Abstract
Objectives
To examine reciprocal relations between body mass index (BMI), internalizing problems and externalizing problems from infancy through middle childhood with a focus on sex and history of overweight.
Study design
Data from 1254 children in the NICHD Study of Early Child Care and Youth Development were used to conduct longitudinal analyses of relations between BMI and scores on the Child Behavior Checklist from age two through 6th grade.
Results
BMI and behavior problems showed stability across the 7 measurement occasions. No consistent relation between BMI and behavior problems was evident prior to school entry; but being heavier was associated with later internalizing problems beginning in 1st grade for boys and girls. Higher BMI was not associated with increased conduct problems.
Conclusions
As children move into middle childhood, higher BMI is associated with increased likelihood of developing internalizing problems. Health care providers should monitor BMI as children enter school and to provide guidance to parents regarding emerging symptoms of anxiety and depression.
Keywords: Obesity, Internalizing Problems, Externalizing Problems, Mental Health
Despite the rapidly increasing prevalence of childhood obesity, the social stigma attached to being overweight has not diminished1–3. Although obesity can lead to low self-esteem and depression4–8 , most overweight children do not manifest serious depression or mood disorders9–13. Arguments have also been made that the psychological strain accompanying overweight can also lead to irritability and aggressive behavior, but the number of studies of conduct problems is quite small11,14–19. Overall, research on obesity and mental health (especially conduct problems) has been inconsistent, with variations noted by sex, age, family context, and duration and type of obesity 5,10,11,13,20,21. Direction of causality remains unresolved.
The purpose of this study was to further delineate the interplay of adiposity and maladaptive behavior in children followed prospectively from birth to determine (a) at what age relations with internalizing (depression and anxiety, withdrawal, somatic complaints) and externalizing (aggression, conduct problems, delinquency) behavior problems might emerge, and (b) the primary direction of influence. Data from the NICHD Study of Early Child Care and Youth Development 33–35 were used to determine whether lagged relations exist between BMI and behavior problems, either in the form of earlier BMI predicting to later maladaptive behavior or in the form of earlier behavior problems predicting to later BMI, after taking into consideration the stability in both BMI and behavior problems. A secondary purpose of the study is to determine whether the pattern of relations observed are different for children (a) with a history of being overweight, and (b) for boys versus girls.
Methods
The data analyzed in this study were taken from participants in the NICHD Study of Early Child Care and Youth Development (http://secc.rti.org). Families were recruited during the first 11 months of 1991 from 24 hospitals in the vicinity of 10 data collection sites (Charlottesville, Virginia; Irvine, California; Lawrence, Kansas; Little Rock, Arkansas; Madison, Wisconsin; Morganton, North Carolina; Philadelphia, Pennsylvania; Pittsburgh, Pennsylvania; Seattle, Washington; and Wellesley, Massachusetts). Using a random sampling procedure designed to assure representative coverage of days of the week at participating hospitals, a total of 8986 women who gave birth during the selected 24-hour periods were contacted and given information about the study. We asked their permission to contact them one month later to describe the study in greater detail. The study was conducted under a cooperative agreement with the National Institute of Child Health and Human Development. All procedures were reviewed annually by the institutional review boards of the 10 participating institutions.
Mother-newborn dyads were excluded if: the mother was under 18 years old, did not speak English, had a substance abuse problem, was too ill, was placing her infant for adoption, or refused to be interviewed; if the infant had serious medical complications or was a multiple birth; or if the family lived more than an hour’s drive from the lab site, or planned to move from the area. 5416 families met the eligibility criteria. Study participants were selected from eligible families based on conditionally random sampling to insure the sample would include at least 10% single-parent households, 10% mothers with less than a high school education, and 10% ethnic minorities. Recruitment and selection procedures are described in detail in previous publications34 (http://secc.rti.org). A total of 1364 families with healthy newborns were enrolled in the study.
Analysis sample
The analysis sample consisted of 1254 children (608 girls, 646 boys). Children were included if they participated in any of the repeated assessments of Body Mass Index (BMI) or Internalizing and Externalizing Problems. In the analysis sample, mothers had an average of 14.3 years of education and were living with a spouse or partner an average of 82.5% of measurement occasions from the time children were 6 months of age until 6th grade. Their average family income, assessed in terms of income-to-needs averaged from the period months to 6th grade, was higher than the U.S. government-determined poverty line by a factor of 3.91. Compared with the 110 children who were recruited at birth but not included in this analysis because of missing data, children in the analysis sample were more likely to be white (77.5% vs. 63.6%, p < 0.001) and lived in two-parent families a greater proportion of the time (M = 83.5% vs. 65.9%, p < 0.0001); had mothers with more years of education (M = 14.33 vs. 13.08, p < 0.0001), and families with higher income-to-needs ratios (M = 3.91 vs. 2.34, p < 0.0001).
Children were followed from birth through age 14. Each family was visited at home when the target child was 1, 6, 15, 24, 36, and 54 months of age, and when the child was in 1st, 3rd, 5th and 6th grades. At each home visit, mothers responded to a demographic interview and completed questionnaires about themselves, the child, and their family, and children were observed in interaction with one or both parents. Mothers and children from all families also came to university laboratories when they were 15, 24, 36, and 54 months old, and during 1st, 3rd, 4th, 5th and 6th grades. At these visits children completed standardized assessments and developmental tasks and were observed during play and interaction with their mothers. Beginning when they were 9½ years old, children received annual health and physical development assessments from a nurse practitioner or physician.
Standardized procedures were used to measure height and weight at 24, 36, and 54 months, and at 1st, 3rd, 5th, and 6th grades. Height was measured with children standing with shoes off, feet together, and their backs to a calibrated 7-foot measuring stick. Height was measured to the nearest 1/8 inch (0.32 cm) and recorded two times. If the first two measures differed by more than 1/4 inch (0.64 cm), two more measurements were taken. Weight was measured using a physician’s 2-beam scale. Scales were calibrated monthly using certified calibration weights. Weight was measured with children in minimal clothing (i.e., undergarments); it was measured twice, each time to the nearest ¼ pound (0.1 kg). If the two measurements differed by more than ¼ pound, two more measurements were taken. BMI was calculated by converting height to meters (m) and weight to kilograms (kg) then dividing weight (kg) by height (m) squared.
For each assessment of BMI, children were classified as “at risk for overweight” (BMI percentile ≥ 85%ile) or “normal weight” (BMI percentile < 85%ile). Based on their classifications from 24 months to 6th grade, children were grouped into “never overweight” or “overweight one or more times”.
Mothers completed the Child Behavior Checklist (CBCL) at 24, 36, and 54 months and at 1st, 3rd, 5th and 6th grades. The CBCL-2/333, used at 24 and 36 months, lists 99 problem behaviors which are rated as not true(0), somewhat true(1), or very true(2) of the child over the last 2 months. The CBCL-4/1834, completed by mothers at 54 months and 1st, 3rd, 5th and 6th grade, lists 113 problem behaviors rated on the same 3-point scale. There is substantial evidence for reliability and validity of these maternal reports36,37. Correlations across adjacent time points ranged from .54 to .73 for Internalizing Problems and .66 to .79 for Externalizing Problems.
The primary analysis model involved fitting a cross-lagged structural equation model tested using AMOS 4.0139. AMOS uses full information maximum likelihood estimation of missing data and utilizes the maximum sample size for each pathway to be estimated without deletion or imputation39. Overall model fit was assessed using the Root Mean Square Error of Approximation (RMSEA), as well as the Normed Fit Index (NFI) and the Tucker Lewis Index (TLI).
The original or baseline model included stability coefficients between the measures of BMI, Internalizing Problems and Externalizing Problems. Cross-lagged paths were included from one measurement of BMI to the next measurement of Internalizing and vice versa; and from one measurement of BMI to the next measurement of Externalizing Problems and vice versa ( Figure 1; available at www.jpeds.com). In addition, correlations between residuals for Internalizing Problems and Externalizing Problems at each assessment period were calculated to account for common-rater variance.
Figure 1.
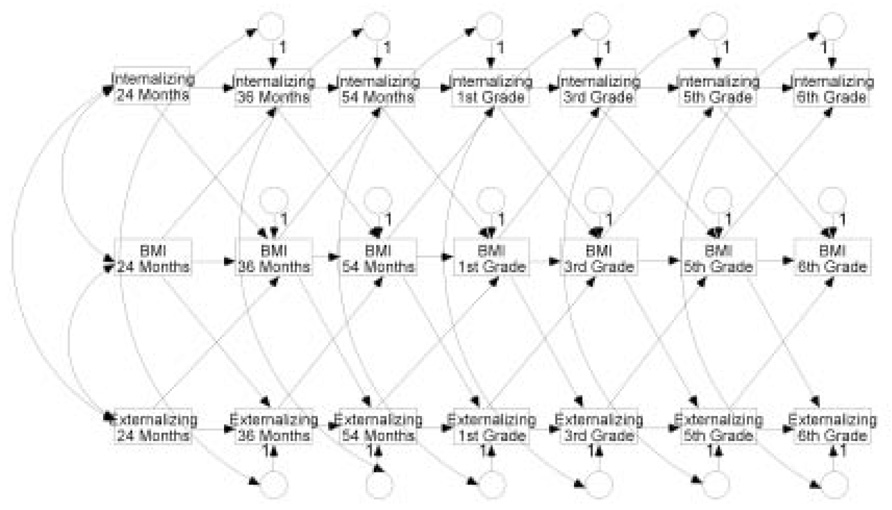
Baseline Model Showing Stability Paths and All Cross-Lagged Paths Between BMI. Internalizing Behavior and Externalizing Behavior.
We tested a series of nested models in an attempt to discern the most parsimonious model that adequately fit the data. We began with a model that included every possible pathway between adjacent measures (i.e., the model depicted in Figure 1). We then ran a series of analyses designed to determine whether certain paths might be eliminated without reducing overall model fit. In each case, chi-square difference tests were conducted to determine whether the imposed model constraints significantly influenced model fit.
Once the most parsimonious model was finalized, we tested potential moderators (sex and history of overweight) one at a time via two multi-group models. Chi-square difference tests were completed to determine how close the models for the two groups (i.e., boys vs. girls and overweight vs. not overweight) could be made without incurring a significant detriment to model fit.
Results
Descriptive statistics for study variables are presented in Table I (available at www.jpeds.com). The stability of BMI, internalizing problems, and externalizing problems are presented in Table II. Children’s average BMI declined between 24 and 54 months (24 mo: M = 16.77, sd = 1.37; 36 mo: M = 16.16, sd = 1.31; 54 mo: M = 16.05, sd = 1.56), then rose steadily through 6th grade (1st grade: M = 16.82, sd = 2.55; 3rd grade: M = 18.39, sd = 3.70; 5th grade: M = 20.00, sd = 4.64; 6th grade: M = 20.80, sd = 4.86). Average internalizing scores reached a high of 51.21 (sd = 9.50) when children were 36 months old and a low of 47.29 (sd = 8.88) when children were 54 months old. Average externalizing scores were highest at 24 months (M = 52.32, sd = 8.48) and lowest at 5th grade (M = 45.80, sd = 10.09).
BMI was highly stable beginning at age two (Table II). Correlations between adjacent assessments ranged between .79 and .97. Internalizing and externalizing behavior was relatively stable as well. Correlations between scores at adjacent time periods ranged from .54 to .79.
Correlations between BMI and internalizing were non-significant from age 24 months through first grade. Correlations between BMI and internalizing behavior during middle childhood (grades 3 to 6) were positive but low (never higher than r = .14). Correlations between BMI and externalizing behavior were sporadically significant but never higher than r = .12.
The baseline model fit the data well, p = 0.000, RMSEA = 0.06, NFI = 0.99, TLI = 0.99. We then conducted two analyses to determine whether the cross-paths between BMI and externalizing could be eliminated without reducing overall model fit. When constraining the cross-paths from externalizing to BMI to be zero, no detriment to model fit was noted, p = 0.39. The second analysis was aimed at determining whether the paths from BMI to externalizing could be eliminated. Similarly, constraining the cross-paths from BMI to externalizing to be zero did not hinder model fit, p = 0.39. This series of tests indicates that after controlling for stability, BMI does not relate to subsequent externalizing, and externalizing does not relate to subsequent BMI.
When constraining the cross-paths from internalizing to BMI to be zero, no detriment to model fit was noted, p = .0.64. However, when constraining the cross-paths from BMI to internalizing to be zero, model fit declined significantly, p < 0.01. Thus, after controlling for stability, internalizing is not related to subsequent BMI, but BMI is related to subsequent internalizing. Constraining the BMI to internalizing cross-paths to just the preschool period led to a significant decline in model fit, p = 0.03, but constraining the cross-paths to just the elementary period did not lead to a decline in model fit, p = 0.48. Thus, after controlling for stability, BMI and subsequent internalizing were unrelated in the preschool period (24, 36, and 54 months), but BMI was associated with subsequent internalizing during the elementary period (3rd, 5th, and 6th grade).
In this final (most parsimonious) model, standardized stability coefficients for BMI ranged from 0.81 to 0.97 (p < 0.001), standardized stability coefficients for externalizing ranged from 0.63 to 0.77 (p < .001), standardized stability coefficients for internalizing ranged from 0.52 to 0.71 (p < 0.001), paths from BMI to internalizing were significant between 3rd and 5th grade (0.04, p < 0.05) and between 5th and 6th grade (0.06, p < 0.01), but not between 1st and 3rd grade (0.02, p = 0.36).
We tested whether our two moderators (sex and history of overweight) influenced the remaining cross-paths of the model. In all cases, adding constraints requiring the cross paths to be equal for contrasted groups did not significantly affect model fit [Sex: Δ chi-square (3, n = 1254) = 1.45, p = 0.70); history of overweight: Δ chi-square (3, n = 816) = 7.79, p = 0.51)]. When additional constraints for various portions of the model were added (e.g., constraining means to be the same in the two groups), results regarding the cross-paths did not change.
Discussion
Although the association between BMI and internalizing appears relatively weak in middle childhood, findings from this study are consistent with research suggesting that being overweight can lead to internalizing behavior such as withdrawal, anxiety, and somatic complaints2,4,7,9,11,13,15. This finding, showing that overweight leads to internalizing symptoms but only beginning in middle childhood, is not surprising in that the social-cognitive processes that are presumed to forge the connection (feelings of stigmatization, dissatisfaction with body image, and beliefs that weight is under one’s personal control) are not well developed in most children prior to school entry28–30. It is not that preschool children are unable to perceive differences in body size or that they have not begun forming general negative attributions regarding people who are overweight; but rather that preschoolers have not begun internalizing feelings of being personally stigmatized and what that represents regarding their own behavior and life prospects1,40. A cross-sectional study of Australian children showed no relation between BMI and behavior problems for children age 5 but a significant relation at age 1418. Although we found no sex differences in patterns of relations for BMI and internalizing problems, a small number of prior studies suggest the possibility that the pattern may emerge slightly earlier in girls15,21. In neither study, however, was the measure of internalizing problems as complete as for our study.
Consistent with prior studies, our findings do not indicate a strong connection between BMI and serious internalizing problems8,10–12,19. In one study of 6 to 13 year old children, even though being overweight was related to mother- and teacher-reported internalizing problems, it was not related to child-reported depression41. However, studies done with clinical populations suggest that for some obese children the relation may be stronger10,13,17,22,42. However, as Puhl and Latner1 have argued, the relation is by no means inevitable. It may well be that some obese children are more vulnerable to the processes that give rise to depressive symptoms than others; thus there would be value in identifying potential protective factors.
Consistent with our hypothesis, we found no consistent relation between BMI and externalizing problems. In the few studies where a relation was observed, the study either involved clinical samples17,23 or produced findings that held for only one sex or at one age15. Moreover, in the one study that showed behavior problems predicting weight gain, the researchers used a measure of behavior problems that included both internalizing and externalizing behaviors31; and a second study involved older children who reported their own heights and weights41. The fact that ours is the only study to control for reporter bias suggests that there is limited likelihood that being overweight contributes to serious externalizing problems.
Findings from this study offered no support for the hypothesis that either internalizing behavior or externalizing behavior in non-clinical populations contributes to being overweight, a finding that comports with the conclusion offered by Zemetkin et al13. To date, there is no convincing support that being somewhat depressed increases the likelihood of becoming overweight prior to adolescence. There is a small amount of evidence suggesting that serious depression might increase such a tendency, but no general population studies have provided convincing evidence for such an effect. The only study with adequate controls that showed a link between earlier depression and later obesity in children involved children in grades 7 through 12 and used self-reported height and weight5. Thus, it will be useful to follow the current cohort of children to determine whether there is some shift in the pattern of relations beginning in adolescence.
A limitation of the present study is that there were too few children from most socio-cultural groups to conduct subgroup analyses. A second limitation is that mothers were the only reporters for children’s behavior problems. It would be worthwhile to perform analyses similar to those done in this study on minority populations within the United States as well as samples drawn from other countries.
Findings from this study offer further evidence that becoming overweight can carry a diverse array of negative consequences for well-being in children. As children move into middle childhood, being overweight is associated with increased likelihood of developing internalizing problems. The American Academy of Pediatrics Committee on Obesity Prevention recommends that physicians routinely monitor children’s BMI and provide guidance to parents regarding healthy eating habits, physical activity, and emerging symptoms of anxiety and depression44. Few pediatricians consistently check for signs of anxiety, depression or related signs of distress, but there are simple screening tools that can be used with parents when children are identified as overweight45. Although scores on such instruments do not provide definitive diagnoses, they can be used as a basis for making appropriate referrals for further assessment and possible intervention.
Acknowledgments available at www.jpeds.com.
Figure 2.
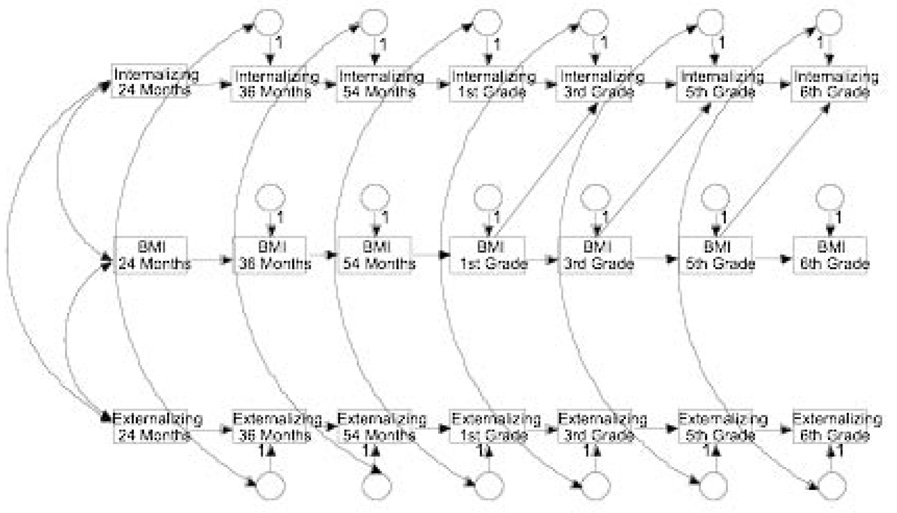
Final Model Showing Stability Paths and Significant Cross-Lagged Paths Between BMI. Internalizing Behavior and Externalizing Behavior.
Acknowledgments
This study is directed by a Steering Committee. Participating investigators for the NICHD Early Child Care Research Network are (listed in alphabetical order): Jay Belsky (Birbeck College, University of London), Cathryn Booth-LaForce (University of Washington), Robert H. Bradley (University of Arkansas at Little Rock), Celia A. Brownell (University of Pittsburgh), Susan B. Campbell (University of Pittsburgh), Elizabeth Cauffman (University of California, Irvine), Robert Crosnoe (University of Texas at Austin), James A. Griffin (NICHD Project Scientist and Scientific Coordinator), Bonnie Halpern-Fisher (University of California, San Francisco), Willard Hartup (University of Minnesota), Bonnie Knoke (RTI International), Kathleen McCartney (Harvard University), Philip Nader (University of California, San Diego), Marion O’Brien (University of North Carolina, Greensboro), Margaret Tresh Owen (University of Texas, Dallas), Ross Parke (University of California, Riverside), Robert Pianta (University of Virginia), Kim M. Pierce (University of Wisconsin), Glenn I. Roisman (University of Illinois at Champaign-Urbana), Susan Spieker (University of Washington), Elizabeth Susman (Pennsylvania State University), Deborah Lowe Vandell (University of California, Irvine), and Marsha Weinraub (Temple University).
This study is supported by NICHD through a cooperative agreement (U10) which calls for scientific collaboration between grantees and the NICHD staff. The authors declare no potential conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychol Bull. 2007;133:557–580. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- 2.Friedman MA, Brownell KD. Psychological correlates of obesity: Moving to the next research generation. Psychol Bull. 1995;117:3–20. doi: 10.1037/0033-2909.117.1.3. [DOI] [PubMed] [Google Scholar]
- 3.Latner JD, Stunkard AJ. Getting worse: the stigmatization of obese children. Obesity Res. 2003;11:452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- 4.French SA, Story M, Perry CL. Self-esteem in children and adolescents: a literature review. Obesity Res. 1995;3:479–490. doi: 10.1002/j.1550-8528.1995.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 5.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;109:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 6.Hesketh K, Wake M, Waters E. Body mass index and parent-reported self-esteem in elementary school children: evidence for a causal relationship. Int J Obesity. 2004;28:1233–1237. doi: 10.1038/sj.ijo.0802624. [DOI] [PubMed] [Google Scholar]
- 7.Strauss R. Childhood obesity and self-esteem. Pediatr. 2000;105(e15) doi: 10.1542/peds.105.1.e15. [DOI] [PubMed] [Google Scholar]
- 8.Young-Hyman D, Schlundt D, Herman-Wenderoth L, Bozylinski K. Obesity, appearance, and psychosocial adaptation in young African American children. J Pediatr Psych. 2003;28:463–472. doi: 10.1093/jpepsy/jsg037. [DOI] [PubMed] [Google Scholar]
- 9.Braet C, Mervielde I, Vandereycken W. Psychological aspects of childhood obesity: a controlled study in a clinical and nonclinical sample. J Pediatr Psych. 1997;22:59–71. doi: 10.1093/jpepsy/22.1.59. [DOI] [PubMed] [Google Scholar]
- 10.McElroy SL, Kotwal R, Malhotra S, Nelson EB, Keck PE, Nermeroff CB. Are mood disorders and obesity related? A review for the mental health professional. J Clin Psychiatry. 2004;65:634–651. doi: 10.4088/jcp.v65n0507. [DOI] [PubMed] [Google Scholar]
- 11.Mustillo S, Wortham C, Erkanli A, Keeler G, Angoold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111:851–859. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- 12.Sheslow D, Wallace W, DeLancey E. The relationship between self-esteem and depression in obese children. Annals NY Acad Sciences. 1993;699:289–291. doi: 10.1111/j.1749-6632.1993.tb18869.x. [DOI] [PubMed] [Google Scholar]
- 13.Zametkin AJ, Zoon C, Klein H, Munson S. Psychiatric aspects of child and adolescent obesity: a review of the past 10 years. J Amer Acad Child & Adoles Psychiatry. 2004;43:134–150. doi: 10.1097/00004583-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Bin W, Hong-Bo Z, Gang X. Survey on the behavioral problems in children with obesity from 6 to 11 years old. Chinese Mental Health J. 2005;19:679–681. [Google Scholar]
- 15.Datar A, Sturm R. Childhood overweight and parent- and teacher-reported behavior problems: Evidence from a prospective study of kindergartners. Arch Pediatrics & Adol Med. 2004;158:804–810. doi: 10.1001/archpedi.158.8.804. [DOI] [PubMed] [Google Scholar]
- 16.Datar A, Sturm R. Childhood overweight and elementary school outcomes. Int J Obesity. 2005;30:1149–1460. doi: 10.1038/sj.ijo.0803311. [DOI] [PubMed] [Google Scholar]
- 17.Israel AC, Shapiro LS. Behavior problems of obese children enrolling in a weight reduction program. J Pediatric Psych. 1985;10:449–460. doi: 10.1093/jpepsy/10.4.449. [DOI] [PubMed] [Google Scholar]
- 18.Lawlor DA, Mamun AA, O’Callaghan MJ, Bar W, Williams GM, Najman JM. Is being overweight associated with behavioural problems in childhood and adolescence? Findings from the Mater-University study of pregnancy and its outcomes. Arch Dis Childhood. 2005;90:692–697. doi: 10.1136/adc.2004.062919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stradmeijer M, Bosch J, Koops W, Seidell J. Family functioning and psychosocial adjustment in overweight youngsters. Int J Eating Disorders. 2000;27:110–114. doi: 10.1002/(sici)1098-108x(200001)27:1<110::aid-eat14>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 20.Herva A, Laiitinen J, Miettunen J, Veijola J, Karvonen JT, Joukamaa M. Obesity and depression: Results from the longitudinal Northern Finland 1966 birth cohort study. Int J Obesity. 2006;30:520–527. doi: 10.1038/sj.ijo.0803174. [DOI] [PubMed] [Google Scholar]
- 21.Krahnstoever–Davison K, Lipps-Birch L. Processes linking weight status and self-concept among girls from age 5 to 7 years. Dev Psychol. 2002;38:735–748. doi: 10.1037//0012-1649.38.5.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Erermis S, Cetin N, Tamar M, Bukusolglu N, Akdeniz F, Goksen D. Is obesity a risk factor for psychopathology among adolescents? Pediatrics Int. 2004;46:296–301. doi: 10.1111/j.1442-200x.2004.01882.x. [DOI] [PubMed] [Google Scholar]
- 23.Flodmark C-E. The happy obese child. Int J Obesity. 2005;29:531–533. doi: 10.1038/sj.ijo.0803060. [DOI] [PubMed] [Google Scholar]
- 24.Pine DS, Goldstein RB, Wolk S, Weissman MM. The association between childhood depression and adult body mass index. Pediatrics. 2001;107:1049–1056. doi: 10.1542/peds.107.5.1049. [DOI] [PubMed] [Google Scholar]
- 25.Tanofsky-Kraff M, Cohen ML, Yavonvski SZ, Cox C, Theim KR, Keil M, Reynolds JC, Yavovski JA. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117:1203–1209. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Epstein LH, Klein KR, Wisniewski L. Child and parent factors that influence psychological problems in obese children. Int J Eating Disorders. 1994;15:151–158. doi: 10.1002/1098-108x(199403)15:2<151::aid-eat2260150206>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 27.Harter S. Developmental and individual difference perspectives on self-esteem. In: Mroczek DK, Little TD, editors. Handbook of personality development. Mahwah, NJ: Erlbaum; 2006. pp. 311–334. [Google Scholar]
- 28.Sawyer MG, Lewis LM, Guy S, Make M, Canterford L, Carlin JB. Is there a relationship between overweight and obesity and mental health problems in 4- to 5-year-old Australian children? Ambulatory Pediatrics. 2006;6:306–311. doi: 10.1016/j.ambp.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Wardle J, Volz C, Golding C. Social variation in attitudes to obesity in children. Int J Obesity. 1995;19:562–569. [PubMed] [Google Scholar]
- 30.Tiggemann M, Anesbury T. Negative stereotyping of obesity in children: the role of controllability beliefs. J Appl Soc Psychol. 2000;30:1977–1993. doi: 10.1093/her/15.2.145. [DOI] [PubMed] [Google Scholar]
- 31.Lumeng JC, Gannon K, Cabral HJ, Frank DA, Zuckerman B. Association between clinically meaningful behavior problems and overweight in children. Pediatrics. 2004;112:1138–1145. doi: 10.1542/peds.112.5.1138. [DOI] [PubMed] [Google Scholar]
- 32.Wardle J, Williamson S, Johnson F, Edwards C. Depression in adolescent obesity: cultural moderators of the association between obesity and depressive symptoms. Int J Obesity. 2006;30:634–643. doi: 10.1038/sj.ijo.0803142. [DOI] [PubMed] [Google Scholar]
- 33.Nader PR, O’Brien M, Houts R, Bradley R, Belsky J, Crosnoe R, Friedman S, Mei Z, Susman E. the NICHD Early Child Care Research Network Identifying risk for obesity in early childhood. Pediatrics. 2006;118:e1–e8. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- 34.NICHD Early Child Care Research Network. Nonmaternal care and family factors in early development: an overview of the NICHD study of early child care. Appl Dev Psychol. 2001;22:457–492. [Google Scholar]
- 35.NICHD Early Child Care Research Network. The effects of infant child care on infant-mother attachment security: results of the NICHD study of early child care. Child Develop. 1997;68:860–879. doi: 10.1111/j.1467-8624.1997.tb01967.x. [DOI] [PubMed] [Google Scholar]
- 36.Achenbach TM. Manual for the Child Behavior Checklist/ 2–3 and 1992 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1992. [Google Scholar]
- 37.Achenbach TM. Manual for the Child Behavior Checklist/ 4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 38.Ainsworth MD, Blehar M, Waters E, Wall S. Patterns of attachment: a psychological study of the strange situation. Hillsdale, N.J: Erlbaum; 1978. [Google Scholar]
- 39.Arbuckle JL, Wothke W. Amos 4.0 User’s Guide. Chicago: Small Waters Corporation; 1995–1999. [Google Scholar]
- 40.Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obesity Rev. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 41.Tanofshy-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. J Consulting & Clin Psychol. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Christoffel KK, Forsyth BW. Mirror image of environmental deprivation: severe childhood obesity of psychosocial origin. Child Abuse & Neglect. 1989;13:246–256. doi: 10.1016/0145-2134(89)90011-2. [DOI] [PubMed] [Google Scholar]
- 43.Anderson E, Cohen P, Naumova EN, Must A. Relationship of childhood behavior disorders to weight gain from childhood to adulthood. Ambulatory Pediatrics. 2006;6:297–301. doi: 10.1016/j.ambp.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 44.American Academy of Pediatrics Committee on Prevention? Policy statement: prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 45.Gardner G, Murphy M, Child G, Kelleher K, Pagano M, Jellinek M, McInerny TK, Wasserman RC, Nutting P, Chiappetta L. The PSC-17: a brief pediatric symptom checklist with psychosocial problems subscales. A report form PROS and ASPN. Amb Child Health. 1999;5:225–236. [Google Scholar]


