;39:1061–1066. doi: 10.1249/01.mss.0b013e318053721d. [DOI] [PubMed] [Google Scholar]
- 15.Muthukumar T, Butt SH, Cassar-Pullicino VN, McCall IW. Cauda equina syndrome presentation of sacral insufficiency fractures. Skeletal Radiol. 2007;36:309–313. doi: 10.1007/s00256-006-0239-5. [DOI] [PubMed] [Google Scholar]
- 16.Parikh VA, Edlund JW. Sacral insufficiency fractures--rare complication of pelvic radiation for rectal carcinoma : report of a case. Dis Colon Rectum. 1998;41:254–257. doi: 10.1007/BF02238256. [DOI] [PubMed] [Google Scholar]
- 17.Sciubba DM, Wolinsky JP, Than KD, Gokaslan ZL, Witham TF, Murphy KP. CT fluoroscopically guided percutaneous placement of transiliosacral rod for sacral insufficiency fracture : case report and technique. AJNR Am J Neuroradiol. 2007;28:1451–1454. doi: 10.3174/ajnr.A0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silva RT, De Bortoli A, Laurino CF, Abdalla RJ, Cohen M. Sacral stress fracture : an unusual cause of low back pain in an amateur tennis player. Br J Sports Med. 2006;40:460–461. doi: 10.1136/bjsm.2005.023473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsiridis E, Upadhyay N, Giannoudis PV. Sacral insufficiency fractures : current concepts of management. Osteoporos Int. 2006;17:1716–1725. doi: 10.1007/s00198-006-0175-1. [DOI] [PubMed] [Google Scholar]
- 20.Tsuchida T, Kosaka N, Sugimoto K, Itoh H. Sacral insufficiency fracture detected by FDG-PET/CT : report of 2 cases. Ann Nucl Med. 2006;20:445–448. doi: 10.1007/BF03027382. [DOI] [PubMed] [Google Scholar]
- 21.Weber M, Hasler P, Gerber H. Insufficiency fractures of the sacrum. Twenty cases and review of the literature. Spine. 1993;18:2507–2512. doi: 10.1097/00007632-199312000-00021. [DOI] [PubMed] [Google Scholar]