Abstract
The concept and need for a gender-specific or female-specific total knee prosthesis have generated interest and discussion in the orthopaedic community and the general public. This concept relies on the assumption of a need for such a design and the opinion that there are major anatomic differences between male and female knees. Most of the information regarding this subject has been disseminated through print and Internet advertisements, and through direct-to-patient television and magazine promotions. These sources and a recent article in a peer-reviewed journal, which support the need for a female-specific implant design, have proposed three gender-based anatomic differences: (1) an increased Q angle, (2) less prominence of the anterior medial and anterior lateral femoral condyles, and (3) reduced medial-lateral to anterior-posterior femoral condylar aspect ratio. We examined the peer-reviewed literature to determine whether women have had worse results than men after traditional TKAs. We found women have equal or better results than men. In addition, we reviewed the evidence presented to support these three anatomic differences. We conclude the first two proposed differences do not exist, and the third is so small that it likely has no clinical effect.
Level of Evidence: Level IV, systematic review. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Female-specific total knee implants have been marketed and promoted to orthopaedic surgeons and their patients despite a paucity of evidence-based, peer-reviewed information. Of two recent medical journal articles that advocated a female-specific knee design, one was an interview with the implant’s designer or consultant [6] and the other was a news release authored by a reporter quoting two designers or consultants of the prosthesis [9]. Neither article was peer-reviewed. The authors of two additional articles have advocated a prosthetic design that incorporated female-specific sizing. Both were published in peer-reviewed journals but authored by the designers or consultants. One article had no conflict of interest statement [18] and the second was published with a very narrowly defined conflict of interest statement [15].
The Journal of the American Academy of Orthopaedic Surgeons published an article that put forward three anatomic differences between men’s and women’s knees and specifically advocated a female-specific implant designed to address these differences [11]. The senior author (SC) was the Chief Marketing Officer for the manufacturer, and the two junior authors (AR, RC) were designers or consultants. Five months later, the same journal published an anonymous article entitled “Gender-specific Knee Replacements: A Technology Overview” [2]. No conflict of interest statement was included for the anonymous authors. The concept of a female-specific total knee implant design is based on the theory that there are clinically important morphologic differences between male and female knees and that traditional designs have failed to address these differences, implying the results of TKA are worse for women than for men. If the advocates for female-specific knee prosthetic designs, ie, separate designs for men and women, are correct, the evidence for this claim should have been revealed in prior outcome and survivorship studies. That is, comparative outcomes should dictate whether a female-specific prosthetic design is needed or even desirable.
The purpose of this article is twofold: to perform a thorough review of the peer-reviewed orthopaedic literature to locate any published evidence that the results of TKA are different in women and men and to analyze the evidence for the male-female anatomic differences advanced to support the need for a female-specific implant design. Presuming these anatomic differences between men and women are clinically important, we hypothesized traditional total knee designs based on average anthropomorphic measurements from men and women would show worse results for women than for men.
Search Strategy and Criteria
We (ACM) searched the MEDLINE® database using the following search string: “Arthroplasty, Replacement, Knee” [MeSH] AND (survivorship OR results OR durability OR wear OR osteolysis). We limited the search to articles published in English from 1989 to 2007. We recovered 2381 citations. Three of us (ACM, RPG, SFD) screened for inappropriate studies about unicompartmental, patellofemoral, and revision arthroplasties, papers that did not address gender differences, and other irrelevant studies, leaving 86 citations. One of us (RAT) examined the articles that included hip and knee arthroplasties and reduced that number to 80. Finally, two of us (EAA, WBL) excluded studies with fewer than 400 TKAs leaving 29 papers. Our exclusion criteria for length of followup depended on the goal of each study. For those that assessed survivorship, wear-related failures, revision rate, patient satisfaction, and outcome scores, we required at least a 5-year followup. For papers that evaluated factors that likely would remain static after 2 years, such as pain, range of motion, and stiffness, we required a 2-year minimum followup. Two of us (MF, WRP) examined the 29 papers using these criteria, leaving 19 studies for full review.
Search Results
Women did not have worse outcomes than men using traditional total knee designs. In fact, we found the women achieve essentially equal results compared with men, and in many studies, their results were better. We found no papers specifically designed to study differences between men and women. Ten studies reported results in a numeric, statistical form (Table 1). Eight of these papers [3, 12, 19, 29, 30, 32, 34, 36] totaling 77,449 TKAs with 5- to 15-year followups showed women have better results than men. One study [33] using a simplified, subjective, patient-reported satisfaction survey with a 6-year followup reported 84.5% of men were either satisfied or very satisfied after their TKA compared with 84.0% of women. This small 0.5% difference in a very simple and subjective survey was not clinically important. Ritter et al. [31] reported women had 1.9° less range of motion than men. No calculations were provided for possible interobserver error, which may have accounted for this difference, and this small difference did not appear to be clinically important. The remaining nine studies (Table 2) did not report their results regarding male-female differences in a numeric form. Instead they used phrases such as “male and female patients had similar outcomes,” “gender did not affect outcomes,” or “no significant differences were found between men and women.” All nine studies reported no difference between the results of men and women.
Table 1.
Studies of primary TKAs reporting significant male-female differences
| Study | Total TKAs | Males | Females | Male knees | Female knees | Criteria | Result | p Value |
|---|---|---|---|---|---|---|---|---|
| Rand and Illstrup [29], 1991 | 9200 | NNG | NNG | 3544 | 5656 | Implant survival at 10 years | M = 76%F = 83% | 0.0001 |
| Robertsson et al. [33], 2000 | 24,368 | NNG | NNG | 7191 | 17,177 | Patient satisfaction at 6 years | M = 85.0%F = 84.5% | 0.001 |
| Robertsson et al. [34], 2001 | 41,223 | NNG | NNG | 13,611 | 27,612 | Relative risk for revision at 10 years | M > FRelative risk = 1.5 | 0.01 |
| Vazquez-Vela Johnson et al. [36], 2003 | 559 | NNG | NNG | 188 (OA) | 340 (OA) | Implant survival, OA, at 10 years | M = 95%F = 99% | 0.042 |
| Rand et al. [30], 2003 | 11,606 | 3701 | 4589 | NNG | NNG | Implant survival at 10 years | M = 88%F = 93% | 0.0001 |
| Ritter et al. [31], 2003 | 4724 | NNG | NNG | 1929 | 2798 | Postoperative range of motion at 3 years | Flexion: M = 1.9° > F | < 0.0001 |
| Fehring et al. [12], 2004 | 1287 | 627 | 1110 | NNG | NNG | Implant failure at 5–13 years | M risk = 2.8 times > F risk | < 0.0001 |
| Himanen et al. [19], 2005 | 8467 | 1586 | 5623 | 1839 | 6628 | Implant survival at 10 years | M = 93%F = 94% | 0.01 |
| Roberts et al. [32], 2007 | 4606 | 1590 | 2800 | NNG | NNG | Implant survival at 15 years | M = 90%F = 94% | 0.001 |
| Baker et al. [3], 2007 | 501 | 172 | 224 | NNG | NNG | Implant failure at 15 years (hazard risk) | M hazard risk = 2.48 | 0.004 |
M = male; F = female; NNG = number not given; OA = osteoarthritis.
Table 2.
Studies of primary TKAs reporting no significant male-female differences
| Study | Total TKAs | Males | Females | Male knees | Female knees | Followup (years) | Criteria | Result: male/female difference |
|---|---|---|---|---|---|---|---|---|
| Scuderi et al. [35], 1989 | 1430 | NNG | NNG | 445 | 985 | 2–15 | Implant survivorship | No significant difference |
| Whiteside [37], 1991 | 724 | NNG | NNG | 339 | 385 | 2 | Pain relief | No significant difference |
| Font-Rodriguez et al. [13], 1997 | 2629 | NNG | NNG | 789 | 1840 | 2–22 | Implant survivorship | No significant difference |
| Gill and Joshi [14], 2001 | 404 | 120 | 208 | NNG | NNG | 2–17 | Implant survivorship | No significant difference |
| Khaw et al. [24], 2002 | 501 | 172 | 224 | NNG | NNG | 3–13 | Implant survivorship | No significant difference |
| Kim et al. [25], 2004 | 1000 | 337 | 644 | NNG | NNG | 3 | Stiffness | No significant difference |
| Wright et al. [39], 2004 | 523 | 130 | 277 | NNG | NNG | 2–15 | Outcome scores | No significant difference |
| Kane et al. [23], 2005 (meta-analysis of 62 studies) | > 100 per study | 34.6% | 65.4% | NNG | NNG | Variable or no data | Outcome scores | No significant difference |
| Bourne et al. [7], 2007 | 843 | 292 | 436 | NNG | NNG | 5–11 | Outcome scores | No significant difference |
NNG = number not given.
We also found no evidence to support a claim that there are anatomic differences between men’s and women’s knees that would justify a female-specific total knee implant design.
At the time of our literature search for this review, we identified only one peer-reviewed article, by Conley et al. [11], that advocated the need for a female-specific total knee design. The authors of that article used the term “notable” to describe three anatomic variations of the female knee compared with the male knee. To evaluate that article, we studied the evidence presented by the authors to support each of these three differences: (1) an increased Q angle, (2) less prominent anterior medial and lateral femoral condyles, and (3) a reduced medial-lateral to anterior-posterior (ML:AP) femoral condylar aspect ratio.
The Q Angle
We recognize the true Q angle (first described by Brattstrom [8]) as the complimentary angle formed between the patellar tendon and the resultant line of force of the quadriceps muscles. Because this resultant line of force is impossible to measure clinically, it is commonly accepted that a line from the anterior superior iliac spine to the center of the patella acts as a substitute. It is this anatomic Q angle discussed in this analysis.
In support of their theory that women have a larger Q angle than men, Conley et al. [11] listed six peer-reviewed references [1, 17, 21, 22, 26, 38]. An examination of these references is important. In 1989, Livingston [26] reviewed prior studies and summarized the conclusions of those studies. No original data were presented. Conley et al. [11] used this reference to validate their statement: “Women are typically shorter than men, with wider hips and a larger Q angle, …” However, after a thorough literature review, Livingston concluded in part: “The common belief that women have wider hips than men is not supported by scientific data, nor is the assumption that Q angles are bilaterally symmetric. These outdated assumptions must be replaced by a new approach to the study of the Q angle” [26]. Guerra et al. [17] reported the average Q angle was 5.8° greater for women than for men. However, despite having collected height data for all subjects, the authors failed to correct for the average height difference between men and women. Woodland and Francis [38] reported a 3° mean difference but also did not correct for the average height difference between men and women. Aglietti et al. [1] also reported a small 3° mean difference but again did not correct for the smaller stature of women. Horton and Hall [21] determined the average female Q angle to be 4.6° larger than that of the male. Once again, these authors did not correct for differences in height. Hsu et al. [22] also reported a 3.2° difference, with females being larger than males. These authors did not perform reproducibility measurements nor did they correct for height differences between men and women. Either or both could have accounted for this difference. Furthermore, many of these reports failed to describe the protractor used, report the method of Q angle measurement, and perform reproducibility studies.
Conley et al. [11] omitted any reference to the study by Grelsamer et al. [16]. These authors, using a long, more accurate protractor to reach the anterior superior iliac spine and a standardized measurement method, concluded, when the data are corrected for the difference in average height between men and women, the difference between male and female Q angles disappears. They proved women and men have similar Q angles, and shorter people, whether male or female, have slightly greater Q angles than taller people.
Anterior Condylar Height
Conley et al. [11] contended “…that the female has a less pronounced anterior condylar height than does the male knee” and offered two references in support [28, 40]. During 100 consecutive TKAs, Poilvache et al. [28] measured the thickness of the anterior lateral and anterior medial resected bone after making the anterior cut (Fig. 1). These authors reported an average 1.4 mm lower lateral condyle and a 1.6 mm lower medial condyle for females compared with males. These data were direct, absolute measurements, uncorrected for the size of the distal femur or the patient. The authors clearly recognized these differences were the result of size and not gender by stating, “The anterior extent of the trochlea was smaller in females, but this difference can be explained by the smaller size of the femurs.” When Brattstrom [8] performed a detailed radiographic-anatomic study of 200 normal subjects measuring 400 knees (half of the subjects were women) and found women had, on average, 1.5 mm lower lateral and 1.1 mm lower medial condyles anteriorly, he attributed this difference to the smaller size and stature of women. When corrected for size, men and women have similar anterior condylar measurements. Their second supporting reference [40] was to a commercial Internet Web site advertising a particular female-specific knee implant system that contained no independent supporting data.
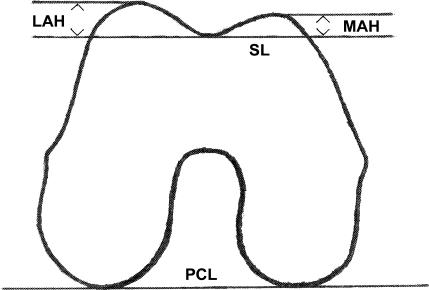
Fig. 1.
This diagram depicts a cross section of the distal femur. PCL = posterior condylar line; SL = sulcus line (parallel to PCL; represents the anterior cut during TKA); LAH = lateral anterior height; MAH = medial anterior height. The average anterior lateral condyle height and anterior medial condyle height for men are 13.7 mm and 10.6 mm, respectively, whereas those for women are 12.3 mm and 9.0 mm, respectively.
Conley et al. [11] hypothesized using implants sized to demographic averages “may result in a patellofemoral joint that feels tight or ‘overstuffed’ after surgery and limit postoperative range of motion.” Of the three references cited to support this possibility, only two were published [5, 20]. Hitt et al. [20] investigated male-female differences in the ML:AP aspect ratio. They did not investigate or discuss anterior condylar height differences nor did they investigate or discuss the possibility of decreased range of motion or “tightness” postoperatively in women. Bengs and Scott [5] reported a relatively small and insignificant decrease in range of motion intraoperatively relative to increasing patellar thickness.
The ML:AP Aspect Ratio
To support their theories of a lower anterior condylar height and reduced ML:AP aspect ratio, Conley et al. [11] referred to a “proprietary three-dimensional tomography analysis technology” of Mahfouz et al. We were not able to review that reference because it was not published. As mentioned above, Hitt et al. [20] did not investigate anterior condylar height; however, they did design and perform an excellent multicenter study to compare detailed and accurate measurements of the distal femur and proximal tibia intraoperatively with the dimensions of the prostheses to be implanted. Eight centers participated, and six different prosthetic knee systems were analyzed. They measured 337 knees in 295 patients; 209 (62%) of the knees were female and 128 (38%) were male. They found the distal femoral female ML:AP aspect ratio was smaller than that of the male and there was significant variation among the different implants in accommodating that difference, especially in the smaller sizes. They hypothesized this mismatch “could result in soft tissue irritation,” “effect balancing efforts,” “leave exposed cancellous bone,” “and may permit increased osteolysis from wear debris in longer follow-up” However, they knew of no report that “has specifically addressed this issue.”
Discussion
By reviewing the peer-reviewed orthopaedic literature regarding traditional, primary TKA, we tried to determine whether women had worse results than men using various criteria for success or failure. We also sought any evidence to determine whether there are skeletal differences between men’s and women’s knees, and if so, that these differences would be clinically important. Those who propose a need for a female-specific total knee design [6, 11] should be able to support that proposal with clinical and scientific evidence published with genuine peer review in an evidence-based format without bias. If studies that used traditional, averaged, gender-neutral total knee designs found worse results for women than for men, then the need for female-specific designs might be inferred. However, just the opposite is true. The results from such studies show women achieve results that are at least as good as or, more likely, better than men. Thus, we see, no matter what criteria are used to measure success or failure by the multiple studies about primary TKA (Tables 1, 2), whether it is by implant survival [13, 14, 19, 24, 29, 30, 35, 36], pain [37], risk of revision [34], range of motion [31], wear-related failures [3, 12], stiffness [25], outcomes scores [7, 23, 39], or satisfaction [33], when traditional implant designs are used, women achieve essentially equal or even better results than men. This finding refutes the theory that traditional knee prosthetic designs place women at a disadvantage compared with men and that gender-specific designs are needed to address anatomic differences between men and women.
A limitation of our literature search was that we found no study specifically designed to ascertain difference between the results of men and women using traditional total knee designs. Therefore, we had to rely on authors who were gathering data for other reasons to report any male-female differences. Certainly, studies that reported such differences numerically with significant probability values (Table 1) were more reliable than those that did not (Table 2). However, the fact that our search discovered no studies specifically designed to test for possible male-female differences is instructive. If being female were an obvious risk factor for premature failure or poor outcome, we suspect studies would have been performed to document this risk and its magnitude. Ideally, a long-term study with a large cohort could be designed to specifically answer the question: Are the TKA results worse in females than males? However, the data we have reported seem to leave no question that women’s results are the same or better than those of men.
When the data supporting major anatomic differences in the Q angle between male and female knees are reviewed carefully, it becomes apparent this difference disappears when corrected for the average height difference between men and women. Indeed, Grelsamer et al. [16] reported the female pelvis is not wider than the male pelvis when measured between the anterior superior iliac spines. Furthermore, in a subject of average height, because the anterior superior iliac spine is so far from the patella, a 4-cm-wider pelvis would only change the Q angle 2°. Conversely, a 5° increase in the Q angle would require almost a 9-cm-wider pelvis. By using a long, more accurate protractor and a consistent, standardized method of measurement, they also reported the Q angle changed 0.2° for each centimeter in height, and the average height difference of 11.5 cm between men and women explained the small 2.3° gender difference in the Q angle. With this information, implant designers might advocate height-specific designs, but not gender- or female-specific designs.
Concerning the claim that the medial and lateral condyles have smaller anterior heights in women compared with men, this difference is explained entirely by size and not gender difference. We found no evidence to support the claim that using implants sized to demographic averages will result in overstuffing of the patellofemoral joint. The concept of overstuffing the patellofemoral joint has been simply and uncritically transferred from the femorotibial joint with no confirmatory studies. Because the capsule and inelastic ligaments secure the femorotibial joint, it is extremely important to balance these ligaments carefully during TKA and avoid a tibial insert that is too large. This will certainly overstuff this joint and lead to a poor result with decreased range of motion. The patellofemoral joint is a totally different articulation. Although the patellar ligament is inelastic, the quadriceps muscles are elastic and stretchable. This explains why the investigation by Bengs and Scott [5] not only failed to support the claim of overstuffing by Conley et al. [11], but actually refuted it. More recently, Pierson et al. [27] reviewed 830 primary TKAs to determine the effects of so-called overstuffing the patellofemoral joint. Their findings did “not support the widely held belief that stuffing of the patellofemoral joint results in adverse outcomes after total knee arthroplasty.”
With reference to the smaller female ML:AP aspect ratio of the distal femur, there is no scientific or clinical evidence to show it has a major clinical impact. Hitt et al. [20] clearly showed women have a smaller ML:AP aspect ratio on average than men. One reason this difference may not rise to clinical significance is that the differences within groups of men and women are greater than the differences between men and women. That is, the mean difference between groups is almost always smaller than the standard deviations of the measurements within the groups. Because we found women achieve essentially the same or better results after traditional TKA compared with men in 19 studies with more than 120,000 TKAs spanning 18 years, we conclude this smaller female ML:AP aspect ratio has no measurable clinical effect. Other designers [18] have used the same data presented by Hitt et al. [20] to improve the sizing options for men and women in the same implant system. They decreased the ML:AP aspect ratio in the smaller sizes and decreased the increment change between sizes, thereby offering more options in the same overall range. They rejected the concept of female-specific total knee designs and in their early short-term study have reported successful results for men and women [18]. Barrett [4] studied the need for gender-specific prostheses in TKA, taking into consideration the smaller female ML:AP aspect ratio. He concluded, although some modification of sizing within current total knee systems might be beneficial, the development of separate designs for men and women would likely be costly and unnecessary. Chin et al. [10] reached the same conclusion after studying intraoperative measurements of male and female distal femurs. They confirmed a 2% to 3% difference in the aspect ratio between men and women and suggested prosthetic manufacturers use these data to produce “…a range of prosthetic sizes that provides more optimum fit across genders…” We agree the availability of more sizes may produce a better anatomic fit for more patients, and this might improve functional or survivorship results; however, that too remains speculative.
The use of female-specific total knee designs poses an interesting ethical and, perhaps, medicolegal dilemma. When obtaining informed consent, should the orthopaedic surgeon disclose to the male patient that he or she plans to use an implant that was designed and intended for use in the female knee? Conversely, should he or she explain to the female patient that there is no scientific or clinical evidence to support the use of this new female-specific total knee prosthetic design?
After a thorough review and analysis of the literature regarding traditional primary TKA, no matter what criteria were used to define success or failure, we found no evidence to support the original hypothesis that women traditionally have worse outcomes than men. On the contrary, women appear to have the same or better results than men. In addition, the average anatomic differences between male and female knees can be explained by the average smaller height and size of women compared with men, not by their gender. The difference in the distal femoral aspect ratio described by Hitt et al. [20] is apparently too small to be of clinical importance. We conclude the need for female- or gender-specific total knee prosthetic designs is not supported by existing scientific and clinical evidence.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11999-008-0650-4
References
- 1.Aglietti P, Insall JN, Cerulli G. I. Measurements of incongruence. Clin Orthop Relat Res. 1983;176:217–224. [PubMed]
- 2.Anonymous. Gender-specific knee replacements: a technology overview. J Am Acad Orthop Surg. 2008;16:63–67. [PubMed]
- 3.Baker PN, Khaw FM, Kirk LM, Esler CN, Gregg PJ. Randomized controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg Br. 2007;89:1608–1614. [DOI] [PubMed]
- 4.Barrett W. The need for gender-specific prostheses in TKA: does size make a difference? Orthopedics. 2006;29(suppl):S53–S55. [PubMed]
- 5.Bengs BC, Scott RD. The effect of patellar thickness on intraoperative knee flexion and patellar tracking in total knee arthroplasty. J Arthroplasty. 2006;21:650–655. [DOI] [PubMed]
- 6.Booth RE Jr. The gender-specific (female) knee. Orthopedics. 2006;29:768–769. [DOI] [PubMed]
- 7.Bourne RB, McCalden RW, MacDonald SJ, Mokete L, Guerin J. Influence of patient factors on TKA outcomes at 5 to 11 years follow-up. Clin Orthop Relat Res. 2007;464:27–31. [DOI] [PubMed]
- 8.Brattstrom H. Shape of the intercondylar groove normally and in recurrent dislocation of the patella; a clinical and x-ray anatomical investigation. Acta Orthop Scand Suppl. 1964;68:1–148. [PubMed]
- 9.Brooks J. Gender-specific knees. CMAJ. 2007;176:309–310. [DOI] [PMC free article] [PubMed]
- 10.Chin KR, Dalury DF, Zurakowski D, Scott RD. Intra-operative measurements of male and female distal femurs during primary total knee arthroplasty. J Knee Surg. 2002;15:213–217. [PubMed]
- 11.Conley S, Rosenberg A, Crowninshield R. The female knee: anatomic variations. J Am Acad Orthop Surg. 2007;15(suppl 1):S31–S36. [DOI] [PubMed]
- 12.Fehring TK, Murphy JA, Hayes TD, Roberts DW, Pomeroy DL, Griffin WL. Factors influencing wear and osteolysis in press-fit condylar modular total knee replacements. Clin Orthop Relat Res. 2004;428:40–50. [DOI] [PubMed]
- 13.Font-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79–86. [DOI] [PubMed]
- 14.Gill GS, Joshi AB. Long-term results of kinematic condylar knee replacement. J Bone Joint Surg Br. 2001;83:355–358. [DOI] [PubMed]
- 15.Greene KA. Gender-specific design in total knee arthroplasty. J Arthroplasty. 2007;22:27–31. [DOI] [PubMed]
- 16.Grelsamer RP, Dubey A, Weinstein CH. Men and women have similar Q angles. J Bone Joint Surg Br. 2005;87:1498–1501. [DOI] [PubMed]
- 17.Guerra JP, Arnold MJ, Gaidosik RL. Q angle: effects of isometric quadriceps contraction and body position. J Orthop Sports Phys Ther. 1994;19:200–204. [DOI] [PubMed]
- 18.Harwin SF, Greene KA, Hitt K. Early experience with a new total knee implant: maximizing range of motion and function with gender-specific sizing. Surg Technol Int. 2007;16:199–205. [PubMed]
- 19.Himanen AK, Belt E, Nevalainen J, Hämäläinen M, Lehto MU. Survival of the AGC total knee arthroplasty is similar for arthrosis and rheumatoid arthritis: Finnish Arthroplasty Register report on 8,467 operations carried out between 1985 and 1999. Acta Orthop. 2005;76:85–88. [DOI] [PubMed]
- 20.Hitt K, Shurman JR II, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA. Anthropomorphic measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003;85(suppl 4):115–122. [PubMed]
- 21.Horton MG, Hall TL. Quadriceps femoris muscle angle: normal values and relationships with gender and selected skeletal measures. Phys Ther. 1989;69:897–901. [DOI] [PubMed]
- 22.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed]
- 23.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2005;87:1719–1724. [DOI] [PubMed]
- 24.Khaw FM, Kirk LM, Morris RW, Gregg PJ. A randomized, controlled trial of cemented versus cementless press-fit condylar total knee replacement: ten-year survival analysis. J Bone Joint Surg Br. 2002;84:658–666. [DOI] [PubMed]
- 25.Kim J, Nelson CL, Lotke PA. Stiffness after total knee arthroplasty: prevalence of the complication and outcomes of revision. J Bone Joint Surg Am. 2004;86:1479–1484. [DOI] [PubMed]
- 26.Livingston LA. The quadriceps angle: a review of the literature. J Orthop Sports Phys Ther. 1998;28:105–109. [DOI] [PubMed]
- 27.Pierson JL, Ritter MA, Keating EM, Faris PM, Meding JB, Berend ME, Davis KE. The effect of stuffing the patellofemoral compartment on the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2007;89:2195–2203. [DOI] [PubMed]
- 28.Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:35–44. [DOI] [PubMed]
- 29.Rand JA, Ilstrup DM. Survivorship analysis of total knee arthroplasty: cumulative rates of survival of 9,200 total knee arthroplasties. J Bone Joint Surg Am. 1991;73:397–409. [PubMed]
- 30.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85:259–265. [DOI] [PubMed]
- 31.Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME. Predicting range of motion after total knee arthroplasty: clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am. 2003;85:1278–1285. [DOI] [PubMed]
- 32.Roberts VI, Esler CN, Harper WM. A 15-year follow-up study of 4,606 primary total knee replacements. J Bone Joint Surg Br. 2007;89:1452–1456. [DOI] [PubMed]
- 33.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262–267. [DOI] [PubMed]
- 34.Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975–1997: an update with special emphasis on 41,223 knees operated on in 1988–1997. Acta Orthop Scand. 2001;72:503–513. [DOI] [PubMed]
- 35.Scuderi GR, Insall JN, Windsor RE. Survivorship of cemented knee replacements. J Bone Joint Surg Br. 1989;71:798–803. [DOI] [PubMed]
- 36.Vazquez-Vela Johnson G, Worland RL, Keenan J, Norambuena N. Patient demographics as a predictor of the ten-year survival rate in primary total knee replacement. J Bone Joint Surg Br. 2003;85:52–56. [DOI] [PubMed]
- 37.Whiteside LA. The effect of patient age, gender, and tibial component fixation on pain relief after total knee arthroplasty. Clin Orthop Relat Res. 1991;271:21–27. [PubMed]
- 38.Woodland LH, Francis RS. Parameters and comparisons of the quadriceps angle of college-aged men and women in the supine and standing positions. Am J Sports Med. 1992;20:208–211. [DOI] [PubMed]
- 39.Wright RJ, Sledge CB, Poss R, Ewald FC, Walsh ME, Lingard EA. Patient-reported outcome and survivorship after Kinemax total knee arthroplasty. J Bone Joint Surg Am. 2004;86:2464–2470. [DOI] [PubMed]
- 40.Zimmer Gender Solutions Knee. Available at: http://genderknee.com/micro/ctl?op=global&action=1&id=9508&global=1&template=mn. Accessed July 25, 2007.