Abstract
Background
This study aimed to examine kidney transplant recipients’ ability to afford transplant-related out-of-pocket expenses and the financial impact of these expenses on their lives.
Participants and methods
This cross-sectional study involved 77 kidney recipients. Variables analyzed were: ability to afford daily necessities; impact of immunosuppressant expenses on patients’ lives; awareness of Medicare support terminating 3 years post-transplant; and strategies used to pay for out-of-pocket transplant expenses. The Economic Strain Scale measured financial strain.
Results
Twenty-nine percent of kidney recipients experienced financial strain. Poor, less educated, and younger patients were more likely to report financial strain. Out-of-pocket expenses relating to kidney transplantation adversely affected patients’ ability to afford leisure activities (35%), a house (27%), and a car (26%). Thirty-one percent reported that immunosuppressant expenses have had somewhat to great (adverse) impact on their lives. Of those on Medicare and not disabled (n=41), 51% were unaware Medicare coverage will terminate, and 71% did not know how long coverage lasts.
Conclusions
Financial strain presents a considerable risk to kidney recipients’ ability to purchase immunosuppression. Socioeconomic disparities in recipients’ financial strain may be a source of disparities in graft survival. Transplant professionals should better inform transplant candidates about financial consequences of transplantation.
Keywords: kidney transplantation, immunosuppressant, medication, disease expenses, finances, Medicare, health policy, socioeconomic disparities, coping, insurance
Background
Kidney graft loss in the first 10 years following transplantation is a significant problem compounded by socioeconomic and racial/ethnic disparities in graft survival rates (1). The level of insurance coverage has been identified as a major factor contributing to disparities in transplant survival in the United States (2,3). Sufficient coverage of anti-rejection medication is essential because kidney recipients must take immunosuppressants for the life of the functioning kidney graft. The average cost of immunosuppressants is between $10,000 to $14,000 per year (4). In the United States, because patients with end-stage renal disease (ESRD) are entitled to renal replacement therapy by Medicare, Medicare covers 80% of immunosuppressant costs for 3 years post-transplant, while patients and/or insurers cover the rest (5,6). After 3 years, patients receive no financial help from Medicare. Patients who are age 65 and older and/or disabled are legally exempt from these limitations in coverage. Additionally, approximately 12% of the ESRD population are ineligible for Medicare (7).
Kidney transplant advocacy groups have been lobbying Congress to extend Medicare’s entitlement for kidney transplant recipients beyond 3 years, for the life of the kidney (8). Section 113 of the Beneficiary Improvement and Protection Act of 2000 extended immunosuppressive coverage for the life of the kidney but only for patients who qualify for Medicare coverage because they are age 65 or over or disabled. Kidney recipients are no longer regarded as disabled because transplantation is considered rehabilitation, enabling patients to return to work. Most kidney recipients do not have legally defined disabilities, although reports document that 42.5% (of n=226) experience symptoms restricting their work capabilities (9), and therefore income.
The risk of graft rejection from being unable to purchase and take immunosuppressants is a pressing public health problem because transplantation is the treatment of choice for most patients with ESRD (10). Transplantation provides a longer length of life and better quality of life than dialysis (11,12), and is more cost-effective than dialysis (4,13). When kidney grafts fail, patients return to dialysis, creating a greater demand for scarce (re-)transplants, further burdening society with greater costs and increasing ESRD patient mortality rates (14–18). These concerns, compounded by the organ shortage, underscore the need to maximize long-term graft survival (19,20). Understanding factors contributing to long-term graft survival is critical to public health and its expectation that resources be utilized efficiently.
Little is known about whether patients with Medicare coverage experience financial strain in procuring the 20% of expenses in the initial three years post-transplant or thereafter. One telephone survey study of 318 kidney transplant recipients found that 38.4% reported financial strain due to health problems relating to transplantation (21). Yet even for patients with adequate health insurance, immunosuppressants are considered expensive (22). Most patients in one study perceived their health insurance to be inadequate since they were unable to afford the medications, the high copayment or deductible, and the cost of insurance (23). Further, it remains to be determined whether financial strain leads to difficulty obtaining medications thus jeopardizing kidney graft survival. Studies show that financial strain is adversely related to health outcomes (24–26), and contributes to socioeconomic inequality (27). Understanding the range and extent of strategies by which new kidney recipients manage the expenses of transplant medications can shed light on the social context and consequences of Medicare’s policy (28,29).
Previous research has focused on quantifying the impact of insurance coverage on graft outcomes at the population level. These studies document well that Medicaid patients have lower graft survival than patients with private insurance (30), and that Medicare’s duration of coverage affects graft survival differentially by income level (14,15). However, these studies do not examine how kidney recipients respond to the financial demands encountered by the transplant and how transplant-related expenses affect their lives. This paper examines new kidney recipients’ ability to afford these expenses, and the financial impact of immunosuppression on their lives. We provide insight into patients’ personal experiences in dealing with financial changes to their lives generated by transplantation. The financial impact of immunosuppression on new kidney recipients’ lives may serve as a source of socioeconomic disparities in transplant survival. We hypothesize that patients experiencing financial strain are more likely to be ethnic minorities and socioeconomically disenfranchised.
Study Data and Methods
All kidney transplant recipients were recruited in an incidence cohort from Loyola University Medical Center (LUMC) in Maywood, IL (July 2004 - May 2006) and Albany Medical Center (AMC) in Albany, NY (September 2006 - October 2007). Kidney recipients were eligible for participation if they: were 18 years and older, were currently taking immunosuppressants, spoke English, and received a transplant within the previous 6 months. New kidney recipients were recruited in order to capture patients’ financial experiences at the initial stages post-transplant while Medicare coverage was at its greatest, since changes in Medicare and other insurance coverage will affect their finances differently over time.
We used a combination of quantitative and qualitative methods to compare findings across participants and clarify why patterns emerged. We conducted semi-structured interviews with kidney recipients on average within 2 months post-transplant. The interview was part of a larger, longitudinal study on self-care management. Topics covered in the interview, as they pertain to this paper, included: patients’ financial status, how the transplant affects their finances, how the financial aspects of transplant affect patients’ lives, how patients make ends meet, knowledge of current and future insurance coverage, experience interacting with insurance companies or public aid, and demographics. Interviews were conducted in-person or over the phone over one or more sessions according to participant preferences. Interviews were approximately 2 hours, were tape recorded, and transcribed verbatim. Respondents were compensated $20 as an incentive to participate. Institutional Review Board approval was obtained from Loyola University Medical Center and Albany Medical Center. Study participants provided written informed consent.
Financial Strain
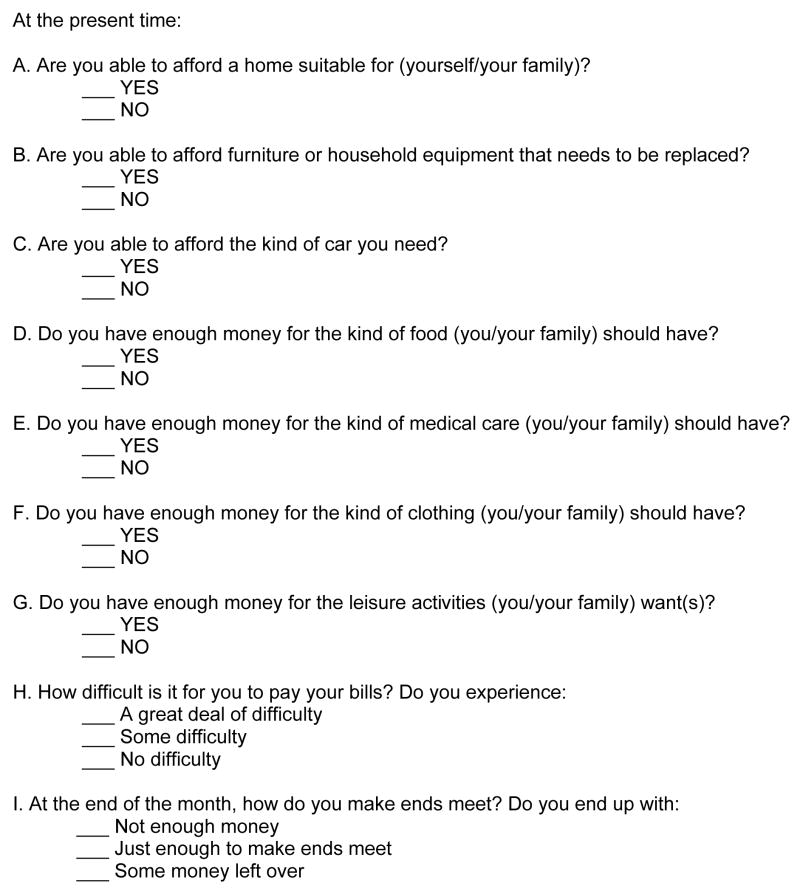
Our primary outcome measure, financial strain, was based on the Economic Strain Scale (ESS) (31,32). The ESS is a 9-item measure, assessing whether an individual has enough money to afford food, medical care, clothing, and leisure activities, and how the patient’s finances figure at month end (see Figure 1). Response anchors range from “some money left over” to “not enough money to make ends meet.” Cronbach’s alpha is 0.86, as reported elsewhere (24); and test-retest reliability correlation is 0.59 (32). The total possible score is between 0 – 11, with a lower score reflecting greater strain. For analysis purposes, we used a cut-off of 7 to indicate financial strain.
Figure 1.
Economic Strain Model Questionnaire (Pearlin et al. 1981)
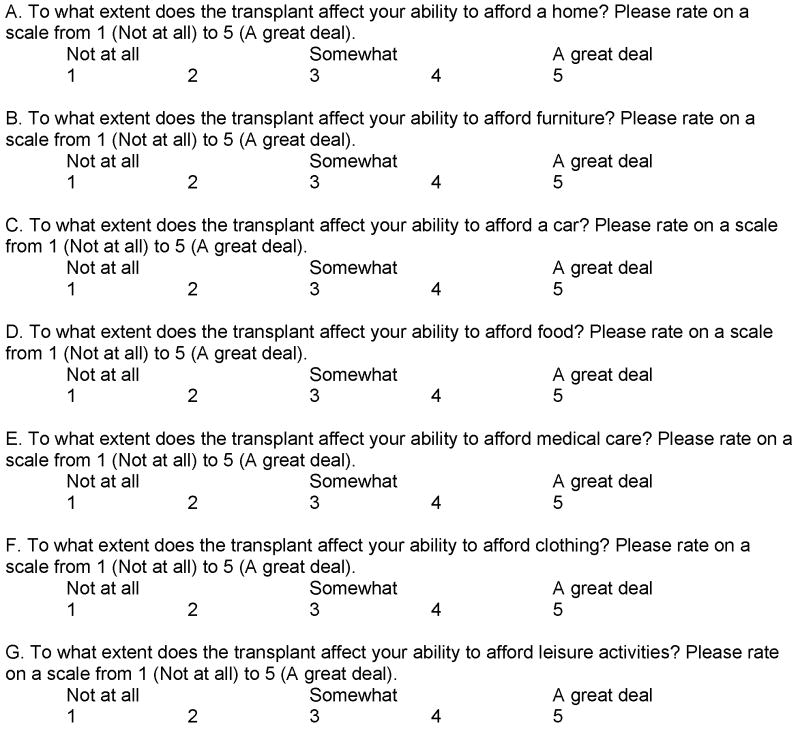
We constructed a secondary parallel measure of financial strain specific to kidney transplantation based on the ESS. This measure included Likert-scaled items assessing the impact of the transplant on patients’ ability to afford living expenses (e.g., home, furniture, car, food, medical care, clothing, and leisure) (see Figure 2). We also constructed measures that included Likert-scaled items assessing the impact of medication expenses on patients’ lives currently and six months from the present time. For the purpose of analysis, we grouped together patients who reported ‘some’ to ‘a great deal’ of financial difficulty (3–5) and compared them to patients who reported ‘none’ or ‘a little’ difficulty (1–2) on all Likert scales.
Figure 2.
Daily Necessities
Descriptive and inferential statistics were used to analyze the data. T-tests and One-way ANOVA were used to compare categorical respondent characteristics by financial strain. Spearman’s rho was used to run correlations between financial strain measures and continuous variables. A multivariate linear regression model was used to examine the relationship between financial strain and patient characteristics. Covariates included demographic (age, gender, race, marital status), socioeconomic (income, education, ability to afford daily necessities), and clinical characteristics (cause of ESRD). Race was based on self-identification, and dichotomized (white versus non-white) due to limited variation in the sample. Dependent variables included financial strain and ability to afford daily necessities. All tests were two-tailed and p < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 15.0 (SPSS, Inc., Chicago, IL). Respondents who did not answer a specific question or part of a multidimensional question were excluded from the analyses of that data element. Kidney recipients’ open-ended responses were analyzed by content analysis, which entails the systematic search for themes and repetitions emergent from the data (33,34). Inter-rater reliability was established as 90% using established methods (35).
Study Results
Of 139 eligible patients, 77 participated in an interview, for a 55% response rate. Twenty-four percent refused to participate due to slow recovery from the operation or time commitments, and 20% gave oral consent but have not yet provided written consent or were unable to be reached for an interview. The sample was predominantly male (57%); married and/or with a partner (78%), and had a high school diploma (93%). The majority of patients were European American (66%; 20% African American, 8% Hispanic, and 6% other). Ages ranged from 21 to 74, with a mean of 48 years. The religious breakdown was predominantly Protestant (43%) or Catholic (38%), or other/none (19%). The demographics of participants generally reflect the age and gender profile of ESRD and kidney transplant recipients nationally (36).
Financial Strain
Two-thirds of patients reported having no financial strain, and attributed their financial stability to having sufficient insurance coverage. For many of these patients, Medicare and/or Medicaid covered most or the entire co-payment for transplant medications. However, almost a third (29%) of kidney recipients experienced financial strain [range: 0–11, SD: 2.950] (Table 1). Patients who were more likely to report greater financial strain: had lower income (r=0.61, p<0.0001, n=71); had Medicare as the primary insurance (t=2.069, p<0.043, n=73); had less education (r=0.31; p<0.007, n=76); were not married (t=2.097, p<0.039); and were younger (r=0.29, p<0.01). There was a trend approaching significance for such patients to be non-white (t=1.842, p<0.074). Thirty-one percent reported that the immunosuppressant expenses have had somewhat to great (adverse) impact on their lives. Seven percent experienced difficulty paying for anti-rejection medications.
Table 1.
Demographic Breakdown of Mean Financial Distress*
| Demographic | N (%) | Financial Distress Mean (SD) | p-value |
|---|---|---|---|
| Total | 77 | 8.5 (3.0) | |
| Income Levels† | 0.0001 | ||
| < $29,999 | 20 (26.0) | 6.0 (3.0) | |
| $30,000 – $74,999 | 32 (41.6) | 9.3 (2.2) | |
| $75,000 + | 19 (24.7) | 10.3 (1.2) | |
| Education Levels | 0.007 | ||
| < High School | 5 (7.0) | 8.0 (3.3) | |
| High School | 22 (28.6) | 7.7 (3.2) | |
| Some – all College | 37 (48.1) | 8.8 (2.7) | |
| Graduate School | 12 (15.6) | 9.7 (3.1) | |
| Age Categories | 0.01 | ||
| 21– 48 years | 41 (53.2) | 7.9 (3.2) | |
| 49 + years | 36 (46.8) | 9.2 (2.6) | |
| Marital Status | 0.04 | ||
| Not married | 28 (36.4) | 7.6 (3.2) | |
| Married | 49 (63.6) | 9.0 (2.7) | |
| Primary Insurer | 0.05 | ||
| Medicare | 34 (44.2) | 7.8 (3.5) | |
| Private | 39 (50.6) | 9.2 (2.3) | |
| Race | 0.08 | ||
| Non-White | 25 (32.5) | 7.5 (3.6) | |
| White | 52 (67.5) | 9.0 (2.4) | |
| Gender | |||
| Male | 44 (57.1) | 8.7 (3.1) | 0.58 |
| Female | 33 (42.9) | 8.3 (2.7) |
Totals do not add up to 77 because participant(s) did not disclose information.
Significant differences were found between income categories <$29,999 and $30,000–$74,999; and between $29,999 and $75,000+.
A multivariate analysis of the impact of sociodemographics and the ability to afford daily necessities (see below) on financial strain was conducted. Findings revealed that financial strain associated with medication expenses was significantly negatively related to the ability to afford a home (p=0.005) and clothing (p=0.002), and positively related to total gross income (p=0.0001). The model captured 59.9% of the explainable variance (F<0.0005).
Affording Daily Necessities Related to Transplantation
When comparing specific domains of daily necessities, patients reported the extent of difficulty in their ability to afford daily necessities due to transplant-related expenses (Table 2). Patients reported facing the greatest difficulty affording leisure activities, their house, and a car, as shown by the higher percentages of respondents reporting strain in these domains. Patients experiencing difficulty affording any one daily necessity were significantly likely to encounter difficulty affording all other daily necessities (p<0.0001) (except the relationship between affording a home and food was p<0.001), and to experience greater financial strain (p<0.0001). Demographic correlates of difficulty affording daily necessities because of the transplant are presented in Table 2. Patients with lower incomes were more likely to experience difficulty affording a car, medical care, a home, furniture, clothing, and leisure. Patients who were younger were more likely to experience difficulty affording a car, clothing, furniture, and leisure. All patients stated that they have prioritized and/or would prioritize the purchase of immunosuppression and other transplant medications over daily necessities when or if they had to make a choice about what to buy.
Table 2.
Patient Characteristics Associated with Difficulty Affording Necessities Due to the Transplant
| Daily Necessity | Percent Reporting Difficulty† | Patient Characteristics | |||
|---|---|---|---|---|---|
| Income | Age | Non-Married | Financial Strain | ||
| Leisure Activities | 35% | r = − 0.33** | r = − 0.33** | t = − 1.901 | r = − 0.56*** |
| Home‡ | 27% | r = − 0.32** | r = − 0.20 | t = − 0.153 | r = − 0.47*** |
| Car‡ | 26% | r = − 0.37** | r = − 0.45* | t = − 0.896 | r = − 0.56*** |
| Medical Care‡ | 25% | r = − 0.34** | r = − 0.15 | t = − 0.791 | r = − 0.40*** |
| Clothing | 21% | r = − 0.33** | r = − 0.30** | t = − 1.192 | r = − 0.60*** |
| Furniture‡§ | 21% | r = − 0.26* | r = − 0.25* | t = − 0.483 | r = − 0.47*** |
| Food§ | 16% | r = − 0.16 | r = − 0.20 | t = 0.271 | r = − 0.50*** |
p < 0.05;
p < 0.01;
p < 0.0001
Percentages based on ‘some’ to ‘a great deal’ of difficulty.
1 patient reported ‘don’t know’. The percentage is calculated on full sample size (n=77), except in correlations.
1 patient was not asked this question. The percentage is calculated without this case in the denominator.
Strategies to pay for out-of-pocket medication expenses and make ends meet
Participants were asked open-ended questions about their specific strategies to pay for out-of-pocket expenses of medication and other transplant related expenses. Analysis of their open-ended responses reveals that patients used three major strategies to afford the out-of-pocket expenses of transplantation, including: 1) cutting down on expenses and closely monitoring day-to-day expenses; 2) borrowing money or resources from family or using credit; and 3) earning additional income.
1. Cost-cutting
With regard to the first strategy, patients reported cost savings approaches which ranged from minor to major lifestyle changes, including limiting spending in general, using coupons, food stamps, buying generic brands instead of name brands, and buying used cars instead of new cars (box 1). Participants reported cutting back on entertainment such as cable television, hobbies, and vacations, and changing their eating habits by avoiding restaurants, buying food in bulk, and cutting back on food. Daily necessities were also not purchased as often, including clothing, gasoline for cars, and laundry. These examples reflect the extent to which patients consider minor expenses in their efforts to manage finances. The following statements provide insight into how patients undertake these efforts and the effects on their lives.
Box 1. Cost-cutting efforts
“I always take care of all my medical problems which are considerable but by budgeting. I’m able to just scrape by every month. I cook all my own meals and stay home basically” (56 year old male with total family income less than $15,000; #10011)
“I just study the [supermarket] ads that come through, and I just arrange my meals around the [supermarket] ads. I just analyze and just look at everything as a whole picture and then just mark, you know, so much for this, so much for that, so I have everything broken down before my check even gets here. And then I go by that, to the best I can. (49 year old female, with total family income between $15,000–$30,000; #12297).
Another notable approach to budgeting is by living “paycheck by paycheck,” as the following quote demonstrates:
Box 2. Cost-cutting by living paycheck by paycheck
“Well, we pretty much live paycheck to paycheck. The checking account pretty much is in and out… For years, we paid [the Visa bill] off all the time, and now we can’t keep up with it. It’s awful, but it’s a couple thousand more than we can afford to pay off. So, we’re a little concerned about that” (57 year old female with total income over $105,000; #10043).
An extreme, albeit not uncommon, lifestyle change was to avoid marriage (box 3) or to remain married (albeit separated) to retain insurance coverage:
Box 3. Cost-cutting by avoiding marriage
“If I didn’t have a kidney transplant I would be able to get married and I can’t get married because then I wouldn’t have insurance. If I didn’t have the transplant I’d be able to work, therefore, I would be able to make more money. I should be able to support my kids and home better.” (41 year old female, with total family income under $15,000; #10039)
2. Borrowing money from family or by credit
The second set of strategies entails borrowing money or resources by credit or from family, including using credit cards, paying bills late, and paying less on bills (box 4). Participants reported relying on family for assistance, including borrowing money from family and moving into their parents’ home. Others reported depleting their saving accounts, which leaves no safety net for future transplant-related expenses. Such approaches enable patients to afford their immediate expenses, yet patients recognize that repaying their debts or getting ahead is unlikely.
Box 4. Borrowing money
“Yeah, like right now, for example, we didn’t pay insurance on time this month. So they just sent us a final [bill], like, you have to pay by the 30th or we’re gonna cut it off. So, now we know that we really have to pay it by the 30th, even though it was actually due on the 15th, like car insurance that’s it. [EG: So you wait until--] Yeah, we wait until the absolute last minute on pretty much everything.” (28 year old male, with total family income between $30,000–$45,000; #12315)
“My daughter pays for everything. I also took a loan. Initially, my daughter paid for my medication with her credit card. But because I did not want to rack up her debt, I took a loan out of about $6,000. I had to take a loan to pay my bills. It basically put me in debt. No other way.” (53 year old male, with total family income less than $15,000; #10027).
3. Earning additional income
The third set of strategies involves earning additional income either before or after the transplant. Participants reported preparing their finances prior to the transplant by paying off debts, receiving money raised from fundraising or paid vacation time donated by co-workers, and through prior investments. Participants stated that they are currently employed or plan to earn additional income by having themselves and/or their spouses, family members, or significant others return to work or work more hours. Alternatively, participants, particularly those unemployed, stated that they rely on insurance or retirement pension or disability for income. The following statements convey how patients had prepared for the expenses in advance of the transplant (box 5).
Box 5. Preparing for the expenses of transplantation
“We tried to prepare before we went in. You know, like, to have a mortgage payment paid, a car payment paid. We had enough for two months. Um, coupons, just watching the sales, you know, being cautious of money. Just, buy what we need. Little more tighter with the money” (47 year old female, with total family income between $45,000–$60,000; #12296)
“I was able to work overtime and kind of prepare financially to be out for a couple of months. [Interviewer: So, did you save?] Save, and work through an agency and it worked. It was difficult in my condition, considering the way I was, but I did it” (44 year old female, with total income between $60,000–$75,000; #10010)
Most patients stated that they or their spouse/partner will look for a job to earn enough money to pay for their medications and other transplant-related co-payments (box 6). As the following quotes illustrate, transplant-related health issues can present difficulties in finding employment, and do not affect just the recipient, but also other family members’ lives.
Box 6. Return to work
“Well, I don’t think it affected my finances because I was on disability. I was getting disability, you know, but they say in nine months, I’ve got to come off of it because of the kidney. That’s why I’m out looking for a job. But you can’t lift anything over 35 pounds. I mean, these factory jobs, you’re going to lift more than that. So, I don’t know what they expect me to do” (50 year old male, with total income between $15,000–$30,000; #10038)
“Well, [my spouse] had to go to work. I’ve had to stay home a lot. She has a part-time job. [Spouse: We use credit a lot.] We’ve had to use credit that we wouldn’t have to otherwise. And we have to be more conservative on what we spend it on” (49 year old male, with total family income between $60,000–$75,000; #10002)
Compounding difficulties in making ends meet is the fact that optimal self-care management for the transplant requires new additional expenses. New expenses patients identified include purchasing more prescriptions, fruits and vegetables, fluids besides water to keep kidneys well-hydrated, and new clothes to accommodate body shape changes due to the frontal placement of the graft and weight gain from immunosuppressants.
Kidney Recipients’ Understanding of Medicare Coverage Policy
Patients were asked to describe their understanding of Medicare’s coverage, in response to questions pertaining to the amount of their coverage over time. Of the 41 patients who have Medicare as either their primary or secondary insurer, and were neither on disability nor age 63 or older (who would continue to receive Medicare after 3 years post-transplant upon reaching the age of retirement), 51% were unaware that Medicare coverage will terminate, and 71% did not know or had an inaccurate estimate of how long coverage lasts. Patients who had an inaccurate estimate of Medicare duration of coverage were more likely to be non-white (X2=9.279; p=0.001). Despite an accurate awareness of Medicare coverage ending, one patient’s response captures well a present-time orientation toward their finances commonly expressed by many kidney recipients (box 7).
Box 7. Present-time orientation toward finances
“I don’t mind paying for some of my meds, but if I can’t afford them, I don’t know. Of course, now I want to try to get a full-time job, so I can maybe get insurance or have more money coming in. There’s no reason why I can’t work full-time now. But I’m not gonna worry about it. I’ve been so lucky and blessed and I feel good. I’ll handle it when it comes. We’ll figure it out, we’ll do whatever we have to do. I’m not gonna worry about three years from now. One day at a time.” (47 year old female, with total family income between $45,000–$60,000; #12296)
Another sentiment patients expressed was the disbelief that Medicare coverage will end given large societal and financial investments in transplantation (box 8).
Box 8. Disbelief that Medicare coverage will end
“I’ve never heard that they would only pay for medications for two years after you spend thousands and thousands of dollars to do a transplant, you know, and knowing if you don’t have the medication, you’re going to lose the kidney, be right [back] and then you’ll be paying for the dialysis anyway, so, you know to me that was just insane.” (36 year old female, with total family income below $15,000; #10028).
Patients were asked how they will afford medicines when Medicare ends. Most patients reported they will continue to work or be retired and expect no change in insurance coverage. Others plan to get a new job or get other insurance. However, patients feared that pre-existing health conditions would prevent them from obtaining insurance. Many patients reported not knowing what they would do to afford the medications when Medicare runs out because they have not planned that far ahead, or they recognize that insurance companies change policies frequently. As the following quotations show, a current of uncertainty yet hopefulness about insurance coverage in the future pervades patients’ comments (box 9).
Box 9. Uncertainty about future insurance coverage
“I’m on Medicaid. If they’re taking that away, it’s going to be Medicare and I’m going to have to pay something instead of not paying anything right now, you know what I mean. So, it’s going to get a little worse for me. I don’t know exactly how much because I haven’t looked into the forty different plans. I’m kind of scared of those. It’s like I don’t want to have to understand them because I’m not going to understand them. You know what I mean—there’s too many words there. Dumb it down for me <laughs>” (26 year old male, with total family income below $15,000; #10041).
“I’m planning on it. I’m trying not to think about that right now, but you know, I take one day at a time. I mean, if I’m on Social Security Disability, then I know I qualify for Medicare. I don’t know about Medicaid ‘cause all the changes that are going on I’ve heard – but I know I’ll have Medicare. And that’s my primary, so I’m not really worried about it right now” (49 year old female, with total family income between $15,000–$30,000; #12297)
Future Financial Strain
We asked kidney recipients to rate how much financial difficulty they anticipate having in six months. Almost one-third (29%) of kidney transplant recipients anticipated having future financial difficulties. Three reported they did not know. Patients who were more likely to predict greater financial difficulty in six months had less education (r= −0.30; p<0.009, n=73), had Medicare as their primary insurer (t= −2.16, p<0.035, n=70), earned less than $60,000 in total family income per year (t = −4.670; p<0.001, n=68), and were unemployed (t= −2.32, p<0.024, n=72). A trend approaching significance was found for non-white patients (t= −1.855, p<0.074).
Ten patients (13%) reported that the transplant has had or they expect it to have a positive effect on their finances. Most explained that the transplant has freed up time to return to work or work more hours, and thus earn more money. As one patient explained, since the outcome of the transplant has been positive, “I was able to return to work within weeks of the transplant. And therefore, I did not miss the paycheck.” (41-year old male, with total family income over $105,000; #12318).
Discussion
This is the first qualitative study we are aware of that examined the complications involved in the financial management of transplantation from the recipient’s point of view and our findings suggest serious concerns about the effects on patients’ financial well-being. We found that almost a third of kidney recipients at the early stages post-transplant experienced financial strain, and a further third anticipated strain in the near future. A substantial number of kidney recipients reported difficulty affording daily necessities because of the transplant-related expenses, which may adversely affect their health and compromise their ability to practice self-care management. Other research confirms our findings. Rodrigue and collegues (2007) similarly found that 38.4% (of 318) kidney recipients reported that health problems relating to transplantation caused financial problems for themselves or families (21). It remains to be determined what patients’ financial situation three years post-transplant will be like when Medicare entitlement terminates. However, Rodrigue and colleagues’ study suggests that financial strain increases as their study participants’ monthly expenses were significantly higher in years 4 and 5 than in year 3 (p<0.05) (21). This strain will likely jeopardize patients’ ability to purchase immunosuppression, which would lead to kidney rejection and return to dialysis.
The average level of financial strain using the Economic Strain Scale (ESS) of kidney recipients in our study was 8.5, which is lower than levels found in the general population (24). For example, Steptoe and colleagues (2005) found that the average ESS scores among 160 men and women who had an improvement in blood pressure at time 1 was 11.7, and 9.4 three years later; the average ESS scores among those who had worse blood pressure at time 1 was 8.8, and 9.6 three years later (24). It makes sense that kidney recipients, many of whom are unemployed and in worse health than the general population, have lower ESS scores (greater financial strain) than participants in Steptoe’s study.
Sociodemographic disparities emerged among kidney recipients experiencing financial stain. It remains to be determined whether such patients are more likely to experience long-term graft loss, which would explain, in part, a source of disparities in graft survival. Disparities can threaten public trust in transplantation, which has been shown to reduce the public’s willingness to donate organs. Fewer donated organs would further limit patients’ access to transplantation (37,38) and exacerbate disparities in transplant access and outcomes (17).
The strategies patients reported using to afford medications have strengths and weaknesses that can undermine their abilities to adequately afford medications. The first strategy, cutting costs, while easy and straightforward to engage in, has relatively little effect on patients’ ability to pay for co-payments and reduce financial strain. Specifically, cutting down on luxury items saves little in comparison to the greater expenses of the medications. The second strategy, borrowing money, is effective in sufficiently obtaining funds necessary to pay for out-of-pocket expenses. However, it is a highly risky approach that only postpones the consequences of financial distress to the future. The third strategy, earning additional income, while effective in procuring sufficient funds, is considerably difficult for patients to successfully achieve. Others have reported barriers kidney recipients face to finding jobs that provide insurance coverage for people with a pre-existing disease, and that are compatible with physical limitations imposed by their health condition and physician recommendation (9, 39). The study by Rodrigue and colleagues similarly found that the most common strategy patients used to offset out-of-pocket expenses incurred by transplantation was savings accounts and credit cards (21). When considering all these strategies together, it is apparent that kidney recipients have few effective options available to adequately afford these ongoing expenses and escape financial strain. Socioeconomically disenfranchised kidney recipients are most at risk of not affording medications or other daily necessities. However, patients who are well-to-do also face similar barriers to obtaining insurance coverage as less fortunate patients would, should they change jobs.
Limitations
The present study has several limitations. First, the research is limited by the small sample size. We were unable to undertake multivariate analyses to investigate deeper interactions between variables. Second, the recruitment attrition rate of 44% may have resulted in a biased sample. That the sample was relatively highly educated may be a vestige of characteristics of patients willing to participate in the study. Given the well-documented relationship between education and income, it is likely that comparable research on a more diverse sample would reveal even greater financial strain. Relatedly, patients early post-transplant may not have had enough time to ascertain the severity of the financial impact of transplantation on their lives, thus the reported levels of financial strain are likely conservative. Similarly, since the ESRD population is generally less educated than the national population (40), it is likely that future research with other samples of the ESRD population would reveal even less knowledge about Medicare coverage. Third, as a multi-site study conducted in the Midwest and Northeast, the findings may not be generalizable to other geographic areas in the US. Fourth, it is likely that transplant professionals did disclose financial information about the transplant to patients prior to and/or after receiving the transplant. That many patients reported no knowledge of limitations to Medicare coverage may be due to patients forgetting, not paying attention, or denial of financial adversity, and/or transplant professionals’ ineffective communication. The idea of denial is conveyed well in one kidney transplant recipient’s narrative account: “I didn’t think about insurance or the medicinal supply upon which my life would depend. I was slowly dying and just wanted to kidney, regardless of what would come after” (41). Lastly, we relied on self-report and did not independently validate patients’ financial situation, monthly transplant-related expenses, or medication fees.
Based on the research findings, we recommend that pre-transplant patient informed consent procedures be strengthened by ensuring patient knowledge of the three year limitation on Medicare payment for immunosuppressants. Other research supports this need: 19.5% of 318 kidney recipients did not feel adequately informed of out-of-pocket expenses before their transplant (21). We further recommend improving the financial education and preparation of kidney recipients prior to transplantation and repeatedly throughout the first three years post-transplant. Greater efforts are needed to educate renal transplant recipients about the expenses involved in transplantation, the extent and duration of insurance coverage available, how to effectively interact with insurance companies, and effective strategies for managing transplant-related expenses. Transplant professionals may find it helpful to share the information reported herein on strategies for managing expenses with prospective kidney transplant candidates and recipients to better enable them to financially prepare for living with the transplant. It is unknown how many transplant centers have post-transplant vocational counselors on staff, who have been shown to be effective and cost-effective (39,42). As the stewards of scarce organs for donation, transplant centers should provide services that ensure the effective use of these resources. Greater attention to kidney transplant recipients’ financial preparation and management of the transplant may improve long-term graft survival.
Policy makers should know the range of experiences and difficulties patients experience in financially managing transplant expenses to appreciate the broad impact of policies on patients’ lives and to mitigate any adverse effects (29). Given the adverse impact of transplant-related expenses on patients’ lives, more effective strategies are needed to help patients obtain immunosuppression for the life of the kidney graft and thus foster long-term graft survival.
Future research
Future research should investigate how patients afford their transplant medications after Medicare’s entitlement ends to reveal the shifting role of finances in relation to graft survival in the long-term. While others have called for empirical analysis of financial outcomes of transplantation (43), we posit that such a line of inquiry must also include transplant recipients’ financial experiences as a key variable of analysis. Further studies should be undertaken to better understand the relationship between financial strain and kidney graft function in the US and internationally. A comparative study of healthcare systems and kidney transplant outcomes found that industrialized nations differ in the percentage of patients with functioning renal transplants according to the kind of healthcare system (44). Countries with a public or “Beveridge” Model (e.g., United Kingdom, Canada, Sweden) have the greatest percentage of patients with functioning renal transplants compared to mixed (e.g., Germany, Italy, France) or private countries (e.g., the United States, Japan) (44). Such research supports the notion that the broader health policy context affects how kidney recipients manage the transplant. Nonetheless, the current findings suggest that financial strain may have a negative impact on patients’ ability to engage in self-care management practices essential to transplant success.
Acknowledgments
An earlier version of this article was presented at the AcademyHealth Annual Research Meeting, June 4, 2007 and the Chicago Transplant Ethics Consortium Meeting, Dilemmas and Struggles in Transplantation Ethics, Psychosocial Considerations, and Policy, April 4, 2008. We thank Laura Grillo and Randy Hohle for their research assistance. Thanks also go to Jack Kress for his helpful comments on an earlier version of this manuscript.
Source of support: Dr. Gordon is supported by a Career Development Award from the National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD (DK063953). The authors’ work was independent of the funder.
Funding: Dr. Gordon is supported by the Alden March Bioethics Institute of Albany Medical Center, NY, and by a Career Development Award from the National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD (DK063953).
Footnotes
The email address of the corresponding author may be published.
All requests for reprints should be addressed to the corresponding author.
Contributors: EG designed and executed the study and acquired the data. EG and TP conducted analysis and interpretation of data. She is guarantor. EG drafted the article, and EG, TP, and AS revised the article. TP and AS supervised the study. EG, TP, and AS gave final approval.
Ethical approval: This study was approved by Loyola University Medical Center and Albany Medical Center.
Contributor Information
Elisa J. Gordon, Research Associate Professor, Institute for Healthcare Studies and Department of Surgery, Feinberg School of Medicine, Northwestern University, 750 North Lake Shore Drive, 10th Floor, Chicago, IL 60611.
Thomas R. Prohaska, Professor of Public Health, Co-Director, Center for Research on Health and Aging, Institute for Health Research and Policy (MC 275), School of Public Health, University of Illinois at Chicago, 1747 West Roosevelt Road, Room 558, Chicago, IL 60608.
Ashwini R. Sehgal, Professor of Medicine, Biomedical Ethics, and Epidemiology & Biostatistics, Director of the Center for Reducing Health Disparities, Division of Nephrology, Rammelkamp Center 228A, MetroHealth Medical Center, 2500 MetroHealth Drive, Cleveland, OH 44109, Submitted for Publication in Clinical Transplantation.
References
- 1.Colm CM, Pascual M. Update in renal transplantation. Arch Intern Med. 2004;164:1373. doi: 10.1001/archinte.164.13.1373. [DOI] [PubMed] [Google Scholar]
- 2.Butkus DE, Mayedrech EF, Raju SS. Racial differences in the survival of cadaver renal allografts – Overriding effects of HLA matching and socioeconomic factors. N Engl J Med. 1992;327:840. doi: 10.1056/NEJM199209173271203. [DOI] [PubMed] [Google Scholar]
- 3.Koyama H, Cecka JM, Terasa PI. Kidney transplants in black recipients: HLA matching and other factors affecting long-term graft survival. Transplantation. 1994;57:1064. [PubMed] [Google Scholar]
- 4.Kasiske BL, Cohen D, Lucey MR, Neylan MD. Payment for immunosuppression after organ transplantation. JAMA. 2000;283:2445. doi: 10.1001/jama.283.18.2445. [DOI] [PubMed] [Google Scholar]
- 5.Social Security Amendments of 1972, Pub. L. No. 92–603, 86 Stat. 1329 (1972). Section 2991, October 30, 1972.
- 6.Department of Health and Human Services. Memorandum from Director-Office Program Operations Procedures, BPO, to Associate Regional Administrators for Medicare, 7 December 1994. URL: [ http://www.transweb.org/reference/articles/hrd.html] Accessed January 3, 2006.
- 7.Thamer M, Henderson SC, Ray NF, Rinehart CS, Greer JW, Danovitch GM. Unequal access to cadaveric kidney transplantation in California based on insurance status. Health Serv Res. 1999;34:879. [PMC free article] [PubMed] [Google Scholar]
- 8.The 109th Congress Considered Bill S. 173, The Comprehensive Immunosuppressive Drug Coverage for Transplant Patients Act of 2005. [Designed to expand coverage for Medicare beneficiaries for the life of the kidney.]
- 9.Manninen DL, Evans RW, Dugan MK. Work disability, functional limitations, and the health status of kidney transplantation recipients post transplant. Clin Transplant. 1991;5:193. [PubMed] [Google Scholar]
- 10.Powe NR. To have and have not: health and health care disparities in chronic kidney disease. Kidney Int. 2003;64:763. doi: 10.1046/j.1523-1755.2003.00138.x. [DOI] [PubMed] [Google Scholar]
- 11.Laupacis A, Keown P, Pus N, Krueger H, Ferguson B, Wong C, Muirhead N. A study of the quality of life and cost-utility of renal transplantation. Kidney Int. 1996;50:235. doi: 10.1038/ki.1996.307. [DOI] [PubMed] [Google Scholar]
- 12.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 13.Loubeau PR, Loubeau JM, Jantzen R. The economics of kidney transplantation versus hemodialysis. Prog Transplant. 2001;11:291. doi: 10.1177/152692480101100411. [DOI] [PubMed] [Google Scholar]
- 14.Woodward RS, Schnitzler MA, Lowell JA, Spitznagel EL, Brennan DC. Effect of extended coverage of immunosuppressive medications by Medicare on the survival of cadaveric renal transplants. Am J Transplant. 2001;1:69. doi: 10.1034/j.1600-6143.2001.010113.x. [DOI] [PubMed] [Google Scholar]
- 15.Yen EF, Hardinger K, Brennan DC, Woodward RS, Desai NM, Crippin JS, et al. Cost-effectiveness of extending Medicare coverage of immunosuppressive medications to the life of a kidney transplant. Am J Transplant. 2004;4:1703. doi: 10.1111/j.1600-6143.2004.00565.x. [DOI] [PubMed] [Google Scholar]
- 16.Kaló Z. Economic aspects of renal transplantation. Transplant Proc. 2003;35:1223. doi: 10.1016/s0041-1345(03)00199-4. [DOI] [PubMed] [Google Scholar]
- 17.Gordon EJ. The ethics of Medicare policy: Increasing transplant access and survival. DePaul Law Review. 2006;54:101. [PMC free article] [PubMed] [Google Scholar]
- 18.Rao PS, Schaubel DE, Jia X, Li S, Port FK, Saran R. Survival on dialysis post-kidney transplant failure. Am J Kidney Dis. 2007;49:294. doi: 10.1053/j.ajkd.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 19.Hariharan A, McBride MA, Cherikh WS, Tolleris CB, Bresnahan BA, Johnson CP. Post-transplant renal function in the first year predicts long-term kidney transplant survival. Kidney Int. 2002;62:311. doi: 10.1046/j.1523-1755.2002.00424.x. [DOI] [PubMed] [Google Scholar]
- 20.Adams PL. Long term patient survival: Strategies to improve overall health. Am J Kidney Dis. 2006;4:S65. doi: 10.1053/j.ajkd.2005.12.043. [DOI] [PubMed] [Google Scholar]
- 21.Rodrigue JR, Reed AI, Nelson DR, Jamieson I, Kaplan B, Howard RJ. The financial burden of transplantation: A single-center survey of liver and kidney transplant recipients. Transplantation. 2007;84:295. doi: 10.1097/01.tp.0000269797.41202.79. [DOI] [PubMed] [Google Scholar]
- 22.Kasiske BL, Chakkera HA, Louis Ta, Ma JZ. A Meta-Analysis of immunosuppression withdrawal trials in renal transplantation. J Am Soc Nephrol. 2000;11:1910. doi: 10.1681/ASN.V11101910. [DOI] [PubMed] [Google Scholar]
- 23.Markell MS, DiBenedetto A, Maursky V, Sumrani N, Hong JH, Distant DA, et al. Unemployment in inner-city renal transplant recipients: Predictive and sociodemographic factors. Am J Kidney Dis. 1997;29:881. doi: 10.1016/s0272-6386(97)90462-5. [DOI] [PubMed] [Google Scholar]
- 24.Steptoe A, Brydon L, Kunz-Ebrecht S. Changes in financial strain over three years, ambulatory blood pressure, and cortisol responses to awakening. Psychosom Med. 2005;67:281. doi: 10.1097/01.psy.0000156932.96261.d2. [DOI] [PubMed] [Google Scholar]
- 25.Solotaroff R, Devoe J, Wright BJ, Smiths J, Boone J, Edlund T, et al. Medicaid programme changes and the chronically ill: Early results from a prospective cohort study of the Oregon health plan. Chronic Illn. 2005;3:191. doi: 10.1177/17423953050010030301. [DOI] [PubMed] [Google Scholar]
- 26.Ahnquist J, Fredlund P, Wamala SP. Is cumulative exposure to economic hardships more hazardous to women’s health than men’s? A 16-year Follow-up Study of the Swedish Survey of Living Conditions. J Epidemiol Community Health. 2007;61:331. doi: 10.1136/jech.2006.049395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blank N, Burstrom B. Limiting long-term illness and the experience of financial strain in Sweden. Scand J Public Health. 2002;30:41. [PubMed] [Google Scholar]
- 28.Heymann SJ. Health and social policy. In: Berkman L, Kawachi I, editors. Social Epidemiology. Oxford: Oxford University Press; 2000. p. 368. [Google Scholar]
- 29.Rist RC. Influencing the policy process with qualitative research. In: Denzin NK, Lincoln YS, editors. Handbook of Qualitative Research. Thousand Oaks, CA: Sage Publications; 1994. p. 545. [Google Scholar]
- 30.Cho YW, Terasaki PI, Cecka JM. New variables reported to the UNOS registry and their impact on cadaveric renal transplant outcomes—a preliminary study. Clin Transpl. 1995:405. [PubMed] [Google Scholar]
- 31.Pearlin LI, Lieberman MA. Social Sources of Emotional Distress. In: Simmons R, editor. Research in Community and Mental Health. Vol. 1. Greenwich, Ct: JAI Press; 1979. p. 217. [Google Scholar]
- 32.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The Stress Process. J Health Soc Behav. 1981;22:337. [PubMed] [Google Scholar]
- 33.Luborsky M. The identification and analysis of themes and patterns. In: Gubrium JF, Sankar A, editors. Qualitative Methods in Aging Research. Thousand Oaks, CA: Sage Publications; 1994. p. 189. [Google Scholar]
- 34.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Serv Res. 2007;42:1758. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- 36.United Network for Organ Sharing. Transplants in the U.S. by Recipient Gender, Ethnicity, and Age. URL: [ http://www.optn.org/latestData/rptData.asp] Accessed 8-28-07. Based on OPTN data as of August 28, 2007.
- 37.Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med. 2006;21:995. doi: 10.1111/j.1525-1497.2006.00516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rhodes R. Justice in transplant organ allocation. In: Rhodes R, Battin MP, Silvers A, editors. Medicine and Social Justice: Essays on the Distribution of Health Care. New York: Oxford University Press; 2002. p. 345. [Google Scholar]
- 39.Carter JM, Winsett RP, Rager D, Hathaway DK. A center-based approach to a transplant employment program. Prog Transplant. 2000;10:204. doi: 10.1177/152692480001000403. [DOI] [PubMed] [Google Scholar]
- 40.Rettig RA, Sadler JH. Measuring and improving the health status of end stage renal disease patients. Health Care Financ Rev. 1997;18:77. [PMC free article] [PubMed] [Google Scholar]
- 41.Trump E. My cure is killing me. George Magazine. 2001 December/January; (no longer in circulation). Re-published in Utne Reader 2007 October 9. [URL: ( http://www.utne.com/archives/MyCureisKillingMe.aspx) accessed May 14, 2008]
- 42.Chang CF, Winsett RP, Gaber AO, Hathaway DK. Cost-effectiveness of post-transplantation quality of life intervention among kidney recipients. Clin Transplant. 2004;18:407. doi: 10.1111/j.1399-0012.2004.00181.x. [DOI] [PubMed] [Google Scholar]
- 43.Abecassis MM. Financial outcomes in transplantation—A provider’s perspective. Am J Transplantation. 2006;6:1257. doi: 10.1111/j.1600-6143.2006.01329.x. [DOI] [PubMed] [Google Scholar]
- 44.Hörl WH, de Alvaro F, Wiliams PF. Healthcare systems and end-stage renal disease (ESRD) therapies—an international review: Access to ESRD. Treatment Nephrol Dial Transplant. 1999;14:10. doi: 10.1093/ndt/14.suppl_6.10. [DOI] [PubMed] [Google Scholar]