Abstract
There are multiple sites at which the brachial plexus block can be induced in selecting regional anesthesia for upper extremity surgical patients. The most frequently used blocks are axillary, infraclavicular, supraclavicular, and interscalene. One must understand brachial plexus anatomy to use these blocks effectively, as well as the practical clinical differences between the blocks. Axillary brachial plexus block is most effective for surgical procedures distal to the elbow. This block is induced at a distance from both the centroneuraxis and the lung; thus, complications in those areas are avoided. Infraclavicular block is often the most effective method of maintaining a continuous block of the brachial plexus, since the catheter is easily secured to the anterior chest. Supraclavicular block provides anesthesia of the entire upper extremity in the most consistent, time-efficient manner of any brachial plexus technique; however, the block needle is necessarily positioned near the lung during injection. Interscalene block is especially effective for surgical procedures involving the shoulder or upper arm because the roots of the brachial plexus are most easily blocked with this technique. The final needle tip position with this block is potentially near the centroneuraxis and arteries perfusing the brain, thus careful aspiration of the needle and incremental injection are important. In summary, when an understanding of branchial plexus anatomy is combined with proper block technique and a patient- and procedure-specific balancing of risk-benefit, our patients and colleagues will be coadvocates of our branchial plexus regional blocks.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown D. L., Cahill D. R., Bridenbaugh L. D. Supraclavicular nerve block: anatomic analysis of a method to prevent pneumothorax. Anesth Analg. 1993 Mar;76(3):530–534. doi: 10.1213/00000539-199303000-00013. [DOI] [PubMed] [Google Scholar]
- DE JONG R. H. Axillary block of the brachial plexus. Anesthesiology. 1961 Mar-Apr;22:215–225. doi: 10.1097/00000542-196103000-00010. [DOI] [PubMed] [Google Scholar]
- DeKrey J. A., Schroeder C. F., Buechel D. R. Continuous brachial plexus block. Anesthesiology. 1969 Mar;30(3):332–332. [PubMed] [Google Scholar]
- Lanz E., Theiss D., Jankovic D. The extent of blockade following various techniques of brachial plexus block. Anesth Analg. 1983 Jan;62(1):55–58. [PubMed] [Google Scholar]
- Lavoie J., Martin R., Tétrault J. P., Côté D. J., Colas M. J. Axillary plexus block using a peripheral nerve stimulator: single or multiple injections. Can J Anaesth. 1992 Jul;39(6):583–586. doi: 10.1007/BF03008322. [DOI] [PubMed] [Google Scholar]
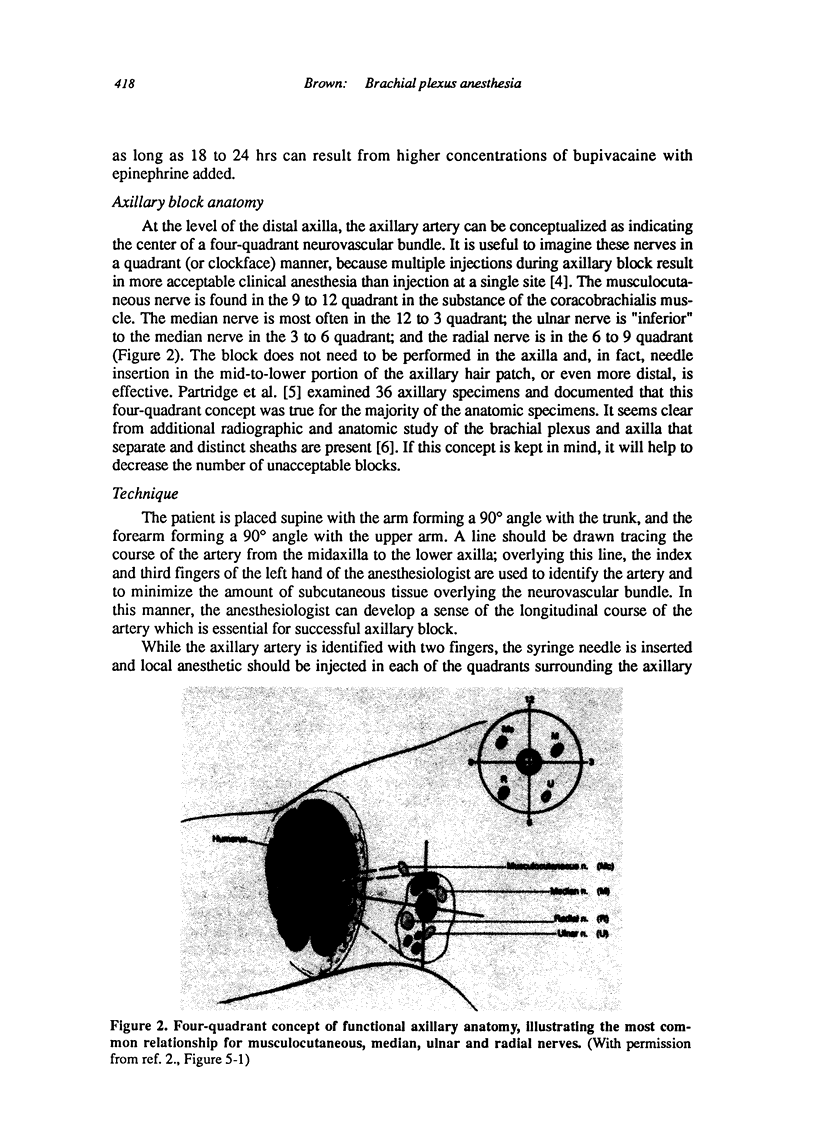
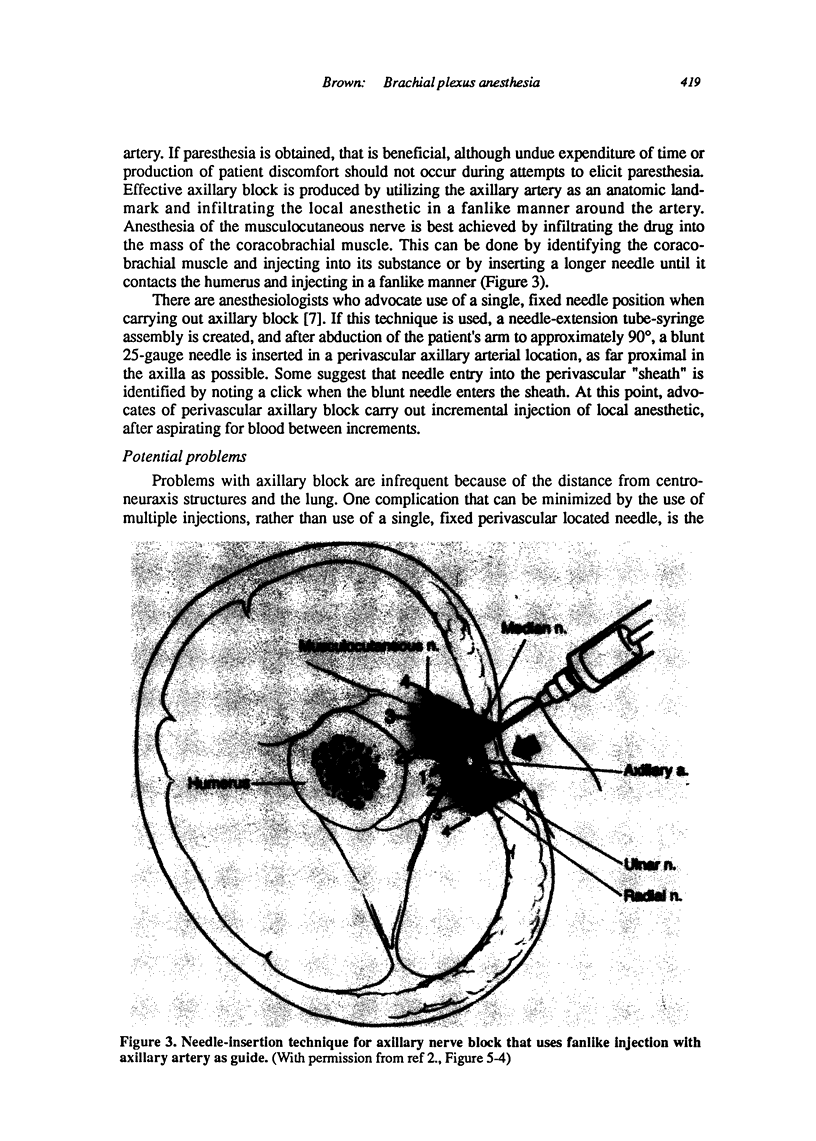
- Partridge B. L., Katz J., Benirschke K. Functional anatomy of the brachial plexus sheath: implications for anesthesia. Anesthesiology. 1987 Jun;66(6):743–747. doi: 10.1097/00000542-198706000-00006. [DOI] [PubMed] [Google Scholar]
- Peterson D. O. Shoulder block anesthesia for shoulder reconstruction surgery. Anesth Analg. 1985 Mar;64(3):373–375. [PubMed] [Google Scholar]
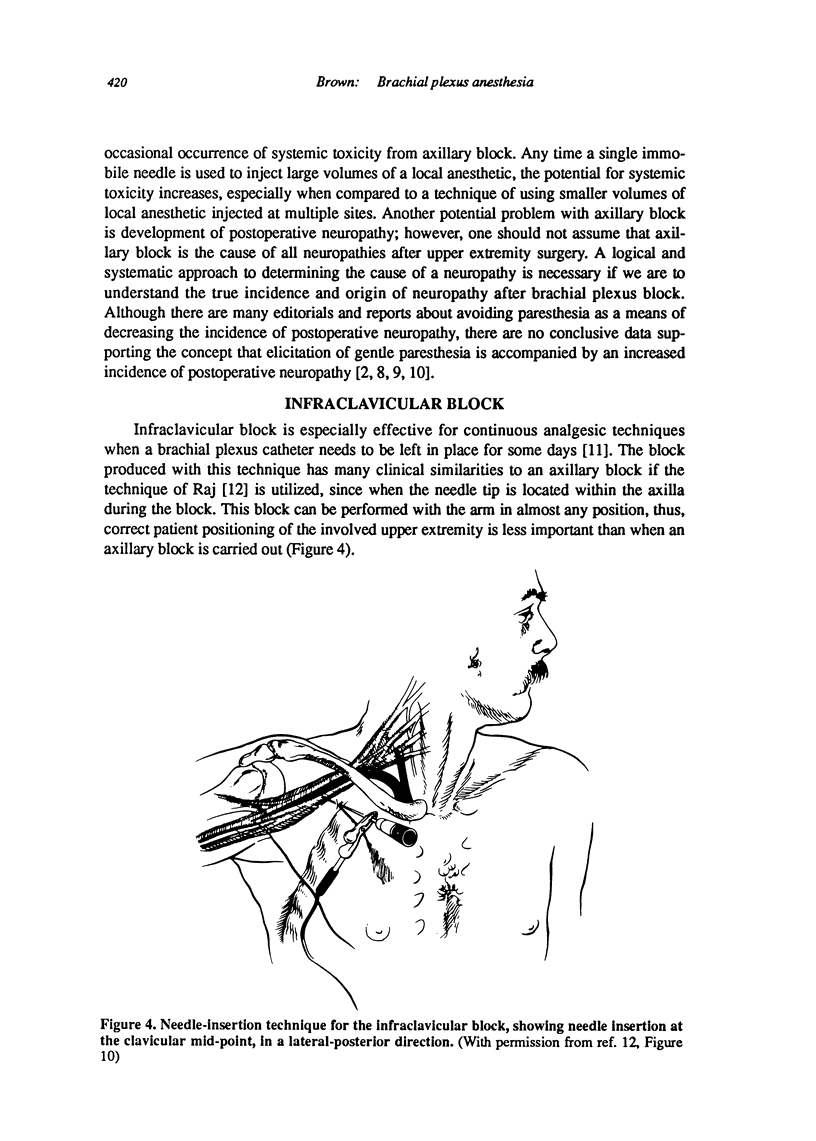
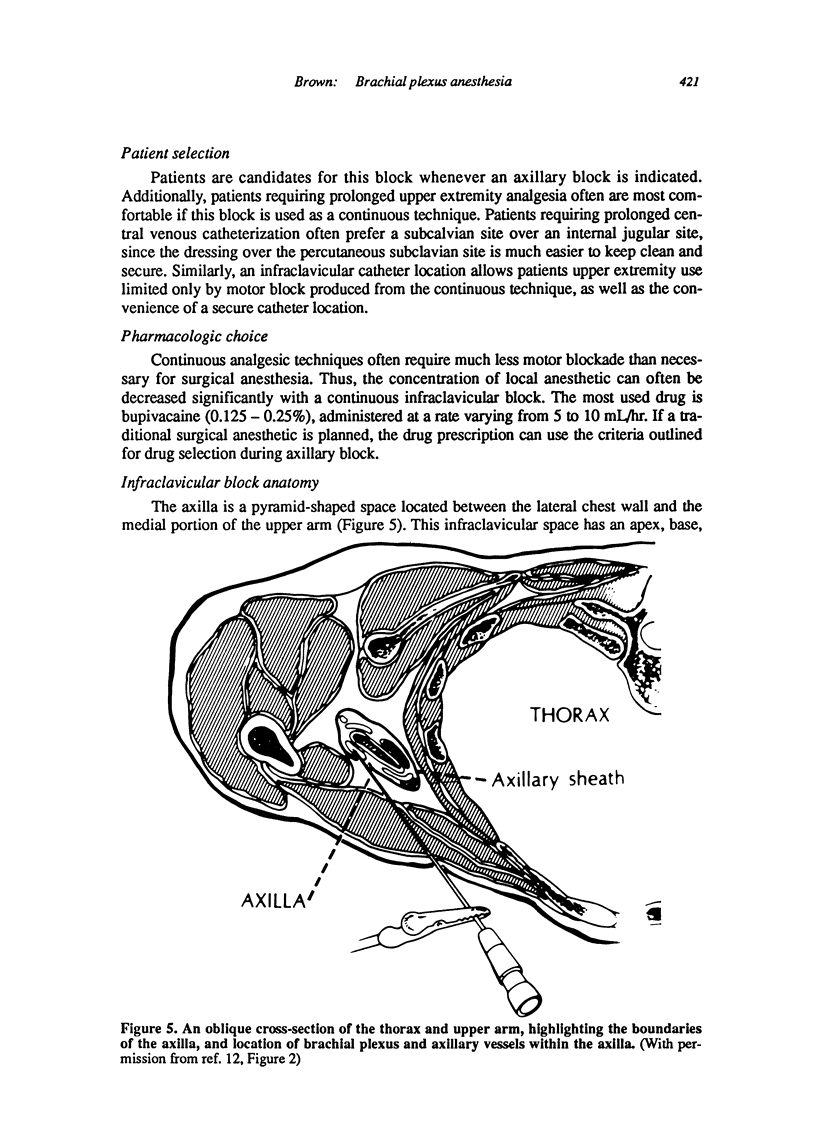
- Raj P. P., Montgomery S. J., Nettles D., Jenkins M. T. Infraclavicular brachial plexus block--a new approach. Anesth Analg. 1973 Nov-Dec;52(6):897–904. [PubMed] [Google Scholar]
- Selander D. Axillary plexus block: paresthetic or perivascular. Anesthesiology. 1987 Jun;66(6):726–728. [PubMed] [Google Scholar]
- Selander D., Edshage S., Wolff T. Paresthesiae or no paresthesiae? Nerve lesions after axillary blocks. Acta Anaesthesiol Scand. 1979 Feb;23(1):27–33. doi: 10.1111/j.1399-6576.1979.tb01417.x. [DOI] [PubMed] [Google Scholar]
- Thompson G. E., Rorie D. K. Functional anatomy of the brachial plexus sheaths. Anesthesiology. 1983 Aug;59(2):117–122. doi: 10.1097/00000542-198308000-00009. [DOI] [PubMed] [Google Scholar]
- Urmey W. F., McDonald M. Hemidiaphragmatic paresis during interscalene brachial plexus block: effects on pulmonary function and chest wall mechanics. Anesth Analg. 1992 Mar;74(3):352–357. doi: 10.1213/00000539-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Winnie A. P. An "immobile needle" for nerve blocks. Anesthesiology. 1969 Dec;31(6):577–578. doi: 10.1097/00000542-196912000-00013. [DOI] [PubMed] [Google Scholar]
- Winnie A. P. Interscalene brachial plexus block. Anesth Analg. 1970 May-Jun;49(3):455–466. [PubMed] [Google Scholar]