Abstract
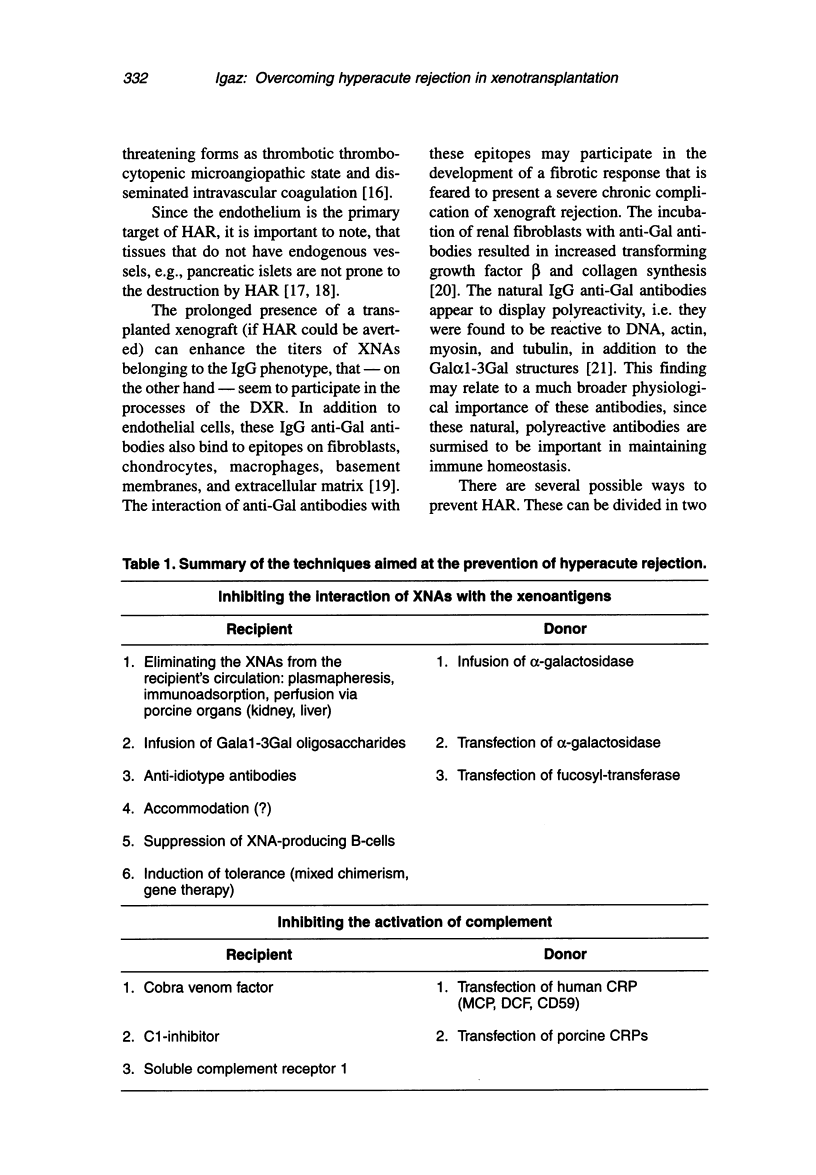
Due to the ever increasing shortage of suitable human donors, alternative strategies are sought to moderate the current discrepancy between the number of executable and required transplantations. Xenotransplantation (i.e., the transplantation of organs [tissues or cells] between different species) appears to be a reasonable solution. However, various problems (immunological, physiological, infectious-microbiological, ethical-juridicial) seem to be associated with xenotransplantation. One of the most formidable barriers to xenotransplantation is the phenomenon of hyperacute rejection that may lead to the destruction of the transplanted vascularized organ in a few minutes to hours. In the pathogenesis of hyperacute rejection, xenoreactive antibodies and the complement system appear to be of primary importance. Various methods can be applied to prevent hyperacute rejection; both the recipient and the donor can be treated. In this brief review, the author attempts to present a synopsis of the possible therapeutical interventions to prevent hyperacute rejection..
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bach F. H., Turman M. A., Vercellotti G. M., Platt J. L., Dalmasso A. P. Accommodation: a working paradigm for progressing toward clinical discordant xenografting. Transplant Proc. 1991 Feb;23(1 Pt 1):205–207. [PubMed] [Google Scholar]
- Begum N. A., Murakami Y., Mikata S., Matsumoto M., Hatanaka M., Nagasawa S., Kinoshita T., Seya T. Molecular remodelling of human CD46 for xenotransplantation: designing a potent complement regulator without measles virus receptor activity. Immunology. 2000 May;100(1):131–139. doi: 10.1046/j.1365-2567.2000.00999.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergelson J. M., Chan M., Solomon K. R., St John N. F., Lin H., Finberg R. W. Decay-accelerating factor (CD55), a glycosylphosphatidylinositol-anchored complement regulatory protein, is a receptor for several echoviruses. Proc Natl Acad Sci U S A. 1994 Jun 21;91(13):6245–6248. doi: 10.1073/pnas.91.13.6245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bracy J. L., Sachs D. H., Iacomini J. Inhibition of xenoreactive natural antibody production by retroviral gene therapy. Science. 1998 Sep 18;281(5384):1845–1847. doi: 10.1126/science.281.5384.1845. [DOI] [PubMed] [Google Scholar]
- Brenner P., Reichenspurner H., Schmoeckel M., Wimmer C., Rucker A., Eder V., Meiser B., Hinz M., Felbinger T., Müller-Höcker J. IG-therasorb immunoapheresis in orthotopic xenotransplantation of baboons with landrace pig hearts. Transplantation. 2000 Jan 27;69(2):208–214. doi: 10.1097/00007890-200001270-00003. [DOI] [PubMed] [Google Scholar]
- Byrne G. W., McCurry K. R., Martin M. J., McClellan S. M., Platt J. L., Logan J. S. Transgenic pigs expressing human CD59 and decay-accelerating factor produce an intrinsic barrier to complement-mediated damage. Transplantation. 1997 Jan 15;63(1):149–155. doi: 10.1097/00007890-199701150-00027. [DOI] [PubMed] [Google Scholar]
- Bühler L., Basker M., Alwayn I. P., Goepfert C., Kitamura H., Kawai T., Gojo S., Kozlowski T., Ierino F. L., Awwad M. Coagulation and thrombotic disorders associated with pig organ and hematopoietic cell transplantation in nonhuman primates. Transplantation. 2000 Nov 15;70(9):1323–1331. doi: 10.1097/00007890-200011150-00010. [DOI] [PubMed] [Google Scholar]
- Carrington C. A., Richards A. C., van den Bogaerde J., Tucker A. W., White D. J. Complement activation, its consequences, and blockade by gene transfer. World J Surg. 1997 Nov-Dec;21(9):907–912. doi: 10.1007/s002689900325. [DOI] [PubMed] [Google Scholar]
- Cozzi E., Bhatti F., Schmoeckel M., Chavez G., Smith K. G., Zaidi A., Bradley J. R., Thiru S., Goddard M., Vial C. Long-term survival of nonhuman primates receiving life-supporting transgenic porcine kidney xenografts. Transplantation. 2000 Jul 15;70(1):15–21. [PubMed] [Google Scholar]
- Dalmasso A. P., Benson B. A., Johnson J. S., Lancto C., Abrahamsen M. S. Resistance against the membrane attack complex of complement induced in porcine endothelial cells with a Gal alpha(1-3)Gal binding lectin: up-regulation of CD59 expression. J Immunol. 2000 Apr 1;164(7):3764–3773. doi: 10.4049/jimmunol.164.7.3764. [DOI] [PubMed] [Google Scholar]
- Dalmasso A. P., Platt J. L. Potentiation of C1 inhibitor plus heparin in prevention of complement-mediated activation of endothelial cells in a model of xenograft hyperacute rejection. Transplant Proc. 1994 Jun;26(3):1246–1247. [PubMed] [Google Scholar]
- Deckert M., Kubar J., Zoccola D., Bernard-Pomier G., Angelisova P., Horejsi V., Bernard A. CD59 molecule: a second ligand for CD2 in T cell adhesion. Eur J Immunol. 1992 Nov;22(11):2943–2947. doi: 10.1002/eji.1830221128. [DOI] [PubMed] [Google Scholar]
- Galili U. Interaction of the natural anti-Gal antibody with alpha-galactosyl epitopes: a major obstacle for xenotransplantation in humans. Immunol Today. 1993 Oct;14(10):480–482. doi: 10.1016/0167-5699(93)90261-i. [DOI] [PubMed] [Google Scholar]
- Goddard M. J., Foweraker J. E., Wallwork J. Xenotransplantation--2000. J Clin Pathol. 2000 Jan;53(1):44–48. doi: 10.1136/jcp.53.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gojo S., Bartholomew A., Xu Y., Neethling F. A., Awwad M., Saidman S., Cosimi A. B., Cooper D. K. Anti-Galalpha1-3Gal antibody levels in organ transplant recipients receiving immunosuppressive therapy. Transplantation. 2000 Mar 15;69(5):914–917. doi: 10.1097/00007890-200003150-00042. [DOI] [PubMed] [Google Scholar]
- Hamann J., Vogel B., van Schijndel G. M., van Lier R. A. The seven-span transmembrane receptor CD97 has a cellular ligand (CD55, DAF). J Exp Med. 1996 Sep 1;184(3):1185–1189. doi: 10.1084/jem.184.3.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinchliffe S. J., Rushmere N. K., Hanna S. M., Morgan B. P. Molecular cloning and functional characterization of the pig analogue of CD59: relevance to xenotransplantation. J Immunol. 1998 Apr 15;160(8):3924–3932. [PubMed] [Google Scholar]
- Joziasse D. H., Oriol R. Xenotransplantation: the importance of the Galalpha1,3Gal epitope in hyperacute vascular rejection. Biochim Biophys Acta. 1999 Oct 8;1455(2-3):403–418. doi: 10.1016/s0925-4439(99)00056-3. [DOI] [PubMed] [Google Scholar]
- Kopp C. W., Siegel J. B., Hancock W. W., Anrather J., Winkler H., Geczy C. L., Kaczmarek E., Bach F. H., Robson S. C. Effect of porcine endothelial tissue factor pathway inhibitor on human coagulation factors. Transplantation. 1997 Mar 15;63(5):749–758. doi: 10.1097/00007890-199703150-00023. [DOI] [PubMed] [Google Scholar]
- Koren E., Milotic F., Neethling F. A., Koscec M., Fei D., Kobayashi T., Taniguchi S., Cooper D. K. Monoclonal antiidiotypic antibodies neutralize cytotoxic effects of anti-alphaGal antibodies. Transplantation. 1996 Sep 27;62(6):837–843. doi: 10.1097/00007890-199609270-00023. [DOI] [PubMed] [Google Scholar]
- Kozlowski T., Monroy R., Xu Y., Glaser R., Awwad M., Cooper D. K., Sachs D. H. Anti-Gal(alpha)1-3Gal antibody response to porcine bone marrow in unmodified baboons and baboons conditioned for tolerance induction. Transplantation. 1998 Jul 27;66(2):176–182. doi: 10.1097/00007890-199807270-00006. [DOI] [PubMed] [Google Scholar]
- Kroshus T. J., Salerno C. T., Yeh C. G., Higgins P. J., Bolman R. M., 3rd, Dalmasso A. P. A recombinant soluble chimeric complement inhibitor composed of human CD46 and CD55 reduces acute cardiac tissue injury in models of pig-to-human heart transplantation. Transplantation. 2000 Jun 15;69(11):2282–2289. doi: 10.1097/00007890-200006150-00011. [DOI] [PubMed] [Google Scholar]
- Lawson J. H., Daniels L. J., Platt J. L. The evaluation of thrombomodulin activity in porcine to human xenotransplantation. Transplant Proc. 1997 Feb-Mar;29(1-2):884–885. doi: 10.1016/s0041-1345(96)00192-3. [DOI] [PubMed] [Google Scholar]
- Lin Y., Soares M. P., Sato K., Csizmadia E., Robson S. C., Smith N., Bach F. H. Long-term survival of hamster hearts in presensitized rats. J Immunol. 2000 May 1;164(9):4883–4892. doi: 10.4049/jimmunol.164.9.4883. [DOI] [PubMed] [Google Scholar]
- Loss M., Kunz R., Przemeck M., Schmidtko J., Arends H., Jalali A., Lorenz R., Piepenbrock S., Klempnauer J., Winkler M. Influence of cold ischemia time, pretransplant anti-porcine antibodies, and donor/recipient size matching on hyperacute graft rejection after discordant porcine to cynomolgus kidney transplantation. Transplantation. 2000 Mar 27;69(6):1155–1159. doi: 10.1097/00007890-200003270-00021. [DOI] [PubMed] [Google Scholar]
- Maher S. E., Pflugh D. L., Larsen N. J., Rothschild M. F., Bothwell A. L. Structure/function characterization of porcine CD59: expression, chromosomal mapping, complement-inhibition, and costimulatory activity. Transplantation. 1998 Oct 27;66(8):1094–1100. doi: 10.1097/00007890-199810270-00021. [DOI] [PubMed] [Google Scholar]
- Maisner A., Schneider-Schaulies J., Liszewski M. K., Atkinson J. P., Herrler G. Binding of measles virus to membrane cofactor protein (CD46): importance of disulfide bonds and N-glycans for the receptor function. J Virol. 1994 Oct;68(10):6299–6304. doi: 10.1128/jvi.68.10.6299-6304.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruyama S., Cantu E., 3rd, DeMartino C., Wang C. Y., Chen J., Al-Mohanna F., Nakeeb S. M., D'Agati V., Pernis B., Galili U. Interaction of baboon anti-alpha-galactosyl antibody with pig tissues. Am J Pathol. 1999 Nov;155(5):1635–1649. doi: 10.1016/s0002-9440(10)65479-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruyama S., Cantu E., 3rd, Galili U., D'Agati V., Godman G., Stern D. M., Andres G. alpha-galactosyl epitopes on glycoproteins of porcine renal extracellular matrix. Kidney Int. 2000 Feb;57(2):655–663. doi: 10.1046/j.1523-1755.2000.00887.x. [DOI] [PubMed] [Google Scholar]
- Ogawa H., Muramatsu H., Kobayashi T., Morozumi K., Yokoyama I., Kurosawa N., Nakao A., Muramatsu T. Molecular cloning of endo-beta -galactosidase C and its application in removing alpha -galactosyl xenoantigen from blood vessels in the pig kidney. J Biol Chem. 2000 Jun 23;275(25):19368–19374. doi: 10.1074/jbc.M001888200. [DOI] [PubMed] [Google Scholar]
- Ohdan H., Yang Y. G., Swenson K. G., Kitamura H., Sykes M. T cell and B cell tolerance to GALalpha1,3GAL-expressing heart xenografts is achieved in alpha1,3-galactosyltransferase-deficient mice by nonmyeloablative induction of mixed chimerism. Transplantation. 2001 Jun 15;71(11):1532–1542. doi: 10.1097/00007890-200106150-00009. [DOI] [PubMed] [Google Scholar]
- Onishi A., Iwamoto M., Akita T., Mikawa S., Takeda K., Awata T., Hanada H., Perry A. C. Pig cloning by microinjection of fetal fibroblast nuclei. Science. 2000 Aug 18;289(5482):1188–1190. doi: 10.1126/science.289.5482.1188. [DOI] [PubMed] [Google Scholar]
- Patience C., Takeuchi Y., Weiss R. A. Infection of human cells by an endogenous retrovirus of pigs. Nat Med. 1997 Mar;3(3):282–286. doi: 10.1038/nm0397-282. [DOI] [PubMed] [Google Scholar]
- Platt J. L. Approaching the clinical application of xenotransplantation. Am J Med Sci. 1997 May;313(5):315–321. doi: 10.1097/00000441-199705000-00012. [DOI] [PubMed] [Google Scholar]
- Platt J. L., Lin S. S., McGregor C. G. Acute vascular rejection. Xenotransplantation. 1998 Aug;5(3):169–175. doi: 10.1111/j.1399-3089.1998.tb00024.x. [DOI] [PubMed] [Google Scholar]
- Platt J. L., Saadi S. The role of complement in transplantation. Mol Immunol. 1999 Sep-Oct;36(13-14):965–971. doi: 10.1016/s0161-5890(99)00119-4. [DOI] [PubMed] [Google Scholar]
- Polejaeva I. A., Chen S. H., Vaught T. D., Page R. L., Mullins J., Ball S., Dai Y., Boone J., Walker S., Ayares D. L. Cloned pigs produced by nuclear transfer from adult somatic cells. Nature. 2000 Sep 7;407(6800):86–90. doi: 10.1038/35024082. [DOI] [PubMed] [Google Scholar]
- Pruitt S. K., Kirk A. D., Bollinger R. R., Marsh H. C., Jr, Collins B. H., Levin J. L., Mault J. R., Heinle J. S., Ibrahim S., Rudolph A. R. The effect of soluble complement receptor type 1 on hyperacute rejection of porcine xenografts. Transplantation. 1994 Feb;57(3):363–370. doi: 10.1097/00007890-199402150-00009. [DOI] [PubMed] [Google Scholar]
- Sablinski T., Emery D. W., Monroy R., Hawley R. J., Xu Y., Gianello P., Lorf T., Kozlowski T., Bailin M., Cooper D. K. Long-term discordant xenogeneic (porcine-to-primate) bone marrow engraftment in a monkey treated with porcine-specific growth factors. Transplantation. 1999 Apr 15;67(7):972–977. doi: 10.1097/00007890-199904150-00007. [DOI] [PubMed] [Google Scholar]
- Sachs D. H. Mixed chimerism as an approach to transplantation tolerance. Clin Immunol. 2000 Apr;95(1 Pt 2):S63–S68. doi: 10.1006/clim.1999.4814. [DOI] [PubMed] [Google Scholar]
- Satapathy A. K., Ravindran B. Naturally occurring alpha-galactosyl antibodies in human sera display polyreactivity. Immunol Lett. 1999 Sep 1;69(3):347–351. doi: 10.1016/s0165-2478(99)00116-9. [DOI] [PubMed] [Google Scholar]
- Schulte am Esch J., 2nd, Cruz M. A., Siegel J. B., Anrather J., Robson S. C. Activation of human platelets by the membrane-expressed A1 domain of von Willebrand factor. Blood. 1997 Dec 1;90(11):4425–4437. [PubMed] [Google Scholar]
- Shafren D. R., Dorahy D. J., Ingham R. A., Burns G. F., Barry R. D. Coxsackievirus A21 binds to decay-accelerating factor but requires intercellular adhesion molecule 1 for cell entry. J Virol. 1997 Jun;71(6):4736–4743. doi: 10.1128/jvi.71.6.4736-4743.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafren D. R., Williams D. T., Barry R. D. A decay-accelerating factor-binding strain of coxsackievirus B3 requires the coxsackievirus-adenovirus receptor protein to mediate lytic infection of rhabdomyosarcoma cells. J Virol. 1997 Dec;71(12):9844–9848. doi: 10.1128/jvi.71.12.9844-9848.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinkel T. A., Chen C. G., Salvaris E., Henion T. R., Barlow H., Galili U., Pearse M. J., d'Apice A. J. Changes in cell surface glycosylation in alpha1,3-galactosyltransferase knockout and alpha1,2-fucosyltransferase transgenic mice. Transplantation. 1997 Jul 27;64(2):197–204. doi: 10.1097/00007890-199707270-00003. [DOI] [PubMed] [Google Scholar]
- Simeonovic C. J. Xenogeneic islet transplantation. Xenotransplantation. 1999 Feb;6(1):1–5. doi: 10.1034/j.1399-3089.1999.00003.x. [DOI] [PubMed] [Google Scholar]
- Simon A. R., Warrens A. N., Yazzie N. P., Seebach J. D., Sachs D. H., Sykes M. Cross-species interaction of porcine and human integrins with their respective ligands: implications for xenogeneic tolerance induction. Transplantation. 1998 Aug 15;66(3):385–394. doi: 10.1097/00007890-199808150-00017. [DOI] [PubMed] [Google Scholar]
- Simon P. M., Neethling F. A., Taniguchi S., Goode P. L., Zopf D., Hancock W. W., Cooper D. K. Intravenous infusion of Galalpha1-3Gal oligosaccharides in baboons delays hyperacute rejection of porcine heart xenografts. Transplantation. 1998 Feb 15;65(3):346–353. doi: 10.1097/00007890-199802150-00009. [DOI] [PubMed] [Google Scholar]
- Smith R. M., Mandel T. E. Pancreatic islet xenotransplantation: the potential for tolerance induction. Immunol Today. 2000 Jan;21(1):42–48. doi: 10.1016/s0167-5699(99)01554-6. [DOI] [PubMed] [Google Scholar]
- Soin B., Vial C. M., Friend P. J. Xenotransplantation. Br J Surg. 2000 Feb;87(2):138–148. doi: 10.1046/j.1365-2168.2000.01351.x. [DOI] [PubMed] [Google Scholar]
- Steele D. J., Auchincloss H., Jr Xenotransplantation. Annu Rev Med. 1995;46:345–360. doi: 10.1146/annurev.med.46.1.345. [DOI] [PubMed] [Google Scholar]
- Stoye J. P., Le Tissier P., Takeuchi Y., Patience C., Weiss R. A. Endogenous retroviruses: a potential problem for xenotransplantation? Ann N Y Acad Sci. 1998 Dec 30;862:67–74. doi: 10.1111/j.1749-6632.1998.tb09118.x. [DOI] [PubMed] [Google Scholar]
- Taniguchi S., Kobayashi T., Neethling F. A., Ye Y., Niekrasz M., White D. J., Cooper D. K. Cobra venom factor stimulates anti-alpha-galactose antibody production in baboons. Implications for pig-to-human xenotransplantation. Transplantation. 1996 Sep 15;62(5):678–681. doi: 10.1097/00007890-199609150-00024. [DOI] [PubMed] [Google Scholar]
- Tearle R. G., Tange M. J., Zannettino Z. L., Katerelos M., Shinkel T. A., Van Denderen B. J., Lonie A. J., Lyons I., Nottle M. B., Cox T. The alpha-1,3-galactosyltransferase knockout mouse. Implications for xenotransplantation. Transplantation. 1996 Jan 15;61(1):13–19. doi: 10.1097/00007890-199601150-00004. [DOI] [PubMed] [Google Scholar]
- Warrens A. N., Simon A. R., Theodore P. R., Sachs D. H., Sykes M. Cross-species compatibility of intercellular adhesion molecule-1 (CD54) with its ligands. Transplantation. 2000 Feb 15;69(3):394–399. doi: 10.1097/00007890-200002150-00015. [DOI] [PubMed] [Google Scholar]
- Weiss R. A. Xenotransplantation. BMJ. 1998 Oct 3;317(7163):931–934. doi: 10.1136/bmj.317.7163.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wekerle T., Sykes M. Mixed chimerism and transplantation tolerance. Annu Rev Med. 2001;52:353–370. doi: 10.1146/annurev.med.52.1.353. [DOI] [PubMed] [Google Scholar]
- White S. A., Nicholson M. L. Xenotransplantation. Br J Surg. 1999 Dec;86(12):1499–1514. doi: 10.1046/j.1365-2168.1999.01340.x. [DOI] [PubMed] [Google Scholar]
- Yang Y. G., deGoma E., Ohdan H., Bracy J. L., Xu Y., Iacomini J., Thall A. D., Sykes M. Tolerization of anti-Galalpha1-3Gal natural antibody-forming B cells by induction of mixed chimerism. J Exp Med. 1998 Apr 20;187(8):1335–1342. doi: 10.1084/jem.187.8.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu A. Binding of human natural antibodies to nonalphaGal xenoantigens on porcine erythrocytes. Transplantation. 2000 Jun 15;69(11):2422–2428. doi: 10.1097/00007890-200006150-00036. [DOI] [PubMed] [Google Scholar]
- van den Berg C. W., Morgan B. P. Complement-inhibiting activities of human CD59 and analogues from rat, sheep, and pig are not homologously restricted. J Immunol. 1994 Apr 15;152(8):4095–4101. [PubMed] [Google Scholar]
- van den Berg C. W., Pérez de la Lastra J. M., Llanes D., Morgan B. P. Purification and characterization of the pig analogue of human membrane cofactor protein (CD46/MCP). J Immunol. 1997 Feb 15;158(4):1703–1709. [PubMed] [Google Scholar]


