Abstract
Objective
Although anterior cervical discectomy and fusion (ACDF) is the standard treatment for degenerative cervical disc disease, concerns regarding adjacent level degeneration and loss of motion have suggested that arthroplasty may be a better alternative. We have compared clinical and radiological results in patients with cervical disc herniations treated with arthroplasty and ACDF.
Methods
We evaluated 53 patients treated for cervical disc herniations with radiculopathy, 21 of whom underwent arthroplasty and 32 of whom underwent ACDF. Clinical results included the Visual Analogue Scale (VAS) score for upper extremity radiculopathy, neck disability index (NDI), duration of hospital stay and convalescence time. All patients were assessed radiologically by measuring cervical lordosis, segmental lordosis and segmental range-of-movement (ROM) of operated and adjacent disc levels.
Results
Mean hospital stay (5.62 vs. 6.26 days, p<0.05) and interval between surgery and return to work (1.10 vs. 2.92 weeks, p<0.05) were significantly shorter in the arthroplasty than in the fusion group. Mean NDI and extremity VAS score improved after 12 months in both groups. Although it was not significant, segmental ROM of adjacent levels was higher in the fusion group than in the arthroplasty group. And, segmental motion of operated levels in arthroplasty group maintained more than preoperative value at last follow up.
Conclusion
Although clinical results were similar in the two groups, postoperative recovery was significantly shorter in the arthroplasty group. Although it was not significant, ROM of adjacent segments was less in the arthroplasty group. Motion of operated levels in arthroplasty group was preserved at last follow up.
Keywords: Anterior discectomy and fusion (ACDF), Arthroplasty, Cervical disc herniations, Artificial cervical disc, Mobi-C®, Solis cages®
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is the standard treatment for patients with cervical disc herniations. ACDF, however, can result in accelerated degeneration of adjacent segments; this problem encouraged the development of cervical arthroplasty1,3,4,8). Cervical artificial discs are designed to maintain the motion of the intervertebral space, thus theoretically slowing the degeneration of the adjacent disc space and allowing normal physiological curvatures. Total intervertebral disc replacement was designed to preserve motion, avoid limitations of fusion, and allow patients to quickly return to routine activities.
The primary goal of these procedures in the cervical spine is to restore segmental motion after removing local pathology. A secondary goal is to preserve normal motion at adjacent cervical levels, which may prevent later adjacent level degeneration13).
Disc replacement can also eliminate morbidities associated with bone graft harvest, as well as avoiding pseudarthrosis, anterior cervical plating-related complications, and cervical immobilization side-effects. The aim of this retrospective study was to compare the clinical and radiological outcomes in patients receiving ACDF using Solis®-cages (Stryker Spine, NewJersey, U.S.A) and cervical arthroplasty with Mobi-C® (LDR, Troyes, France).
MATERIALS AND METHODS
We retrospectively assessed outcomes in 53 patients (31 men, 22 women) with cervical soft disc herniation who presented with upper extremity radiculopathy, with or without axial neck pain. Patients with multi-level disc disease, evidence of cervical instability, severe degeneration as seen by radiography, serious medical problems, and patients undergoing revision surgery, were excluded.
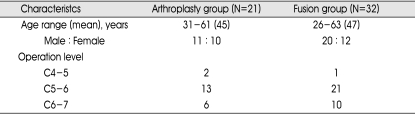
The cervical fusion group consisted of 32 patients (20 men, 12 women), of mean age 47 years (range, 26 to 63 years), followed-up for a mean of 22 months. The arthroplasty group consisted of 21 patients (11 men, 10 women), of mean age 45 years (range, 31 to 61 years), followed-up for a mean of 20 months. Surgery at the C4-5, C5-6, and C6-7 levels was performed in 1, 21, and 10 patients, respectively, in the fusion group, and in 2, 13, and 6 patients, respectively, in the arthroplasty group (Table 1) .
Table 1.
Baseline demographic and clinical characteristics
All patients in the both groups underwent surgery employing the usual right-sided approach and discectomy was performed as usual manner. Then, the appropriate size trial was placed into the disc space to confirm the size, position and height of the implant to be used. The consideration of the stability and prevention of overdistraction led us to choose the implant of optimal height that was also as wide as possible. Iliac bone harvest which was useless in Mobi-C® was inserted into Solis®- cage®. Each implant of both groups was then inserted into the prepared disc space, taking care to ensure correct alignment and position under fluroscopic guidance. After surgery, the patients in fusion group had to keep external cervical orthosis for 2 months.
Clinical results were evaluated using the duration of hospital stay, convalescence time, neck disability index (NDI) and VAS scores of upper extremity radiculopathy. Cervical overall lordosis, segmental lordosis and range-of-motion (ROM) at the operative level, and adjacent segme-ntal range-of-motion (ROM), were evaluated radiologically. Cervical lordosis was measured as the angle formed by the lines drawn parallel to the caudal endplate of C-2 and C-7. Preoperative and postoperative segmental lordosis were measured as the angle formed by the lines drawn parallel to the each endplate forming disc space in the neutral position. Segmental ROM was measured as the difference of segmental lordosis between flexion and extension state in dynamic views and adjacent segmental ROM was measured with the same method. Groups were compared statistically using the Mann-Whitney test and Repeated Measures Analysis of Variance.
RESULTS
Clinical outcomes
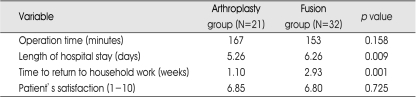
Mean operation time was similar in the arthroplasty and fusion groups (167 vs. 153 min, p>0.05). Length of hospital stay (5.62 vs. 6.26 days, p<0.05) and convalescence time (1.10 vs. 2.93 weeks, p<0.05) were significantly shorter in the arthroplasty than in the fusion group. Patient satisfaction, measured at last follow up, was similar in the arthroplasty and fusion groups (6.85 vs. 6.80, p>0.05) (Table 2).
Table 2.
Clinical outcomes in the arthroplasty and fusion groups
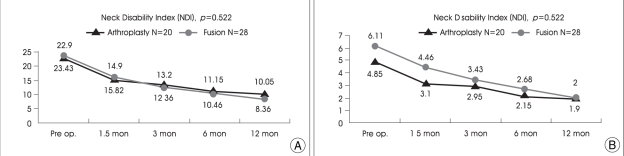
NDI of both groups decreased over 12 months, from 22.9 to 10.05 in the arthroplasty group and from 23.43 to 8.36 in the fusion group (Fig. 1A). Upper extremity VAS scores of both groups also decreased over 12 months, from 4.85 to 1.9 in the arthroplasty group and from 6.11 to 2.0 in the fusion group. But, both of these data were not significantly different (Fig. 1B). There was no newly aggravated symptoms including neck pain in both groups.
Fig. 1.
A : Neck Disability Index in the arthroplasty and fusion groups (p>0.05). B : Visual analogue scale scores of radiculopathy in the arthroplasty and fusion groups (p>0.05).
Radiological outcomes
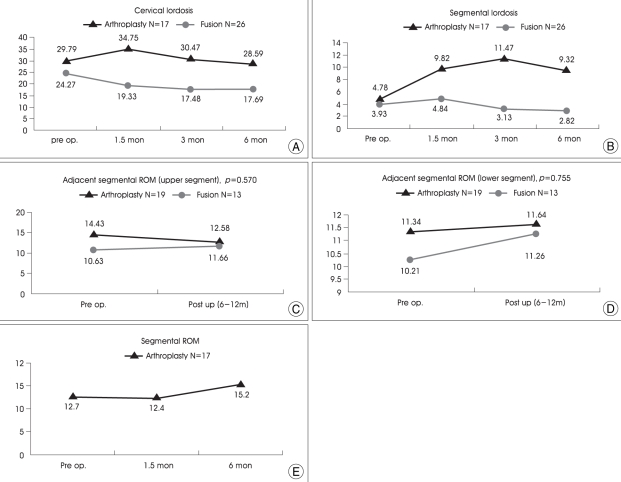
Six months after surgery, cervical lordosis fell from 29.79 to 28.59 in the arthroplasty group and from 24.27 to 17.69 in the fusion group. In the arthroplasty group, lordosis increased during the immediate postoperative period and then decreased to preoperative levels. In the fusion group, however, lordosis decreased gradually, and could not return to preoperative levels (Fig. 2A).
Fig. 2.
A : Cervical lordosis in the arthroplasty and fusion groups. In the arthroplasty group, cervical lordosis increased immediately after surgery, later decreasing to preoperative levels. Cervical lordosis in the fusion group decreased after surgery, but did not return to preoperative levels. B : Segmental lordosis in the arthroplasty and fusion groups. In the arthroplasty group, segmental lordosis increased after surgery, decreasing after 3 months and returning to preoperative levels. In the fusion group, however, segmental lordosis increased immediately after surgery, later decreasing but not returning to preoperative levels. C : Adjacent range-of-movement of the upper level in the arthroplasty and fusion groups. Following surgery, upper ROM decreased in the arthroplasty group but increased in the fusion group (p>0.05). D : Adjacent range-of-movement (ROM) of the lower level in the arthroplasty and fusion groups. Following surgery, lower ROM increased in both groups, but the increase is greater in the fusion group (p>0.05). E : Segmental range-of-movement (ROM) of the arthroplasty decreased immediately after surgery, later increasing more than preoperative levels.
Segmental lordosis changed from 4.78 to 9.32 in the arthroplasty group and fell from 3.93 to 2.82 in the fusion group. Although segmental lordosis in the arthroplasty group maintained more than preoperative levels, the lordosis became a little more kyphotic than before surgery in the fusion group (Fig. 2B).
Upper segmental ROM of the arthroplasty group decreased postoperatively, from 14.42 to 12.58, whereas upper segmental ROM of the fusion group increased, from 10.63 to 11.66 (p>0.05) (Fig. 2C).
Although lower segmental ROM increased postoperatively in both groups, the increase was higher in the fusion group than in the arthroplasty group (from 10.21 to 11.26 vs. from 11.34 to 11.64, p>0.05) (Fig. 2D).
Segmental ROM of operative level in arthroplasty group increased postoperatively, although it slightly decreased immediately after surgery, the last ROM was larger than preoperative level (from 12.7 to 15.2) (Fig. 2E).
Complications
No complications related to the device such as settling and migration were observed in arthroplasty group, but five cage subsidences were noted in fusion group. There was no heterotrophic ossification (HO) in arthroplasty group.
DISCUSSION
ACDF is currently the most common surgical approach used to treat patients with debilitating cervical degenerative disc disease.3) Although ACDF often provides benefits at the operative level, ACDF-associated adverse effects include adjacent segmental disc disease and limited neck motion. Loss of spinal motion after ACDF is related to additional mechanical stress at adjacent levels, and this stress may initiate or accelerate the degeneration of such levels2,8,11). Nevertheless, the concept of adjacent-segment degeneration remains unproven and the true incidence is controversial issue. However, several studies showed that fusion alters spinal biomechanics7). Increased intradiscal pressure at levels adjacent to intervertebral fusions has been seen in biomechanical modeling of the cervical spine : about 73% and 45% increase in intradiscal pressure at upper and lower levels17). Therefore, there are always the risks of adjacent segment degeneration to be considered due to increase of intradiscal pressure at adjacent levels7). In contrast, arthroplasty of the cervical intervertebral disc, which can maintain the motion by the artificial joint can theoretically prevent degeneration of adjacent spaces.
For arthroplasty, our institute uses Mobi-C®, which is relatively easy to manage, in a procedure similar to that of ACDF. Surgical insertion of Mobi-C® disc prosthesis is very simple, safe, and reproducible, because the implant holder easily allows the adjustment of position, axis and depth6). Thus, the mean operation time was similar in the two groups. We also found that clinical results, as determined by NDI and upper extremity VAS score, were similar in the two groups. Similar results have been reported previously, as has a relationship among symptom improvement and lesion decompression and stabilization9,10). In that study, a significant pain reduction in neck and arm was observed, with no significant differences between both groups. Postoperative recovery, as determined by length of stay in hospital and convalescence time, was significantly better in the arthroplasty group than in the fusion group. We observed no incidence of postoperative orthosis or iliac harvest morbidity in the arthroplasty group, thus shortening postoperative recovery time14,15).
We found that neither postoperative overall cervical lordosis nor segmental lordosis recovered to preoperative levels in the fusion group; rather, these data became more kyphotic. Similarly, a previous study reported that, of 106 patients, 10 (9%) showed cage subsidence in cervical fusion surgery16). Unfortunately, some patients of fusion group, who became more kyphotic, showed cage subsidences after surgery in our study. Other authors have reported that degeneration of adjacent levels was significantly associated with loss of physiological cervical lordosis in a retrospective study of 42 patients followed for a mean of 10 years after undergoing anterior cervical discectomy and fusion for symptomatic cervical lordosis5,7). They also emphasized the importance of the relation between postoperative sagittal alignment and clinical outcomes. We must also consider our procedure didn't use anterior cervical plate. One study reported ACDF with plate could reduce cage subsidence, which might suggest high ratio of kyphosis of our data. However, we thought plate related complications, such as esophageal injury, pulled out screw might be severe problem and clinical outcomes between ACDF with or without anterior plate were not different in one study. Therefore, above results explain the difference of overall and segmental lordosis between two groups in our data were so high and similar clinical outcomes.
One of the primary goals of cervical disc replacement is to reproduce normal kinematics after implantation12). Another study showed the preservation of motion in Bryan® (Medtronic, Tennessee, U.S.A) treated spinal segments17). Our results also showed segmental ROM preservation after surgery.
We found that adjacent upper segmental ROM decreased in the arthroplasty group, but increased in the fusion group. Similarly, the increase in lower segmental ROM was greater in the fusion group than in the arthroplasty group. Taken together, these findings indicate that, compared with fusion, arthroplasty has the advantage of preventing hypermobility of adjacent segments. Similarly, other studies have shown that motion of the treated level maintained at preoperative levels in patients who underwent arthroplasty, indicating that this form of surgery did not affect the motion of adjacent levels9,10,12,18).
CONCLUSION
Clinical results, such as NDI and upper extremity VAS score, were similar in both groups that underwent arthroplasty or fusion. Postoperative recovery time was, however, shorter in the arthroplasty group, which may be related to absence of postoperative orthosis and iliac graft donor site pain. Patients in the fusion group tended to become more kyphotic than before surgery, which may be related to postoperative graft subsidence in some cases. Although statistically not significant, ROM of adjacent segments was smaller in the arthroplasty than in the fusion group. And, ROM of the operative level in the arthroplasty group was preserved. However, our study has limitation of short follow up and small number of patients. More cases and long-term follow up are needed to make conclusion about the efficacy of cervical arthroplasty.
ACKNOWLEDGEMENTS
This paper was presented at the 2008 Spring Meeting of the Korean Neurosurgical Society.
References
- 1.Cummins BH, Robertson JT, Gill SS. Surgical experience with an implanted artificial cervical joint. J Neurosurg. 1998;88:943–948. doi: 10.3171/jns.1998.88.6.0943. [DOI] [PubMed] [Google Scholar]
- 2.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002;27:2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 3.Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17:79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10:320–324. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim SH, Shin HC, Shin DA, Kim KN, Yoon do H. Early clinical experience with the mobi-C disc prosthesis. Yonsei Med J. 2007;48:457–464. doi: 10.3349/ymj.2007.48.3.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim SW, Shin JH, Arbatin JJ, Park MS, Chung YK, McAfee PC. Effects of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine. Eur Spine J. 2008;17:20–29. doi: 10.1007/s00586-007-0459-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kulkarni V, Rajshekhar V, Raghuram L. Accelerated spondylotic changes adjacent to the fused segment following central cervical corpectomy : magnetic resonance imaging study evidence. J Neurosurg. 2004;100:2–6. doi: 10.3171/spi.2004.100.1.0002. [DOI] [PubMed] [Google Scholar]
- 9.Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion : a randomized controlled clinical trial. J Neurosurg Spine. 2007;6:198–209. doi: 10.3171/spi.2007.6.3.198. [DOI] [PubMed] [Google Scholar]
- 10.Nabhan A, Ahlhelm F, Pitzen T, Steudel WI, Jung J, Shariat K, et al. Disc replacement using Pro-Disc C versus fusion : a prospective randomised and controlled radiographic and clinical study. Eur Spine J. 2007;16:423–430. doi: 10.1007/s00586-006-0226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pickett GE, Rouleau JP, Duggal N. Kinematic analysis of the cervical spine following implantation of an artificial cervical disc. Spine. 2005;30:1949–1954. doi: 10.1097/01.brs.0000176320.82079.ce. [DOI] [PubMed] [Google Scholar]
- 12.Sasso RC, Smucker JD, Hacker RJ, Heller JG. Artificial disc versus fusion : a prospective, randomized study with 2-year follow-up on 99 patients. Spine. 2007;32:2933–2940. doi: 10.1097/BRS.0b013e31815d0034. [DOI] [PubMed] [Google Scholar]
- 13.Shim CS, Lee SH, Park HJ, Kang HS, Hwang JH. Early clinical and radiologic outcomes of cervical arthroplasty with Bryan Cervical Disc prosthesis. J Spinal Disord Tech. 2006;19:465–470. doi: 10.1097/01.bsd.0000211235.76093.6b. [DOI] [PubMed] [Google Scholar]
- 14.Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine. 2003;28:134–139. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- 15.St John TA, Vaccaro AR, Sah AP, Schaefer M, Berta SC, Albert T, et al. Physical and monetary costs associated with autogenous bone graft harvesting. Am J Orthop. 2003;32:18–23. [PubMed] [Google Scholar]
- 16.van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW. Anterior cervical interbody fusion with a titanium box cage : early radiological assessment of fusion and subsidence. Spine J. 2005;5:645–649. doi: 10.1016/j.spinee.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Weinhoffer SL, Guyer RD, Herbert M, Griffith SL. Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine. 1995;20:526–531. doi: 10.1097/00007632-199503010-00004. [DOI] [PubMed] [Google Scholar]
- 18.Yoon DH, Yi S, Shin HC, Kim KN, Kim SH. Clinical and radiological results following cervical arthroplasty. Acta Neurochir (Wien) 2006;148:943–950. doi: 10.1007/s00701-006-0805-6. [DOI] [PubMed] [Google Scholar]