Abstract
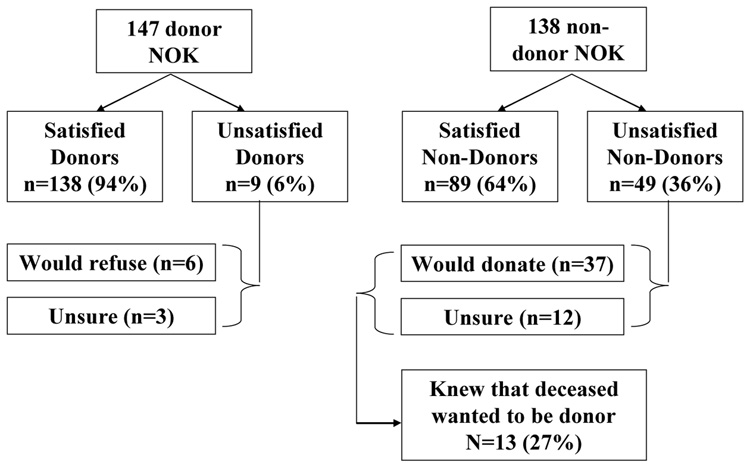
We examined the instability of organ donation decisions made by next-of-kin and factors that predict whether non-donors wish they had consented to donation. Next-of-kin of donor-eligible individuals from one organ procurement organization participated in a semi-structured telephone interview. Participants were asked if they would make the same decision if they had to make it again today. Of the 147 next-of-kin donors, 138 (94%) would make the same decision again; 6 (4%) would not consent to donation, and 3 (2%) were unsure. Of the 138 next-of-kin non-donors, 89 (64%) would make the same decision again, 37 (27%) would consent to donation, and 12 (9%) were unsure. Regret among non-donors was more likely when the next-of-kin had more favorable transplant attitudes (OR=1.76, CI=1.15, 2.69), had the first donation discussion with a non-OPO professional (OR=0.21, CI=0.13, 0.65), was not told their loved one was dead before this discussion (OR=0.23, CI=0.10, 0.50), did not feel they were given enough time to make the decision (OR=0.25, CI=0.11, 0.55), had not discussed donation with family members (OR=0.30, CI=0.13, 0.72), and had not heard a public serve announcement about organ donation (OR=0.29, CI=0.13, 0.67). OPOs should consider targeting these variables in educational campaigns and donation request approaches.
Keywords: organ donation, decision stability, regret, organ procurement organization
INTRODUCTION
Despite donor designation legislation in most states, which permits organ procurement organizations (OPO) to recover organs when the deceased’s donation intentions have been documented, family members continue to play a prominent role in the donation decision-making process. Several studies in recent years have highlighted the many factors that influence donation decisions by next-of-kin.1–6 OPO practices and the Organ Donation Breakthrough Collaborative have, in part, used findings from these studies to develop new strategies or to modify existing ones to optimize organ donation consents and organs recovered per donor.7–8
In addition to these key objectives, OPOs strive to facilitate a “good decision” – one that is characterized by providing families with sufficient organ donation information to make an informed choice, the family feeling comfortable with their decision, and OPO and medical staff supporting the family’s donation decision, whether donation consent is obtained or not. There is recognition within the OPO community that family members may confront a similar situation in the future and a negative experience now might lead to donation resistance in the future. However, despite the best efforts of OPOs, family members often must consider a donation request in a relatively short time period and factors such as the deceased’s donation intentions, existing organ donation attitudes, family disagreement, requestor characteristics, and other contextual variables are related to the donation decision.1,4
One issue that has not been the focus of much study is whether next-of-kin later come to regret their decision to consent to or refuse the donation request. Currently, we have limited information about how many next-of-kin donors and non-donors would make the same or a different decision if they had to do so again, and about the variables that are associated with decision instability. In the only study to examine this issue in some detail, Burroughs et al.9 found that 21% of the 225 families they surveyed would not make the same donation decision again. More specifically, 14% of next-of-kin who consented to donation and 38% of those who refused donation were no longer satisfied with their decision at the time the survey was conducted. Donor and non-donor satisfaction with their decision was predicted by more comfort and confidence during the decision-making process, more familiarity with the medical center, and a better understanding of brain death.
The current study has two primary aims: (1) to examine the instability of organ donation decisions made by next-of-kin, and (2) to identify factors that predict decision instability among non-donor next-of-kin. In their examination of issue, Burroughs et al.9 combined donors and non-donors in their analysis and, therefore, did not examine non-donor instability directly. Since non-donors who come to regret their decision represent a potential lost opportunity for the recovery of organs, we were mainly interested in examining predictors of decision instability in this subsample. We hypothesized, based on the Burroughs et al.9 study, that as many as 25% of study participants would report being dissatisfied or regretful of their organ donation decision, although non-donors would have a much higher level of decision instability than donors.
METHODS
Study Participants
Study participants were 285 next-of-kin (147 donors, 138 non-donors) who were approached by coordinators at LifeQuest Organ Recovery Services in Gainesville, Florida during a 4-year study period (July 2001 – February 2004). Each participant was paid $75.00.
Recruitment and Data Collection Procedures
The recruitment procedures and data collection strategies for this study are part of a larger study that examined multivariate predictors of organ donation decisions among next-of-kin. 4 In brief, during the study recruitment period, LifeQuest coordinators approached 680 families about organ donation, of which 456 were informed of the study and provided with a laminated card that further described the study purpose, procedures, and instructions on how to participate. Those interested in study participation or who wanted additional information about the study called the toll-free number on the card (n = 312). A trained research assistant answered questions, provided additional details about the study, and obtained verbal consent to conduct a comprehensive telephone interview for those interested in participating in the study. All 285 interviews were conducted by telephone. Some interviews were conducted immediately following verbal consent, while others were scheduled for a later date that was more convenient for the participants. Regardless, it was our intention to conduct the interviews as close in time as possible to the actual donation decision, to reduce the likelihood of interview responses being influenced by memory and decision justification processes over time. Consequently, the majority (76%) of interviews were done within 4 weeks of the donation decision.
The telephone interview was semi-structured in nature and research assistants worked from a detailed script, recording responses and using decision trees to progress through the questions. Interviews lasted 42 minutes, on average. We developed the interview questions and script on the basis of previous research, theoretical constructs, recommendations from the study’s advisory panel, and pilot studies by our research team.1,2,9,10 Items cut across 5 conceptual domains, including deceased, next-of-kin, and requestor characteristics, communication processes, and satisfaction with the healthcare team. In addition to questions within these conceptual domains, we asked study participants the following question: “Would you make the same donation decision if you had to make it again today?” Response choices were “Yes,” “No,” or “I don’t know.” This study was approved by the University of Florida Institutional Review Board.
Statistical Analysis
First, summary statistics were calculated for all variables. Second, bivariate analyses examined the relationship between donation decisions stability and deceased characteristics, next-of-kin characteristics, and other contextual variables. We used t-test for continuous variables, chi-square (χ2) test for variables with 3 or more categories, and Fisher’s exact test for variables with 2 categories. Finally, logistic regression analysis was used to examine multivariate predictors of regret for non-donor next-of-kin. Data were analyzed using the Statistical Package for the Social Sciences database (SPSS, Version 11, Chicago IL).
RESULTS
Sample Characteristics
Next-of-kin participants were predominantly middle aged (49.3±13.2 yrs), female (80%), white (78%), married (55%), and employed (59%). Most (77%) did not have a college education. Fifty-two percent self-identified as registered organ donors, which is comparable to the 52.7% reported in the 2005 National Public Opinion Survey on Organ Donation (www.organdonor.gov/survey2005). Their relationship to the deceased was spouse (36%), parent (26%), adult child (21%), sibling (10%), and other (7%). Mean length of time between death and next-of-kin study participation was 13.7±9.1 days (range: 1 to 68).
Stability of Donation Decision
Figure 1 highlights the stability of the donation decision for both next-of-kin donors and non-donors. Of the 147 next-of-kin donors, 138 (94%) would make the same decision again; 6 (4%) would now refuse donation, and 3 (2%) were unsure about the decision they would make now. Of the 138 next-of-kin non-donors, 89 (64%) would make the same decision again, 37 (27%) would now consent to donation, and 12 (9%) were unsure what decision they would make now. For subsequent analyses, these latter two groups were combined into one group that reflects non-donor instability or regret. Thirteen (27%) of the 49 next-of-kin who now would likely donate the organs of their deceased loved one initially refused to consent despite knowing that their loved one wanted to be an organ donor.
Figure 1.
Stability of donation decision for next-of-kin donors and non-donors.
Non-donors: Decision Stability and Association with Other Variables
Table 1 shows the variables that were significantly associated with decision instability for next-of-kin non-donors. Decision instability was more likely when the deceased had not previously discussed organ donation with the next-of-kin (p = 0.01) or with others (p = 0.001). Spouses (33.9%), adult children (46.4%), and especially others (mostly extended family members, 70%) were most likely to feel that they would now consent to donation if they could do it over again (p = 0.03). Decision instability was more likely for those who had more favorable attitudes toward transplantation (p = 0.001), poorer understanding of brain death (p = 0.002), and less exposure to organ donation via discussions with family members (p = 0.004), public service announcements (p = 0.003), or movies/television (p = 0.03).
Table 1.
Significant associations with donation decision instability for next-of-kin non-donors
| Make same decision again?€ | Fisher’s exact test, chi square (χ2) statistic, or t test ¶ |
|||
|---|---|---|---|---|
| Donation Decision Variables | Yes (n = 89) | No/Unsure (n = 49) | ||
| Characteristics of the deceased | ||||
| Previous donation discussion with next-of-kin | Yes | 41 (77.4) | 12 (22.6) | p = 0.01 |
| No | 48 (56.5) | 37(43.5) | ||
| Previous donation discussion with others | Yes | 22 (95.7) | 1 (4.3) | χ2 = 15.1, p = 0.001 |
| No | 38 (52.1) | 35 (47.9) | ||
| Don’t know | 29 (69.0) | 13 (31.0) | ||
| Next-of-kin characteristics | ||||
| Relationship to deceased | Spouse | 39 (66.1) | 20 (33.9) | χ2 = 11.0, p = 0.03 |
| Parent | 21 (84.0) | 4 (16.0) | ||
| Child | 15 (53.6) | 13 (46.4) | ||
| Sibling | 11 (68.8) | 5 (31.2) | ||
| Other | 3 (30.0) | 7 (70.0) | ||
| General transplant attitudes§ | 9.9±2.3 | 11.1±1.2 | t = 3.3, p = 0.001 | |
| Adequate knowledge of brain death | Yes | 30 (73.2) | 11 (26.8) | p = 0.002 |
| No | 21 (41.2) | 30 (58.8) | ||
| Important source of organ donation information in 6 months before loved one’s death | ||||
| Discussion with family members | Yes | 35 (81.4) | 8 (18.6) | p = 0.004 |
| No | 54 (56.8) | 41 (43.2) | ||
| Public service announcement | Yes | 39 (81.2) | 9 (18.8) | p = 0.003 |
| No | 50 (55.6) | 40 (44.4) | ||
| Movies or television | Yes | 37 (77.1) | 11 (22.9) | p = 0.03 |
| No | 52 (57.8) | 38 (42.2) | ||
| Requestor characteristics | ||||
| Person who 1st mentioned donation | OPO person | 10 (66.7) | 5 (33.3) | χ2 = 9.2, p = 0.01 |
| Non-OPO person | 61 (58.7) | 43 (41.3) | ||
| Family member | 18 (94.7) | 1 (5.3) | ||
| Communication processes | ||||
| Perceived timing of donation discussion | Timing was right | 48 (80.0) | 12 (20.0) | p = 0.001 |
| Timing was poor | 41 (52.6) | 37 (47.4) | ||
| Told of death before 1st mention of donation | Yes | 51 (82.3) | 11 (17.7) | p = 0.0001 |
| No | 38 (50.0) | 38 (50.0) | ||
| Given enough time to discuss donation decision | Yes | 63 (73.3) | 23 (26.7) | p = 0.006 |
| No | 26 (50.0) | 26 (50.0) | ||
| Satisfaction with healthcare team* | 40.2±6.1 | 37.6±8.3 | t = 2.1, p = 0.04 | |
Values expressed as no. (%) or mean ± standard deviation.
For Fisher’s exact test, only p values are calculated and reported; for chi square and t tests, both the test statistic and p value are calculated and reported.
Measured using 4-point Likert scale. Range = 4–16, with higher scores reflecting more positive attitudes toward transplantation.
Measured using 4-point Likert scale. Range = 14–56, with higher score indicating more satisfaction with the health care team.
Only one requestor characteristic was associated with decision stability. Next-of-kin non-donors were now more likely to consent to donation when the person who first mentioned donation at the time of their loved one’s death was a non-OPO professional, such as physician, nurse, clergy, or social worker (p = 0.01). Finally, decision instability was more likely when next-of-kin non-donors perceived the timing of the donation discussion to be poor (p = 0.001), were not told of their loved one’s death before the first mention of donation (p = 0.0001), and did not feel they were given enough time to discuss their donation decision with others (p = 0.006).
Multivariate Predictors of Decision Instability
Logistic regression analysis was used to examine the relative contribution of the deceased, next-of-kin, and requestor characteristics, deceased’s characteristics, next-of-kin characteristics, and communication processes in predicting decision instability in next-of-kin non-donors. This analysis included only those variables that were previously shown to be statistically associated with donation decision stability (Table 1). As highlighted in Table 2, the total regression model is statistically significant (p < 0.001). More favorable attitudes toward transplantation, having been exposed to donation messages via family discussion or public service announcements prior to the loved one’s death, the first mention of donation by a non-OPO coordinator, not being told of the loved one’s death prior to the first donation discussion, and the perception that the family was not given enough time to discuss donation were all significant predictors of decision instability among next-of-kin non-donors.
Table 2.
Summary of significant predictors of decision instability in logistic regression model
| Variables | Total Model | Individual Variables | |
|---|---|---|---|
| Chi-square | % correct prediction | OR (95% CI) | |
| 81.5*** | 81.9 | ||
| Favorable transplant attitudes | 1.76 (1.15, 2.69)*** | ||
| No next-of-kin donation discussion with family members in 6 months preceding death | 0.30 (0.13, 0.72)** | ||
| Next-of-kin had not heard donation PSA in 6 months preceding death | 0.29 (0.13, 0.67)* | ||
| Non-OPO 1st mention of donation | 0.21 (0.13, 0.65)*** | ||
| Not told of death before 1st donation discussion | 0.23 (0.10, 0.50)* | ||
| Felt family was not given enough time to discuss donation | 0.25 (0.11, 0.55)*** | ||
-2 Log Likelihood for the constant-only model was 72.5
p <0.05
p < 0.01
p < 0.001
DISCUSSION
The first aim of this study was to examine the stability of donation decisions made by next-of-kin. We found that in the weeks that follow an organ donation decision at the time of their loved one’s death, a sizable minority of next-of-kin (19%) are dissatisfied or regret the decision they made. Particularly striking is that more than one-third (36%) of non-donors now wish they had consented to organ donation or are questioning their original donation refusal. This finding is similar to the 39% reported by Burroughs et al.9 a decade ago and further highlights an opportunity for OPOs to learn from the non-donor’s decision and its aftermath.
It is of interest that 13 of the 49 (27%) next-of-kin who regret having refused donation had actually gone against the deceased’s favorable donation wishes at the time. We did not assess the psychological ramifications of donation decisions as part of this study, but several study participants told our interviewers that they regretted not following the decision their loved one had documented or shared with others, and that they were having difficulty coping with their decision. Legislation in most states now provide authorization for OPOs to remove organs from those who documented their donation intentions, even when family members are against organ donation. However, many OPOs continue to defer to the family if there are strong objections. Our data and anecdotal accounts suggest that a significant proportion of next-of-kin can be expected to regret their opposition to the deceased’s favorable donation intentions within a short time of their decision. Most of our interviews were conducted within a month of the donation decision so it is possible that an even higher proportion of next-of-kin may come to regret such decisions in the long run.
Decision instability was more likely when the deceased had not talked about organ donation with the next-of-kin or others, perhaps reflecting uncertainty about whether the donation refusal was consistent with the deceased’s wishes. Our data also indicate that next-of-kin who had not previously discussed organ donation with family members were more likely to regret their initial donation decision. One study participant (daughter) refused to donate organs despite the donor designation on her mother’s driver’s license. She reasoned that if organ donation was that important to her mother, she would have discussed it with her or another family member in some capacity. However, the daughter came to regret her decision because she feared that she had not supported her mother’s true donation intentions. Recently, we reported that family disagreement about organ donation was more likely when the deceased’s donation intentions were not known,11 and that such conflict could be attenuated by encouraging families to discuss organ donation before such decisions must be made.12–15 Together, these findings underscore the critical importance of discussing organ donation with others so that family members can feel more confident that the decision being made is consistent with the deceased’s intentions, whether formally documented or not.
Not surprisingly, higher decision instability was seen among those with more favorable attitudes toward transplantation. If you believe that there are many deserving people in need of organ transplantation, that organ transplantation helps to save lives, and that the organ allocation system is fair and equitable, then it may cause some decisional regret for next-of-kin who opted against organ donation. One of our participants (father) shared that he came to regret his refusal to donate his son’s organs because he learned later that a co-worker’s family member was on the waiting list for a liver transplant. He was having difficulty making sense of his donation refusal in the context of otherwise favorable attitudes toward transplantation and the more recent awareness of someone in need.
Results of the multivariate analyses identified 6 factors that were predictive of decision instability among those who refused donation. Favorable attitudes toward transplantation, the 1st mention of organ donation by someone other than an OPO representative, not being told of death before the first donation discussion, and feeling that the family did not have enough time to discuss donation were all strongly predictive of decision instability. In addition, next-of-kin had more regret about their donation refusal when they had not been exposed to organ donation via family discussions or public service announcements prior to the loved one’s death. All of these variables are modifiable in some way, which suggests that OPOs can work to prevent decision instability and possibly increase consent rates. Public education campaigns that highlight the benefits of transplantation and encourage organ donation discussions among family members are designed primarily to increase organ donation registrations. Yet, to the degree that these campaigns are successful in stimulating family discussions about organ donation, an important secondary benefit may be higher decision stability and satisfaction among next-of-kin decision makers.
Previous research has noted that next-of-kin are less likely to consent to organ donation when the non-OPO personnel first approach the family about donation and when the family feels that they did not have ample time to consider and discussion donation.1,4 Findings from the current study also suggest that these factors may trigger some regret about donation refusal. A few study participants told us that when they were first approached by someone from the medical institution (physician, nurse) rather than the OPO, they questioned whether every effort had been made to save the life of their loved one. This issue of medical distrust, in part, led them to refuse organ donation. In the ensuing weeks, however, they came to recognize or believe that the medical team had done all they could for their loved one and now questioned whether they should have consented to donation. Similar anecdotes were shared by those who felt they simply did not have enough time to process the death of their loved one and to contemplate the donation decision. Collectively, these findings suggest that when organ donation is first discussed with OPO representatives there is a higher likelihood of consent at the time of death and a lower likelihood of decision regret in the weeks that follow. Every effort should be made to ensure that representatives from the OPO are the first to discuss the organ donation option with family members and the ones who formally request consent, as this is consistent with the Centers for Medicare and Medicaid Services requirement and has been shown to facilitate an optimal donation request process.16,17 Also, perhaps more important than the actual time that the family has to make an informed decision is the perception that sufficient time has been given. OPO coordinators should ask family members if they feel that they have had ample time to discuss organ donation, which might be 15 minutes for some families and 48 hours for others.
The donation decision clearly was more stable among those who consented to donation – only 9 of 147 (6%) next-of-kin would now refuse donation or were unsure if they would make the same decision now. This finding contrasts sharply with Burroughs et al.,9 who found 14% of donor families to be dissatisfied with their decision. Although not part of our interview protocol, six study participants told our interviewers why they felt differently about organ donation now. One had subsequently learned from a family member that the deceased had not wanted to be an organ donor. Although the next-of-kin decision-maker (sister) had very favorable organ donation attitudes herself, she reported feeling badly that her decision may not have been consistent her brother’s wishes. Two participants (spouse, parent) were angry that they had not learned anything about whether the organs were successfully transplanted or who had received them. One participant (mother) expressed annoyance that she had not yet heard from the recipients of her son’s organs. Although it had only been 7 weeks since her son’s death, she felt that those who receive a life-saving organ transplant should write to the donor family as soon as possible because it helps with the grieving process and affirms that the right decision was made. This highlights the importance and benefit of recipient communication for some donor family members.18 Another participant (spouse) felt that the donation process was handled well, but subsequently he came to believe that some adults do not deserve transplantation (not elaborated upon). Finally, one woman (spouse) did not know her husband’s donation intentions, but decided to donate his organs despite objections from her minister. She believes now that this decision altered her relationship with the minister and she now wishes she had followed his advice. Pertinent to this latter experience, Burroughs et al.9 found that decision regret is more common among the more religious. Organ donation educational programs targeting faith-based organizations have the potential to attenuate the negative psychological effects of such regret.19
In general, adults employ cognitive processes that reinforce the preference for a chosen option, both before and after a final decision has been made.20 Despite these justification processes, however, post-decision regret is possible and may precipitate a “preference reversal” in which some next-of-kin come to favor the donation decision not chosen.21 Minimizing the regret of next-of-kin decision makers is an important issue for OPOs if the goal of achieving a “good decision” is to be realized. Decision making regret, whether consent for donation was granted or not, can potentially complicate the grieving process for next-of-kin and contribute to psychological distress. Indeed, previous research has shown that bereaved family members’ regret over end-of-life decisions for others can trigger intrusive thoughts that affect quality of life.22
There are several important limitations of the current study. First, we conducted most interviews within a short time of the donation decision, so this study focuses largely on short-term decision stability. It is possible that a different picture would emerge if next-of-kin had been interviewed months later. Second, we did not use a validated questionnaire to measure decision instability or regret. Questionnaires measuring regret have recently been developed and organ donation researchers who desire to investigate this construct should consider using or adapting one of these assessment tools.21,22 Third, since data for this study were gathered prior to participation in the Organ Donation Breakthrough Collaborative, the degree to which findings can be generalized to the current Collaborative era is unknown. Finally, we used a passive recruitment strategy that yielded a self-selected sample whose decision stability may not represent the larger population of next-of-kin decision makers. For instance, those who chose to take part in this study may have more decision instability than those chose not to participate, and may have been compelled to disclose this information as part of a research study. It is noteworthy, however, that the only two studies examining this topic, while using different methodologies in different regions of the country, found very similar rates of non-donor regret.
ACKNOWLEDGMENTS
We thank the following individuals for their assistance in the preparation and/or conduct of this study: Shawna Ehlers, Kristin Gant, Shannon Jackson, Ian Jamieson, William Kanasky, Jonathan Lin, Kathleen MacNaughton, Charles McCluskey, Stephen Oelrich, William Pfaff, Olivia Puyana, Joseph Riley, Stephanie Toy, and the National Donor Family Council of the National Kidney Foundation.
This research was supported, in part, by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK55706-01A2) awarded to the first author.
Footnotes
There are no conflicts of interest to report.
REFERENCES
- 1.Siminoff LA, Gordon N, Hewlett J, Arnold RM. Factors influencing families' consent for donation of solid organs for transplantation. JAMA. 2001;286:71–77. doi: 10.1001/jama.286.1.71. [DOI] [PubMed] [Google Scholar]
- 2.DeJong W, Franz HG, Wolfe SM, Nathan H, Payne D, Reitsma W, Beasley C. Requesting organ donation: an interview study of donor and nondonor families. Am J Crit Care. 1998;7:13–23. [PubMed] [Google Scholar]
- 3.Martinez JM, Lopez JS, Martin A, Martin MJ, Scandroglio B, Martin JM. Organ donation and family decision-making within the Spanish donation system. Soc Sci Med. 2001;53:405–421. doi: 10.1016/s0277-9536(00)00345-2. [DOI] [PubMed] [Google Scholar]
- 4.Rodrigue JR, Cornell DL, Howard RJ. Organ donation decision: comparison of donor and nondonor families. Am J Transplant. 2006;6:190–198. doi: 10.1111/j.1600-6143.2005.01130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodrigue JR, Cornell DL, Howard RJ. Pediatric organ donation: what factors most influence parents' donation decisions? Pediatr Crit Care Med. 2008;9:180–185. doi: 10.1097/PCC.0b013e3181668605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sque M, Long T, Payne S. Organ donation: key factors influencing families' decisionmaking. Transplant Proc. 2005;37:543–546. doi: 10.1016/j.transproceed.2004.11.038. [DOI] [PubMed] [Google Scholar]
- 7.Shafer TJ, Wagner D, Chessare J, Zampiello FA, McBride V, Perdue J. Organ donation breakthrough collaborative: increasing organ donation through system redesign. Crit Care Nurse. 2006;26:33–48. [PubMed] [Google Scholar]
- 8.Howard DH, Siminoff LA, McBride V, Lin M. Does quality improvement work? Evaluation of the Organ Donation Breakthrough Collaborative. Health Serv Res. 2007;42:2160–2173. doi: 10.1111/j.1475-6773.2007.00732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burroughs TE, Hong BA, Kappel DF, Freedman BK. The stability of family decisions to consent or refuse organ donation: would you do it again? Psychosom Med. 1998;60:156–162. doi: 10.1097/00006842-199803000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Radecki CM, Jaccard J. Psychological aspects of organ donation: a critical review and synthesis of individual and next-of-kin donation decisions. Health Psychol. 1997;16:183–195. doi: 10.1037//0278-6133.16.2.183. [DOI] [PubMed] [Google Scholar]
- 11.Rodrigue JR, Cornell DL, Howard RJ. Does family disagreement affect donation decisions by next-of-kin? Prog Transplant. doi: 10.1177/152692480801800306. In press. [DOI] [PubMed] [Google Scholar]
- 12.Guadagnoli E, Christiansen CL, DeJong W, et al. The public's willingness to discuss their preference for organ donation with family members. Clin Transplant. 1999;13:342–348. doi: 10.1034/j.1399-0012.1999.130411.x. [DOI] [PubMed] [Google Scholar]
- 13.Morgan SE, Miller JK. Beyond the organ donor card: the effect of knowledge, attitudes, and values on willingness to communicate about organ donation to family members. Health Commun. 2002;14:121–134. doi: 10.1207/S15327027HC1401_6. [DOI] [PubMed] [Google Scholar]
- 14.Smith SW, Kopfman JE, Lindsey LL, Yoo J, Morrison K. Encouraging family discussion on the decision to donate organs: the role of the willingness to communicate scale. Health Commun. 2004;16:333–346. doi: 10.1207/S15327027HC1603_4. [DOI] [PubMed] [Google Scholar]
- 15.Thompson TL, Robinson JD, Kenny RW. Family conversations about organ donation. Prog Transplant. 2004;14:49–55. doi: 10.1177/152692480401400108. [DOI] [PubMed] [Google Scholar]
- 16.Shafer T, Wood RP, Van Buren C, Guerriero W, Davis K, Sullivan H, et al. An in-house coordinator program to increase organ donation in public trauma hospitals. J Transpl Coord. 1998;8:82–87. doi: 10.7182/prtr.1.8.2.w256r778xw724430. [DOI] [PubMed] [Google Scholar]
- 17.Shafer TJ, Davis KD, Holtzman SM, Van Buren CT, Crafts NJ, Durand R. Location of inhouse organ procurement organization staff in level I trauma centers increases conversion of potential donors to actual donors. Transplantation. 2003;75:1330–1335. doi: 10.1097/01.TP.0000060532.70301.32. [DOI] [PubMed] [Google Scholar]
- 18.National Kidney Foundation. Writing to Donor Families and Living Donors: A Simple Guide for Organ and Tissue Transplant Recipients. New York, NY: National Kidney Foundation; 2004. [Google Scholar]
- 19.Arriola KR, Perryman JP, Doldren MA, Warren CM, Robinson DH. Understanding the role of clergy in African American organ and tissue donation decision-making. Ethn Health. 2007;12:465–482. doi: 10.1080/13557850701616896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Svenson O. Differentiation and consolidation theory of human decision making: a frame of reference for the study of pre- and postdecision processes. Acta Psychol. 1992;80:143–168. [Google Scholar]
- 21.Brehaut JC, O'Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E, Feldman-Stewart D. Validation of a decision regret scale. Med Decis Making. 2003;23:281–292. doi: 10.1177/0272989X03256005. [DOI] [PubMed] [Google Scholar]
- 22.Shiozaki M, Hirai K, Dohke R, et al. Measuring the regret of bereaved family members regarding the decision to admit cancer patients to palliative care units. Psychooncology. doi: 10.1002/pon.1312. In press. [DOI] [PubMed] [Google Scholar]