Internal abdominal hernias are rare conditions, accounting for 0.9% of all intestinal obstructions.1 Paraduodenal hernias constitute half of all internal abdominal hernias. They occur when the small bowel herniates into the paraduodenal fossa and can manifest as intestinal obstruction.2 Herniation into the left paraduodenal fossa (fossa of Landzert) occurs more frequently than herniation into the right fossa (fossa of Kolb).3 Clinical diagnosis is difficult. We report the case of a left paraduodenal hernia as a coincidental finding in a patient who underwent a laparotomy for a suspected sigmoid tumour.
Case report
A 59-year-old man presented with a 1-year history of intermittent rectal bleeding, lethargy, tiredness and occasional sharp generalized abdominal pain. The pain was not associated with nausea, vomiting or weight loss. Clinical examination and blood investigations were unremarkable. Barium enema demonstrated colonic diverticulosis and a polypoid lesion in the middle of the sigmoid colon. Colonoscopy failed to reveal the lesion, but repeat barium enema demonstrated a polypoid filling defect in the sigmoid colon.
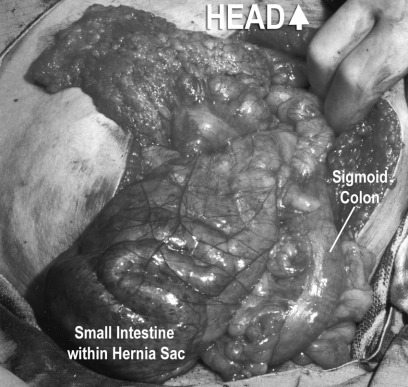
A sigmoid malignant tumour was suspected, and the patient underwent a laparotomy, which revealed that almost the entire small bowel was held within a separate peritoneal sac (Fig. 1). The left colon appeared normal during the on-table sigmoidoscopy. The terminal ileum appeared to emerge from beneath a peritoneal fold, and possibly contained the inferior mesenteric vein. The peritoneal sac was opened to reveal small bowel, partially obstructed by the inferior mesenteric vein, crossing the terminal ileum (Fig. 2). The entire small bowel was reduced from beneath the vascular fold.
FIG. 1. Initial appearance at laparotomy: the small bowel is within the peritoneal sac at the mesentery of the descending colon.
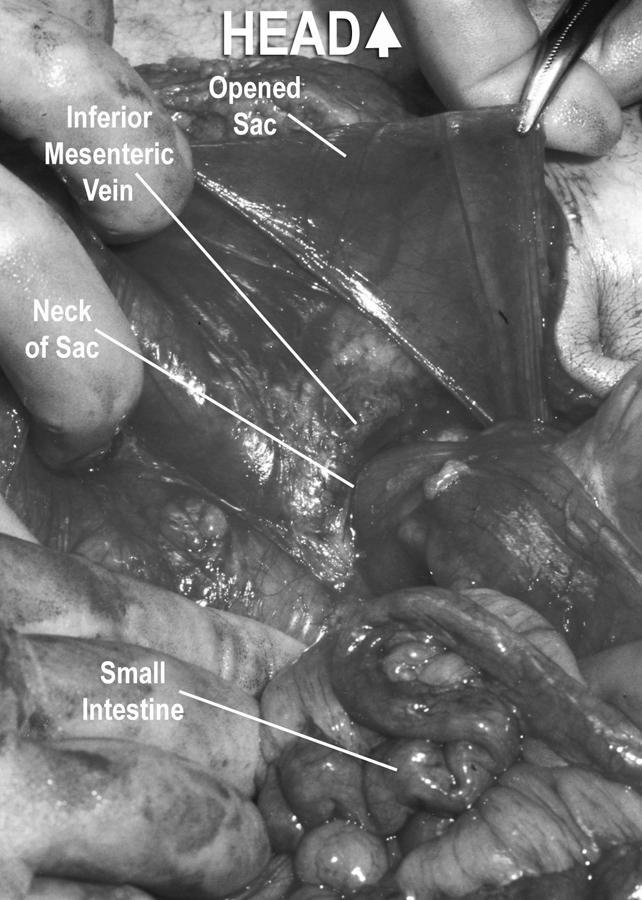
FIG. 2. View from inside the sac, showing the relationship of the inferior mesenteric vein to the neck of the sac.
These findings were consistent with a large hernia of the left paraduodenal fossa, extending behind the inferior mesenteric vein to enclose the entire small bowel. The defect between the inferior mesenteric vein and posterior abdominal wall was closed with a continuous absorbable suture, and the peritoneal sac was excised and plicated. The patient made a smooth recovery. He was asymptomatic at follow-up 12 months postoperatively.
Discussion
An internal hernia is defined as a hernia formed by the protrusion of a viscus through a peritoneal or mesenteric aperture, leading to its encapsulation within a compartment of the abdominal cavity.1,3 Internal hernias account for 0.2%–0.9% of intestinal obstructions.4 Between 10% and 50% of internal hernias are discovered during unrelated abdominal surgeries or at autopsy.2,3 Based on an analysis of 467 cases, Hansmann and Morton5 classified the internal hernias into the following 7 groups, based on location: paraduodenal, foramen of Winslow, pericecal, intersigmoid, transmesenteric, transomental and retroanastomotic. Liew and associates3 listed at least 25 different anatomic sites of internal hernias.
Paraduodenal hernias are very rare, but they account for about 30%–53% of all internal hernias.1 They occur 3 times more commonly in the left paraduodenal fossa than in the right, are more common in men3,4 and are mostly congenital.
The majority of presentations occur between the 4th and 5th decades of life.1,3 Internal hernias can be asymptomatic, present as an acute intestinal obstruction or as chronic intermittent abdominal pain, especially after a large meal.1,2 Findings on physical examination may be normal, unless the hernia produces a mass or causes intestinal obstruction.1,3
Preoperative diagnosis is difficult.3 Plain abdominal radiography may demonstrate a distended, fluid-filled stomach or reveal dilated loops of small bowel in an ovoid mass lateral from the midline.2 Barium-contrast studies may reveal encapsulation of the small bowel within the left upper quadrant.1 Ultrasonography may demonstrate an abdominal mass or internal tubular cysts that change shape over time and after ingestion of fluid.1–3 Computed tomography may reveal a cluster of small-bowel loops, mainly at the level of the ligament of Treitz or behind the pancreas.1–3 Celiac arteriography can demonstrate a displaced spleen.3 Superior mesenteric arteriography can reveal jejunal arteries displaced upward and to the left.
After diagnosis, treatment should be prompt.2 Obstruction of the entrapped bowel can lead to ischemia and perforation with a high mortality.4 Exploratory laparotomy is mandatory.3 The steps of operation include adequate incision, reduction of the hernia content and repair of the defect.1 Removal of the sac remains controversial as it is part of the mesocolon and may lead to colonic vascular impairment.1 In our case, the hernia was reduced and its neck closed with continuous absorbable sutures to the posterior abdominal wall. The sac was excised and plicated.
Conclusion
Paraduodenal hernias are extremely rare and difficult to diagnose. Acute awareness is required, since without prompt surgical treatment the mortality can be high. Radiologic investigations are helpful but should not delay definitive treatment in an unwell patient.
Competing interests: None declared.
Accepted for publication Jan. 16, 2008
Correspondence to: Mr. R. Singhal, 26 Lloyd Square, 16 Niall Close, Edgbaston, Birmingham, B15 3LX, United Kingdom; singhal_rishi@rediffmail.com
References
- 1.Khan MA, Lo AY, Vande Maele DM. Paraduodenal hernia. Am Surg 1998; 64:1218-22. [PubMed]
- 2.Hirasaki S, Koide N, Shima Y, et al. Unusual variant of left paraduodenal hernia herniated into the mesocolic fossa leading to jejunal strangulation. J Gastroenterol 1998;33:734-8. [DOI] [PubMed]
- 3.Liew KL, Choong CS, Shiau GF, et al. Descending mesocolon defect herniation: case report. Changgeng Yi Xue Za Zhi 1999;22:133-7. [PubMed]
- 4.Manji R, Warnock GL. Left paraduodenal hernia: an unusual cause of small-bowel obstruction. Can J Surg 2001;44:455-7. [PMC free article] [PubMed]
- 5.Hansmann GH, Morton SA. Intra-abdominal hernia: report of a case and review of the literature. Arch Surg 1939; 3:973-86.