Abstract
Objective
To present a case of unrecognized female epispadias
Design
Case Report
Setting
University-based reproductive endocrinology and fertility clinic
Patient
A 16-year-old female with epispadias, history of mild urinary incontinence, auditory neuropathy and functional hyperandrogenism
Main Outcome Measure
Peripheral blood array-based comparative genomic hybridization (array CGH)
Results
The patient was referred for evaluation of excessive weight gain, secondary amenorrhea and abnormal external genitalia. Examination under anesthesia revealed bilateral labia minora hypertrophy, bifid clitoris and a patulous urethra, consistent with female epispadias. Hormonal evaluation showed functional hyperandrogenism while peripheral blood array-based comparative genomic hybridization (array CGH) showed no chromosomal deletions or duplications.
Conclusion
Female epispadias is a rare abnormality, not commonly recognized by most practitioners. The diagnosis is supported by a history of urinary incontinence and physical findings of bifid clitoris and patulous urethra. The condition can have serious physical and psychological consequences leading to a gross disruption of social function.
Keywords: epispadias, bifid clitoris, urinary incontinence, patulous urethra
The bladder exstrophy-epispadias complex (BEEC) is an anterior midline defect with variable expression involving the urinary tract and anterior abdominal wall. BEEC manifests as varying degrees of severity, with cloacal exstrophy (CE) representing the most severe form and epispadias representing the mildest form. Isolated epispadias without exstrophy is a rare anomaly; the incidence being 1 in 117,000 in males and 1 in 448,000 in females (1). The main characteristics of this abnormality include lack of labial anterior comissure, bifid clitoris, flattened mons pubis with absence of midline pubic hair, patulous urethra and immature bladder neck. Those patients who present with significant urinary symptoms and genital abnormality are commonly diagnosed before adolescence. In some less affected patients, however, the anomaly goes unrecognized. In a previous case report, the correct diagnosis was not reached until age 39 in a woman with 3 prior vaginal deliveries and a previous incontinence surgery (2).
Case
A 16-year-old Caucasian female with a complicated past medical history of Cushings disease status post pituitary resection, genital abnormality, mild cognitive delay, auditory neuropathy, complex partial seizure disorder and depression presented to the Reproductive Endocrinology and Fertility clinic for the evaluation of excessive weight gain and secondary amenorrhea. The patient also complained of discomfort with physical activity and sitting secondary to the presence of excessive genital skin. She was born prematurely at 34 weeks gestation and experienced neonatal complications including Group B Streptococcal sepsis and grade 4 intraventricular hemorrhage. Hydrocephalus was diagnosed at 8 months of age with subsequent ventriculo-peritoneal shunt placement. She had occasional urinary incontinence as a child, but never to the degree to warrant evaluation such as cystometrography. Pubertal history included presence of isolated premature adrenarche at age 4, thelarche at age 12, and menarche at approximately age 13.
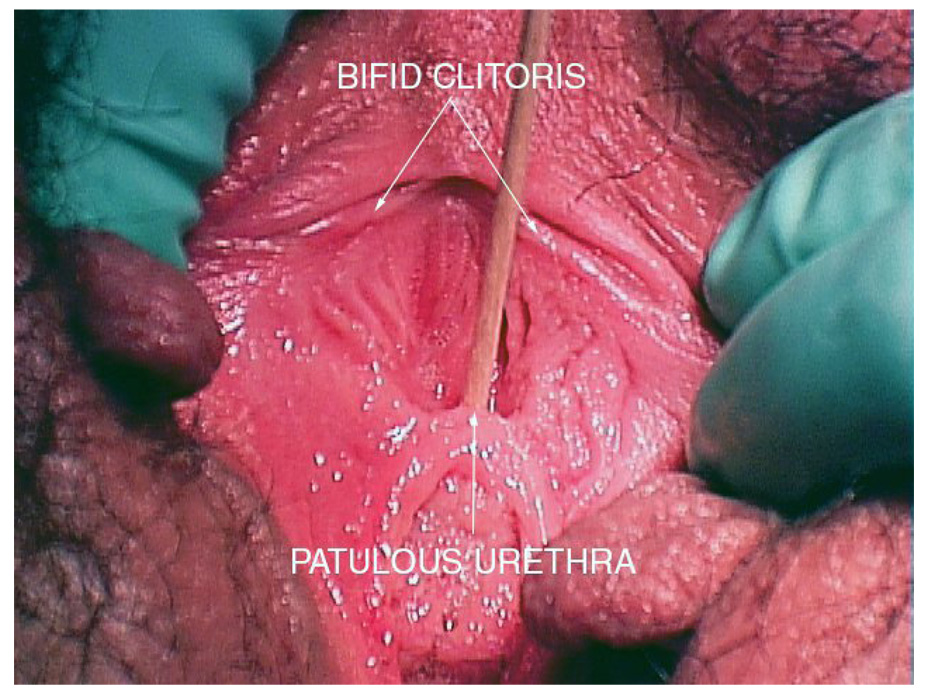
Physical examination was significant for general obese appearance (BMI-Z score= 2.52), mild to moderate acne, purple striae in the axillae, lateral thighs and lower abdomen and abnormal genital exam including a bifid clitoris, patulous urethra and bilateral hypertrophy of the labia minora (Figure 1). Laboratory evaluation was consistent with functional androgen excess and peripheral blood array-based comparative genomic hybridization (array CGH) showed no chromosomal deletions or duplications. Surgery was performed with bilateral labial minora reduction. Written parental permission was obtained for the photograph used in this publication.
Fig 1.
A photograph of external genitalia showing bifid clitoris and patulous urethra.
Discussion
Epispadias without exstrophy is an extremely rare congenital abnormality in females (3–4 times less common than in males). Patients with isolated epispadias present with various degrees of abnormality. A classification by Davis described three degrees of epispadias in female patients (3). In the mildest degree, the urethral meatus simply appears patulous. In the intermediate degree, the urethra is dorsally split along most of the urethra. Finally, in the most severe degree of epispadias, the urethral cleft involves the entire length of the urethra and sphincteric mechanism and the patient is rendered incontinent. The ureterovesical junction is inherently deficient in cases of epispadias, and the ureters often enter the bladder from a lateral position, resulting in reflux. The incidence of reflux is reported to be 30% to 75% (4). Typically, severely affected patients are diagnosed before adolescence, while women with milder forms of epispadias may remain unrecognized, either because surgical correction occurs without diagnosis or because continence is not greatly affected.
There are limited data on the epidemiology, risk factors and genetics of BEEC, perhaps because of its low birth prevalence. BEEC most commonly occurs as an isolated sporadic birth defect with a risk of < 1% in siblings. Epidemiological studies reveal no evidence of a single-gene defect or common environmental factor associated with this syndrome (5, 6). Possible reported associations include Caucasian race (5), advanced parental age (5), birth order (5, 6), and in vitro fertilization (7).
Most BEEC cases occur sporadically. However, to date, 23 families having at least two affected members, have also been reported (8). There are also 28 reported cases of twin pairs, 9 of whom were concordant monozygotic pairs (8). The inheritance pattern in these families is most suggestive of a complex genetic trait (interaction of multiple genes and the environment) as opposed to conventional Mendelian inheritance. A few of the reported familial cases have also exhibited sensorineural hearing loss associated with BEEC (8, 9). One of these cases (9) involved a Filipino-American girl with myelocystocele-cloacal exstrophy and moderate sensorineural hearing loss; the hearing loss was also present in 11 additional family members. In this particular family, a mitochondrial 12s rRNA gene mutation was identified, which is thought to be associated with familial progressive hearing loss, and of unknown significance in relation to the exstrophy syndrome.
Treatment goals for epispadias include achievement of complete continence, preservation of the urinary system function and correction of genital abnormalities. Various surgical options have been reported to control continence including transvaginal plication of the urethra and bladder neck, muscle transplantations, urethra twisting, cauterization of the urethra, bladder flap, Marshall-Marchetti-Krantz vesicourethral suspension and submucosal injection of bulking agents (1, 4, 10–12). Anti-reflux surgery is usually necessary. Correction of the abnormal external genitalia may be necessary in more severe cases when there is substantial separation of the hemiclitorides and the labial minora comissure and posterior displacement of the labia majora. A “mons plasty” has been described which involves the following surgical steps; excision of the previous mons pubis scar and hairless area in cases with previous surgery for bladder exstrophy, lengthening of the labia minora with a Y-V vaginoplasty, reuniting of the hemiclitorides and anterior labia minora to form a clitoral hood and superior-medial rotation of the labia majora to re-establish the correct anatomical relationship of the minor and major labia (13).
The delayed diagnosis in our patient was most likely due to factors including lack of significant urinary incontinence and mild external genitalia abnormalities compared to more severe cases. Fortunately she did not require surgical intervention.
In summary, female epispadias is a rare condition that often goes unrecognized in cases lacking significant urinary incontinence. Milder forms of the condition should be possible to diagnose if certain key features are identified including; (i) diastasis of the pubis symphysis (clinically palpable as a gap or visible on pelvic X-ray), with or without a bifid clitoris; (ii) an oblong external urethral meatus (which may be patulous); (iii) a history of unexplained urinary incontinence; (iv) a low bladder leak pressure on cystometrography.
Acknowledgments
Clinical activities for AMH are supported from NIH K23 RR 021979-03.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Capsule
Female epispadias is a rare abnormality often unrecognized by practitioners.
Characteristics include a bifid clitoris, patulous urethra, flattened mons pubis and varying degrees of urinary incontinence.
References
- 1.Gearhart J, Mathews R. Exstrophy-Epispadias Complex. In: Wein A, editor. Campbell-Walsh Urology. Philadelphia: Saunders Elsevier; 2007. pp. 3547–3548. [Google Scholar]
- 2.Yeni E, Unal D, Verit A, Karatas O. An adult female epispadias without exstrophy was presented with urinary incontinence: a case report. International Urogynecology Journal. 2004;15:212–213. doi: 10.1007/s00192-004-1131-2. [DOI] [PubMed] [Google Scholar]
- 3.Davis D. Epispadias in females and its surgical treatment. Surg Gynecol Obstet. 1928;47:680–696. [Google Scholar]
- 4.Gearhart J, Peppas D, Jeffs R. Complete genitourinary reconstruction in female epispadias. J Urol. 1993;149:1110–1113. doi: 10.1016/s0022-5347(17)36310-3. [DOI] [PubMed] [Google Scholar]
- 5.Boyadjiev SA, Dodson JL, Radford CL, Ashrafi GH, Beaty TH, Mathews RI, et al. Clinical and molecular characterization of the bladder exstrophy-epispadias complex: analysis of 232 families. BJU International. 2004;94:1337–1343. doi: 10.1111/j.1464-410X.2004.05170.x. [DOI] [PubMed] [Google Scholar]
- 6.International Clearinghouse for Birth Defects Monitoring Subcommittee. A communication from the international clearinghouse for birth defects monitoring systems. Teratology. 1987;36:221–227. doi: 10.1002/tera.1420360210. [DOI] [PubMed] [Google Scholar]
- 7.Wood H, Trock B, Gearhart J. In vitro fertilization and the cloacal-bladder exstrophy-epispadias complex: is there an association? J Urol. 2003;169:1512–1515. doi: 10.1097/01.ju.0000054984.76384.66. [DOI] [PubMed] [Google Scholar]
- 8.Kajbafzadeh A-M, Tajik P, Payabvash S, Farzan S, Solhpour A. Bladder exstrophy and epispadias complex in sibling: case report and review of literature. Pediatric Surgery International. 2006;22:767–770. doi: 10.1007/s00383-006-1741-5. [DOI] [PubMed] [Google Scholar]
- 9.Nye J, Hayes E, Amendola M, Vaughn D, Charrow J, Mclone D, et al. Myelocystocele-cloacal exstrophy in a pedigree with a mitochondrial 12S rRNA mutation, aminoglycoside-induced deafness, pigmentary disturbances, and spinal anomalies. Teratology. 2000;61:165–171. doi: 10.1002/(SICI)1096-9926(200003)61:3<165::AID-TERA3>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 10.Mouriquand P, Bubanj T, Feyaerts A, Jandric M, Timsit M, Mollard P, et al. Long-term results of bladder neck reconstruction for incontinence in children with classical bladder exstrophy or incontinent epispadias. BJU International. 2003;92:997–1002. doi: 10.1111/j.1464-410x.2003.04518.x. [DOI] [PubMed] [Google Scholar]
- 11.Mollard P, Basset T, Mure P. Female Epispadias. The Journal of Urology. 1997;158:1543–1546. [PubMed] [Google Scholar]
- 12.Burki T, Hamid R, Ransley P, Mushtaq I, Duffy P. Injectable polydimethylsiloxane for treating incontinence in children with the exstrophy-epispadias complex: long-term results. BJU International. 2006;98:849–853. doi: 10.1111/j.1464-410X.2006.06378.x. [DOI] [PubMed] [Google Scholar]
- 13.Cook AJ, Farhat WA, Cartwright LM, Khoury AE, Pippi Salle JL. Simplified mons plasty: A new technique to improve cosmesis in females with the exstrophy-epispadias complex. The Journal of Urology. 2005;173:2117–2120. doi: 10.1097/01.ju.0000157687.37406.d8. [DOI] [PubMed] [Google Scholar]