Abstract
Cavernous malformations (CMs) arising from the optic nerve and chiasm are extremely rare. The authors present a case of 39-year-old woman with CMs of the optic chiasm. She was referred due to sudden onset of bitemporal hemianopsia and headache, the so-called 'chiasmal apoplexy'. MRI findings suggested a diagnosis of hemorrhage and vascular malformation of the optic chiasm. Pterional craniotomy revealed an intrachiasmatic cavernous malformation with hemorrhage. The malformation was totally excised, but field deficits remained unchanged after surgery.
Keywords: Cavernous malformation, Optic chiasm, Apoplexy
INTRODUCTION
A cavernous malformation (CM), also known as cavernous angioma or cavernoma, is a vascular malformation characterized by the presence of sinusoid-like capillary vessels containing blood in very sluggish circulation1).
CMs have been reported to involve cranial nerves in the following locations : the optic nerve and chiasm, third nerve, seventh nerve in the temporal bone, and seventh and eighth nerves in the internal auditory canal2,5,7). CMs originating from the optic chiasm and/or optic tract are very rare. CMs within the anterior visual pathways can cause visual symptoms as well as headache, retro-orbital pain and nausea, the so-called 'chiasmal apoplexy.' The clinical symptoms of CMs are mostly the result of intrinsic and extrinsic bleeding. We recently experienced a case of chiasmal CMs presenting with chiasmal apoplexy. In this report, the clinical, radiological features and surgical management of this vascular malformation are reviewed with pertinent literature.
CASE REPORT
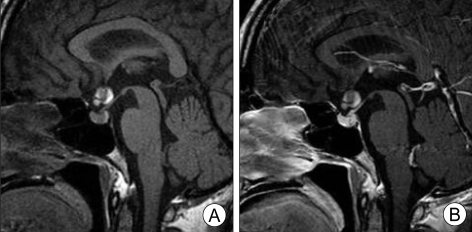
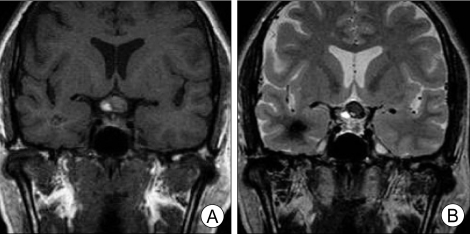
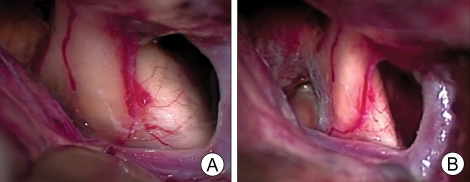
A 39-year-old woman was referred due to sudden onset of visual disturbance, headache and nausea. She had a long history of headache, but no other neurological deficits were noted on admission. Visual field examination showed bitemporal hemianopsia. MRI demonstrated a 1.5-cm sized mass involving the optic chiasm, with intrachiasmatic and posterior extension. Non-contrast-enhanced and contrast-enhanced sagittal T1-weighted MR images of the sella showed an enlargement of the optic chiasm with peripheral hyperintensity and central hypointensity. No significant contrast enhancement was observed after the administration of gadolinium (Fig. 1). Coronal noncontrast-enhanced T1-weighted and T2-weighted MR images revealed an intrachiasmal lesion. The mass lesion was shown as diffuse hyperintensity on T1-weighted images and mixed signal intensity surrounded by a markedly hypointense peripheral rim of hemosiderin on T2-weighted images (Fig. 2). Based on MR findings, we diagnosed this lesion as a chiasmal CM with hemorrhage. Microsurgical excision was performed via right pterional craniotomy. The mass was located inside the optic chiasm and a small portion reached up to the surface (Fig. 3A). Complete removal of the mass lesion was accomplished by microsurgical dissection (Fig. 3B). The margins were distinct, allowing the lesion to be peeled away from the surrounding tissue by repeated coagulation and piecemeal removal. There was no significant bleeding. Histological examination revealed a CM (Fig. 4). After the operation, the patient showed good recovery without further neurological deficits, but the the patient's visual field deficits remained unchanged.
Fig. 1.
Non-contrast-enhanced (A) and contrast-enhanced (B) T1-weighted sagittal magnetic resonance images of the sella demonstrating a 1.5-cm sized mass involving the optic chiasm. No significant contrast enhancement is observed after the administration of gadolinium.
Fig. 2.
Coronal non-contrast-enhanced T1-weighted (A) and T2-weighted magnetic resonance images (B) revealing an intrachiasmal lesion. The mass lesion demonstrates diffuse hyperintensity on T1-weighted imaging and mixed signal intensity surrounded by marked hypointense peripheral rim of hemosiderin on T2-weighted imaging.
Fig. 3.
The mass is located inside the optic chiasm (A). Complete removal of the mass lesion has been accomplished by microsurgical dissection (B).
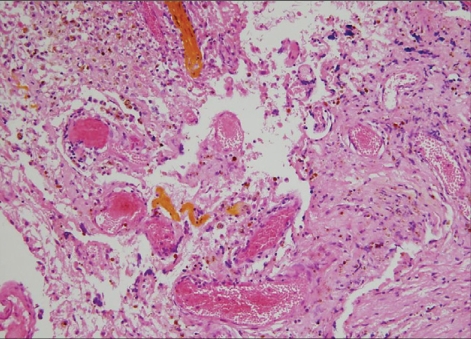
Fig. 4.
Low-power photomicrographs showing various thrombosis and calcifications within the cavernous vascular spaces. Thin-walled vascular channels with little intervening brain are also noted (H & E, ×100).
DISCUSSION
CMs account for approximately 5 to 10% of all vascular malformations8,9). Although CMs are most commonly found in the cerebral hemisphere, they can be located anywhere. CMs originating from cranial nerves have rarely been reported. Cranial nerves such as the optic nerve and chiasm, oculomotor, trigeminal, intracranial portion of the seventh and eighth nerve and hypoglossal nerve have been affected2,5,7). CMs in the optic nerve and chiasm are extremely rare.
Clinical features
CMs of the optic chiasm are most often revealed by chiasmatic apoplexy, which typically occur during the second or third decade of life3,6). The term 'chiasmal apoplexy', related to chiasmal hemorrhage, was first introduced by Maitland et al.4) Characteristic clinical symptoms are associated with three main findings : sudden headache, sudden change of visual acuity, and significant visual field change. Lehner et al.3), who analyzed 30 cases of chiasmal CMs, reported that the bleeding frequency seemed to be much higher at this location than at other regions. However, this phenomenon may actually be due to the fact that even very subtle hemorrhages are likely to cause symptoms when the lesion lies within cranial nerves2,3,10). It was reported that more than one-third of the reported cases had previous episodes of transient blurred vision and headache3,6). Our patient also reported chronic headache, but she had no history of visual disturbance. The symptom of acute visual deterioration and headache in our patient might have originated from acute intrinsic hemorrhage of the chiasmal CM.
Neuroimaging
The diagnosis of CMs is mostly straightforward in typical cases. MRI is considered to be the most sensitive and specific imaging technique for the detection and characterization of these lesions8,9). MRI is especially sensitive to small anatomical structures such as cranial nerves10). CMs of the optic chiasm or nerve and intracerebral CMs present with similar MRI findings6). MR images typically show focal suprasellar lesions with heterogeneous signal intensity, involving the optic pathways, and hyperintense areas suggest recent hemorrhage2). Post-contrast enhancement should be minimal2). The differential diagnosis includes chiasmal neoplasm, especially optic gliomas or craniopharyngiomas, arteriovenous malformations, and multiple sclerosis6). This uncertainty in diagnosis is another reason for surgical excision of these lesions. In our case, the preoperative diagnosis of chiasmal CM was made without difficulty because the patient's MR findings were typical of chiasmal CM, showing a reticular core of mixed signal-intensity and a surrounding rim of decreased signal-intensity.
Treatment and outcome
The current, well-established indications for surgical resection of CMs are recurrent hemorrhage, progressive neurologic deterioration, and intractable epilepsy, unless the location is associated with an unacceptably high surgical risk1,9). In patients with chiasmal syndrome due to hemorrhage from CMs of the optic chiasm, emergency surgery is recommended to avoid permanent damage3,6). Despite its critical location, good surgical outcomes have been reported in the literature concerning chiasmal CMs3,6). Thus, complete surgical removal should be attempted for chiasmal CMs. As demonstrated in our case and in previous reports, chiasmal CMs can be safely resected with preservation or even restoration of cranial nerve function.
CONCLUSION
We report a rare case of an optic chiasm CM that was completely removed by microsurgical excision.
Acknowledgement
This work was supported for two years by Pusan National Uuiversity Research Grant.
References
- 1.Del Curling O, Jr, Kelly DL, Jr, Elster AD, Craven TE. An analysis of the natural history of cavernous angiomas. J Neurosurg. 1991;75:702–708. doi: 10.3171/jns.1991.75.5.0702. [DOI] [PubMed] [Google Scholar]
- 2.Deshmukh VR, Albuquerque FC, Zabramski JM, Spetzler RF. Surgical management of cavernous malformations involving the cranial nerves. Neurosurgery. 2003;53:352–357. doi: 10.1227/01.neu.0000073531.84342.c2. discussion 357. [DOI] [PubMed] [Google Scholar]
- 3.Lehner M, Fellner FA, Wurm G. Cavernous haemangiomas of the anterior visual pathways. Short review on occasion of an exceptional case. Acta Neurochir(Wien) 2006;148:571–578. doi: 10.1007/s00701-006-0751-3. discussion 578. [DOI] [PubMed] [Google Scholar]
- 4.Maitland CG, Abiko S, Hoyt WF, Wilson CB, Okamura T. Chiasmal apoplexy. Report of four cases. J Neurosurg. 1982;56:118–122. doi: 10.3171/jns.1982.56.1.0118. [DOI] [PubMed] [Google Scholar]
- 5.Matias-Guiu X, Alejo M, Sole T, Ferrer I, Noboa R, Bartumeus F. Cavernous angiomas of the cranial nerves. Report of two cases. J Neurosurg. 1990;73:620–622. doi: 10.3171/jns.1990.73.4.0620. [DOI] [PubMed] [Google Scholar]
- 6.Muta D, Nishi T, Koga K, Yamashiro S, Fujioka S, Kuratsu J. Cavernous malformation of the optic chiasm : case report. Br J Neurosurg. 2006;20:312–315. doi: 10.1080/02688690601000238. [DOI] [PubMed] [Google Scholar]
- 7.Park DM, Kim DH. Cavernous angioma of the oculomotor nerve. J Korean Neurosurg Soc. 2005;38:147–150. [Google Scholar]
- 8.Rigamonti D, Hadley MN, Drayer BP, Johnson PC, Hoenig-Rigamonti K, Knight JT, et al. Cerebral cavernous malformations. Incidence and familial occurrence. N Engl J Med. 1988;319:343–347. doi: 10.1056/NEJM198808113190605. [DOI] [PubMed] [Google Scholar]
- 9.Robinson JR, Awad IA, Little JR. Natural history of the cavernous angioma. J Neurosurg. 1991;75:709–714. doi: 10.3171/jns.1991.75.5.0709. [DOI] [PubMed] [Google Scholar]
- 10.Shibuya M, Baskaya MK, Saito K, Suzuki Y, Ooka K, Hara M. Cavernous malformations of the optic chiasma. Acta Neurochir(Wien) 1995;136:29–36. doi: 10.1007/BF01411432. [DOI] [PubMed] [Google Scholar]