Abstract
Background
Breast reconstruction after mastectomy is associated with social, psychological and physical benefits. Barriers to breast reconstruction in the United States include age, stage of disease, socioeconomic status and geographic location; however, little is known about the effects of these factors in the Canadian context of a universal health care system. We sought to determine the rate of breast reconstruction in Nova Scotia, identify characteristics influencing access to the procedure and describe the rates of different reconstructive options.
Methods
We conducted a retrospective cohort study involving all women in Nova Scotia who received diagnoses of breast cancer and had mastectomies between 1991 and 2001. We linked data from 2 administrative databases and performed analyses for each year in the study period. We followed the women until the end of the study period (2001). We used logistic regression to evaluate potential barriers to reconstruction.
Results
A total of 3717 women had mastectomies during the 10-year study period; of these women, 142 (3.8%) had breast reconstruction. The reconstruction rate increased to more than 5% in 3 of the last 4 years. Factors affecting the rate of breast reconstruction included patient age, stage of disease and year of mastectomy. Household income did not significantly affect the likelihood of women seeking breast reconstruction.
Conclusion
The rate of breast reconstruction in Nova Scotia (3.8%) is considerably lower than rates reported in the United States (8%–45%). The fact that household income did not influence the breast reconstruction rate may reflect the universal nature of Canada's public health care system.
Abstract
Contexte
On a établi un lien entre la reconstruction du sein après une mastectomie et des bienfaits sociaux, psychologiques et physiques. Les obstacles à la reconstruction du sein aux États-Unis comprennent l'âge, le stade de la maladie, la situation socioéconomique et la région géographique, mais on connaît toutefois peu de choses au sujet des effets de ces facteurs dans le contexte canadien d'un système de santé universel. Nous avons cherché à déterminer le taux de reconstruction du sein en Nouvelle-Écosse, à cerner les caractéristiques qui influencent l'accès à l'intervention et à décrire les taux de différentes options de reconstruction.
Méthodes
Nous avons effectué une étude de cohorte rétrospective portant sur toutes les femmes de la Nouvelle-Écosse chez lesquelles on a diagnostiqué un cancer du sein et qui ont subi une mastectomie entre 1991 et 2001. Nous avons relié les données de 2 bases de données administratives et nous avons effectué des analyses pour chaque année de la période à l'étude. Nous avons suivi les femmes jusqu'à la fin de la période d'étude (2001). Nous avons utilisé une analyse de régression logistique pour évaluer les obstacles possibles à la reconstruction.
Résultats
Au total, 3717 femmes avaient subi une mastectomie au cours des 10 années étudiées et 142 d'entre elles (3,8 %) avaient eu une reconstruction du sein. Le taux de reconstruction a dépassé 5 % au cours de 3 des 4 dernières années. Les facteurs qui ont une incidence sur le taux de reconstruction du sein comprennent l'âge de la patiente, le stade de la maladie et l'année de la mastectomie. Le revenu du ménage n'a pas eu d'effet important sur la probabilité que les femmes cherchent à obtenir une reconstruction du sein.
Conclusion
Le taux de reconstruction du sein en Nouvelle-Écosse (3,8 %) est beaucoup plus faible que les taux signalés aux États-Unis (8 %–45 %). Le fait que le revenu du ménage n'ait pas eu d'incidence sur le taux de reconstruction du sein est peut-être un effet de l'universalité du système public de soins de santé du Canada.
Breast reconstruction after mastectomy is associated with psychological, functional and sexual benefits.1 However, only a small per-centage of women who undergo mastectomy proceed to breast reconstruction.2 It has consistently been shown that postmastectomy reconstruction decreases anxiety about physical appearance and the reoccurrence of cancer, allows greater flexibility in clothing selection and provides a greater sense of wholeness and well-being.3,4 Breast reconstruction with prosthetic implants or flap procedures has been documented to provide good cosmetic results and patient satisfaction.5
Important barriers to accessing reconstructive breast surgery have been identified in the United States. These include older patient age,5–8 advanced stage of disease6,7 and lack of referral to a cancer centre recognized by the National Cancer Institute.8 Low socioeconomic status has also been identified as a barrier,6–8 as 14%–16% of the American nonelderly population have no form of health insurance.9–<11 The Canadian health care system is touted as being free of many of the access barriers that are present in the United States. In Canada, physicians are not constrained in terms of what procedures they can offer and to whom. As such, it would be expected that reconstruction rates in Canada would be higher than in the United States. The rate of postmastectomy breast reconstruction in the United States is 8.3%–45% in population-based studies, and this rate is increasing over time.5–8,12 Conversely, Baxter and colleagues13 examined reconstruction rates in Ontario and found an overall rate of 7.9%, and they found no change in the rate over a 10-year study period. Proximity to a large urban centre where there are institutions with expertise in breast reconstruction was associated with higher rates.13 Aside from geographic location, the reasons for the low rate were not analyzed.
Many breast reconstruction options are available, and they range in complexity from tissue expansion and implant reconstruction to autologous tissue reconstruction with pedicled and free tissue transfer. Implant reconstruction is less costly than autologous tissue reconstruction at the time of initial procedure; however, this option has been found to be less cost-effective over time.14 Autologous tissue reconstruction has been reported to be a more common procedure than implant-based reconstruction, and preference for autologous tissue reconstruction is increasing. In one large study, autologous reconstruction increased from 64% of all reconstructions between 1975 and 1989 to 80% of all reconstructions in the subsequent 10 years.15 Other investigators have found similar results.16,17
We sought to determine rates of breast reconstruction in the province of Nova Scotia over a 10-year period and identify barriers that may influence these rates. In addition, we aimed to identify changing patterns of reconstructive options.
Methods
We conducted a retrospective cohort study involving all women who received diagnoses of breast cancer and had mastectomies in Nova Scotia between 1991 and 2001, inclusive, as recorded in the Nova Scotia Medical Services Insurance (MSI) physician billing database. We then linked the data for this group of women with the Canadian Institute for Health Information (CIHI) database of hospital discharges using a unique patient identifier. We included in our study only those women with codes for mastectomy in both the MSI and CIHI databases. We then followed the cohort until the end of 2001 and used the various codes for breast reconstruction to identify women who underwent reconstruction after mastectomy. The diagnostic labels included “augmentation mammaplasty,” “free myocutaneous flap,” “breast reconstruction with rectus abdominus flap,” “breast reconstruction with flap and prosthesis” and “insertion of breast tissue expander.” We determined the incidence of reconstruction for subgroups stratified according to household income, rural versus urban location, patient age and stage of disease. We estimated household income using neighbourhood-level data from the census based on the postal code of each patient's home. We determined the stage of disease by linking with the vital statistics database; we considered patients who died within 5 years of their mastectomies to have had advanced disease.
We obtained data on the incidence of various reconstructive options using the codes associated with the diagnostic labels previously mentioned. We examined both the type of reconstruction performed and the time between ablative surgery and reconstructive surgery (immediate v. delayed reconstruction). We considered the reconstruction to be immediate when a patient had reconstructive surgery on the same day as ablative surgery. We performed these steps for each year that the cohort was followed.
We accessed all administrative databases through the Population Health Research Unit. We used logistic regression analysis to identify potential barriers to breast reconstruction. We divided the variable “household income” into quartiles and used it as a nominal variable. We performed our analysis using the SAS/STAT (SAS) and Microsoft Excel (Microsoft Corp.) software packages. We determined odds ratios for each of the barriers analyzed using logistic regression.
The Research Ethics Board of the Capital District Health Authority provided ethics approval for this study.
Results
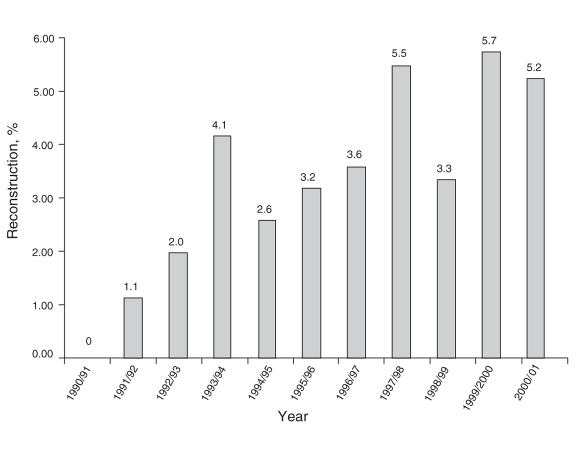
The MSI physician billing database yielded data for 3917 women with codes for mastectomy during our study period. Of these, 3717 (95%) were also in the CIHI hospital discharge database. In this cohort, 142 women underwent breast reconstruction after mastectomy for an overall reconstruction rate of 3.8%. Examining the data on an annual basis, we observed that the rate increased over the study period, reaching a peak of 5.7% for women who had mastectomies in 1999/2000 (Fig. 1). Our logistic regression analysis revealed a statistically significant association between year and rate of mastectomy (p < 0.001).
FIG. 1. Postmastectomy breast reconstruction rate by fiscal year of mastectomy. The rate increased over the study period, p < 0.001.
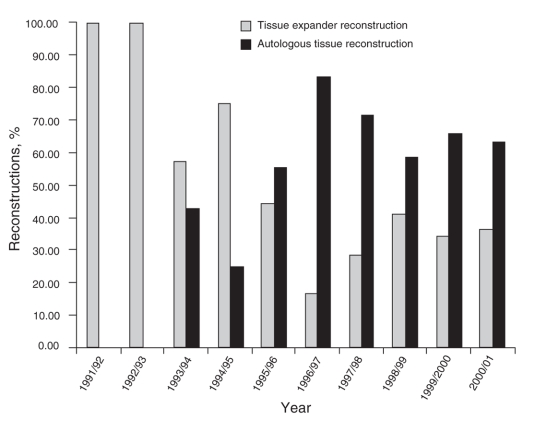
Type of reconstruction
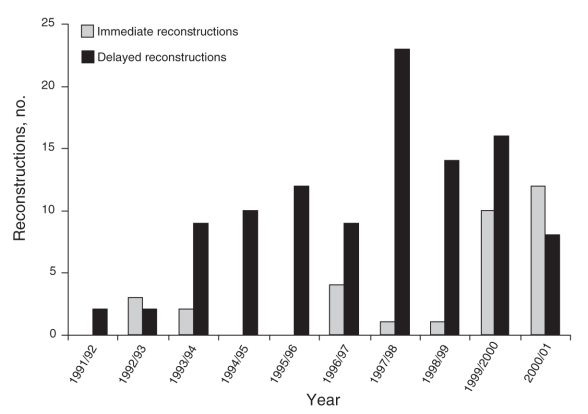
The most common type of breast reconstruction was a tissue expander reconstruction (38%), followed by latissimus flap (25%), free myocutaneous flap (23%) and rectus abdominus flap (14%) reconstructions. The proportion of tissue expander reconstructions decreased over the study period, whereas the proportion of autologous tissue reconstructions increased (Fig. 2). Thirty-three reconstructions (23%) were immediate and 105 (74%) were delayed; data regarding the date of reconstruction were lacking for 4 patients who underwent reconstruction. The number of immediate reconstructions performed each year increased over the study period, with immediate reconstruction surpassing delayed reconstruction in the final year of our study (Fig. 3).
FIG. 2. The proportion of tissue expander reconstructions decreased over the study period, whereas the proportion of autologous tissue reconstructions increased.
FIG. 3. The number of immediate and delayed breast reconstructions by fiscal year of mastectomy.
Barriers to access
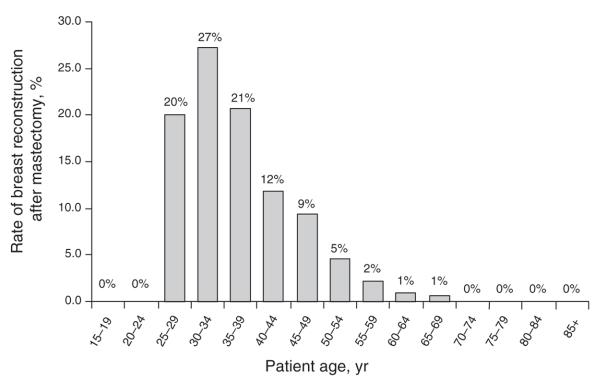
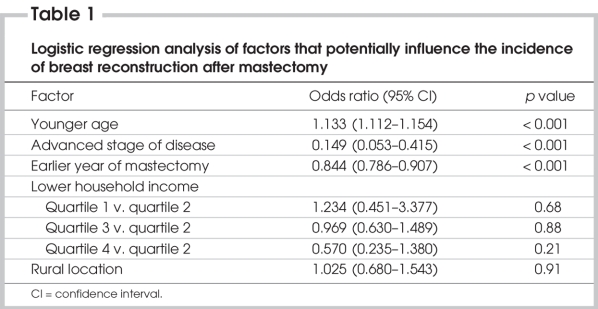
We examined the rate of postmastectomy breast reconstruction within the cohort subgroups. Younger women were more likely to undergo reconstruction than older women (Fig. 4). Women living in urban locations had a higher rate of postmastectomy breast reconstruction (41 reconstructions in 853 patients, 4.8%) than women in rural locations (100 reconstructions in 2693 patients, 3.7%). In our cohort, 649 women (17.5%) died within 5 years of their mastectomies. Of these women, 64% died of causes related to breast cancer. When we examined the rate of reconstruction by 5-year survival, we found that 4.5% of survivors underwent reconstruction, whereas 0.6% of those who did not survive had undergone reconstruction. We performed a logistic regression analysis using patient age, stage of disease (5-yr survival), year of mastectomy, household income and geographic location as variables. Younger patient age (p < 0.001) was associated with higher rates of breast reconstruction, whereas advanced stage of disease (p < 0.001) and earlier year of mastectomy (p < 0.001) were associated with lower rates (Table 1). Household income was not a statistically significant factor in the rate of breast reconstruction.
FIG. 4. The rate of postmastectomy breast reconstruction by patient age.
Table 1
Discussion
Only 3.8% of women in Nova Scotia underwent breast reconstruction after mastectomy between 1991 and 2001, but the proportion of women who have the procedure is increasing over time. In our 10-year study period, there was a trend toward more autologous and immediate reconstructions, whereas the rate of implant-based and delayed reconstructions decreased. This pattern may reflect patient and/or surgeon preference for autologous and immediate breast reconstruction. Despite this trend, implant-based breast reconstruction remained the most common type of reconstruction during our study period.
The reconstruction rate of 3.8% is lower than rates reported in the literature. In a study of 161 mastectomy patients in Illinois who were offered breast reconstruction, 33.5% went on to have the surgery.18 Furthermore, patients treated at a cancer centre recognized by the National Cancer Institute are reported to be 40% more likely to undergo reconstruction after mastectomy than patients treated at other institutions,8 and recognized cancer centres have been found to have a postmastectomy reconstruction rate of 42%.12 Reconstruction rates may be influenced by several factors, including patient desire to undergo the procedure and the failure of surgeons to routinely discuss this option with patients.8 In addition, factors such as stage of disease, geographic location, age and socioeconomic status are important.5–8,13
Our results suggest that women with advanced stage of disease have lower rates of reconstruction. This is likely because of decreased referral rates for this patient group, poor medical condition or death precluding reconstruction. An association between advanced stage of breast cancer and a lower rate of breast reconstruction has been reported in other studies.6–8 Although the literature does not support advanced disease as being a contraindication to breast reconstruction, women and/or their physicians may not perceive the procedure as a high priority. However, women who do undergo reconstruction report substantial improvements in quality of life during their remaining time.19–21
We found that patient age influenced the rate of breast reconstruction in Nova Scotia. Younger women either request reconstruction more often or are more likely than their older counterparts to be offered a referral by their general surgeon. Older women may have comorbidities that preclude additional surgery. These findings are consistent with previous studies in the United States.5–8 However, advanced patient age is not considered to be a contraindication to reconstructive surgery.22 Rates of referral, therefore, should be comparable among all age groups. Recent studies have shown that women adjust well to mastectomies, regardless of whether they undergo reconstruction, as long as they are given the choice.23,24 The fact that the plastic surgery literature does not support patient age nor stage of disease as contraindications to breast reconstruction20–22 highlights the need for all patients to be given the option of reconstruction after mastectomy.
The rate of reconstruction was not significantly different between patients in rural and urban areas, suggesting that women in Nova Scotia have equal access to this service regardless of their geographic locations. We found that household income was not a significant barrier to reconstructive surgery, which contradicts data from American studies that consistently find household income to influence the rate of breast reconstruction after mastectomy.6–8 In Canada, household income is effectively eliminated as an access barrier to breast reconstruction owing to our universal health care system.
To our knowledge, ours is the first study to evaluate potential barriers to breast reconstruction after mastectomy in Canada. Because population-based cohorts are inclusive of the entire population, our findings are generalizable and have a high degree of external validity.
We acknowledge several limitations to our study. We obtained the data for the cohort through administrative databases that were not specifically designed for our study. Consequently, we required proxies for certain variables of interest, including stage of disease and household income. We evaluated the effect of stage of disease on the rate of breast reconstruction by comparing the rate of reconstruction for women who survived 5 years after their mastectomy with that of women who did not. Although the use of postal codes to estimate household income is a common method of estimating socioeconomic status, the method has been found to have a lower correlation with socioeconomic status than other methods.13 However, Deonandan and colleagues25 suggested that postal code estimations can be used to evaluate the impact of socioeconomic status on access to specialized medical procedures. Given that reconstruction after mastectomy became more common in Nova Scotia as our study progressed, applying our methodology at a later date would likely have yielded a larger sample size.
Conclusion
We have found that the rate of breast reconstruction after mastectomy over a 10-year period in Nova Scotia is only 3.8%, but that the proportion of women who undergo reconstruction is increasing over time. This rate is far lower than those reported in the United States (8%–45%). Older patient age and advanced stage of disease negatively influenced rates of reconstruction in our population-based study. Geographic location and household income do not appear to be access barriers in Nova Scotia. The lack of influence of household income on breast reconstruction rates underscores the central value of universal access to health care in Canada. Our study emphasizes the need for universal access to reconstructive surgery consultation regardless of age, disease stage and socioeconomic status.
Acknowledgments
We thank the Population Health Research Unit at Dalhousie University for their help with this study. This study was funded by a grant from the Capital District Health Authority Research Fund, Nova Scotia.
Contributors: All authors designed the study, analyzed the data, reviewed the article and approved its publication. Drs. Barnsley and Sigurdson wrote the article.
Competing interests: None declared.
Accepted for publication Jul. 25, 2007
Correspondence to: Dr. L. Sigurdson, New Halifax Infirmary, 4437-1796 Summer St., Halifax NS B3H 3A7; leif.sigurdson@dal.ca
References
- 1.Schain WS. Reasons why mastectomy patients do not have breast reconstruction [discussion]. Plast Reconstr Surg 1990; 86:1123-5. [PubMed]
- 2.Handel N, Silverstein MJ, Waisman E, et al. Reasons why mastectomy patients do not have breast reconstruction. Plast Reconstr Surg 1990;86:1118-22. [PubMed]
- 3.Schain WS, Jacobs E, Wellisch DK. Psychosocial issues in breast reconstruction. Intrapsychic, interpersonal, and practical concerns. Clin Plast Surg 1984;11:237-51. [PubMed]
- 4.Schain WS, Wellisch DK, Pasnau RO, et al. The sooner the better: a study of psychological factors in women undergoing immediate versus delayed breast reconstruction. Am J Psychiatry 1985;142:40-6. [DOI] [PubMed]
- 5.Desch CE, Penberthy LT, Hillner BE, et al. A sociodemographic and economic comparison of breast reconstruction, mastectomy, and conservative surgery. Surgery 1999; 125:441-7. [PubMed]
- 6.Polednak AP. Postmastectomy breast reconstruction in Connecticut: trends and predictors. Plast Reconstr Surg 1999; 104:669-73. [DOI] [PubMed]
- 7.Polednak AP. How frequent is postmastectomy breast reconstructive surgery? A study linking two statewide databases. Plast Reconstr Surg 2001;108:73-7. [DOI] [PubMed]
- 8.Morrow M, Scott SK, Menck HR, et al. Factors influencing the use of breast reconstruction postmastectomy: a National Cancer Database study. J Am Coll Surg 2001; 192:1-8. [DOI] [PubMed]
- 9.Fuchs VR, Hahn JS. How does Canada do it? A comparison of expenditures for physicians' services in the United States and Canada. N Engl J Med 1990;323: 884-90. [DOI] [PubMed]
- 10.Fronstin P. Trends in health insurance coverage. EBRI Issue Brief 1997;(185):1-18. [PubMed]
- 11.Fronstin P. Sources of health insurance and characteristics of the uninsured: analysis of the March 2001 Current Population Survey. EBRI Issue Brief 2001;(240):1-31. [PubMed]
- 12.Christian CK, Edge S, Niland J, et al. A multi-institutional analysis of the socioeconomic determinants of breast reconstruction. Ann Surg 2006;243;241-9. [DOI] [PMC free article] [PubMed]
- 13.Baxter N, Goel V, Semple JL. Utiliza-tion and regional variation of breast reconstruction in Canada. Plast Reconstr Surg 2005; 115:338-9. [PubMed]
- 14.Kroll SS, Evans GR, Reece GP, et al. Comparison of resource costs between implant-based and TRAM flap breast reconstruction. Plast Reconstr Surg 1996; 97: 364-72. [DOI] [PubMed]
- 15.Losken A, Carlson GW, Bostwick J III, et al. Trends in unilateral breast reconstruction and management of the contralateral breast: the Emory experience. Plast Reconstr Surg 2002;110:89-97. [DOI] [PubMed]
- 16.Trabulsy PP, Anthony JP, Mathes SJ. Changing trends in postmastectomy breast reconstruction: a 13-year experience. Plast Reconstr Surg 1994;93:1418-27. [DOI] [PubMed]
- 17.Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002; 109: 2265-74. [DOI] [PubMed]
- 18.Morrow M, Bucci C, Rademaker A. Medical contraindications are not a major factor in the underutilization of breast conserving therapy. J Am Coll Surg 1998; 186: 269-74. [DOI] [PubMed]
- 19.Behnam AB, Nguyen D, Moran SL, et al. TRAM flap breast reconstruction for patients with advanced breast disease. Ann Plast Surg 2003;50:567-71. [DOI] [PubMed]
- 20.Foster RD, Esserman LJ, Anthony JP, et al. Skin-sparing mastectomy and immediate breast reconstruction: a prospective cohort study for the treatment of advanced stages of breast carcinoma. Ann Surg Oncol 2002;9:462-6. [DOI] [PubMed]
- 21.Newman LA, Kuerer HM, Hunt KK, et al. Feasibility of immediate breast reconstruction for locally advanced breast cancer. Ann Surg Oncol 1999;6:671-5. [DOI] [PubMed]
- 22.Lin KY, Johns FR, Gibson J, et al. An outcome study of breast reconstruction: presurgical identification of risk factors for complications. Ann Surg Oncol 2001;8:586-91. [DOI] [PubMed]
- 23.Baker C, Johnson N, Nelson J, et al. Perspective on reconstruction after mastectomy. Am J Surg 2002;183:562-5. [DOI] [PubMed]
- 24.Harcourt DM, Rumsey NJ, Ambler NR, et al. The psychological effect of mastectomy with or without breast reconstruction: a prospective, multicenter study. Plast Reconstr Surg 2003;111:1060-8. [DOI] [PubMed]
- 25.Deonandan R, Campbell K, Ostbye T, et al. A comparison of methods for measuring socio-economic status by occupation or postal area. Chronic Dis Can 2000; 21: 114-8. [PubMed]