Abstract
Leishmania species are obligate intracellular pathogens of mononuclear phagocytes. Successful infection depends on sequestration of the promastigote (insect form) within host cells, allowing transformation into the relatively hardy amastigote stage. Promastigotes are killed readily by circulating phagocytes and nonimmune serum, suggesting that cutaneous infection is initiated within a permissive cell in the epidermis or dermis. From large sections of primate skin dermal macrophages and epidermal Langerhans cells were isolated, and their interaction with promastigotes of Leishmania major was investigated in vitro. Dermal macrophages were readily infected with promastigotes, and successful transformation to and replication of amastigotes was observed. Ingestion of promastigotes by dermal macrophages was not associated with a significant respiratory burst, in contrast to that by other macrophage populations, and was associated with significantly greater survival of parasites. Stimulation of these cells with phorbol myristate acetate or opsonized zymosan revealed that those cells were generally oxidatively deficient. Langerhans cells could not be successfully infected by promastigotes under similar conditions. Examination of these cells for expression of CR3, which has been identified as a potential Leishmania receptor, revealed that Langerhans cells did not express the alpha M subunit of CR3, whereas dermal macrophages were CR3 positive. These data support the concept that dermal macrophages are the site of initiation of Leishmania infection.
Full text
PDF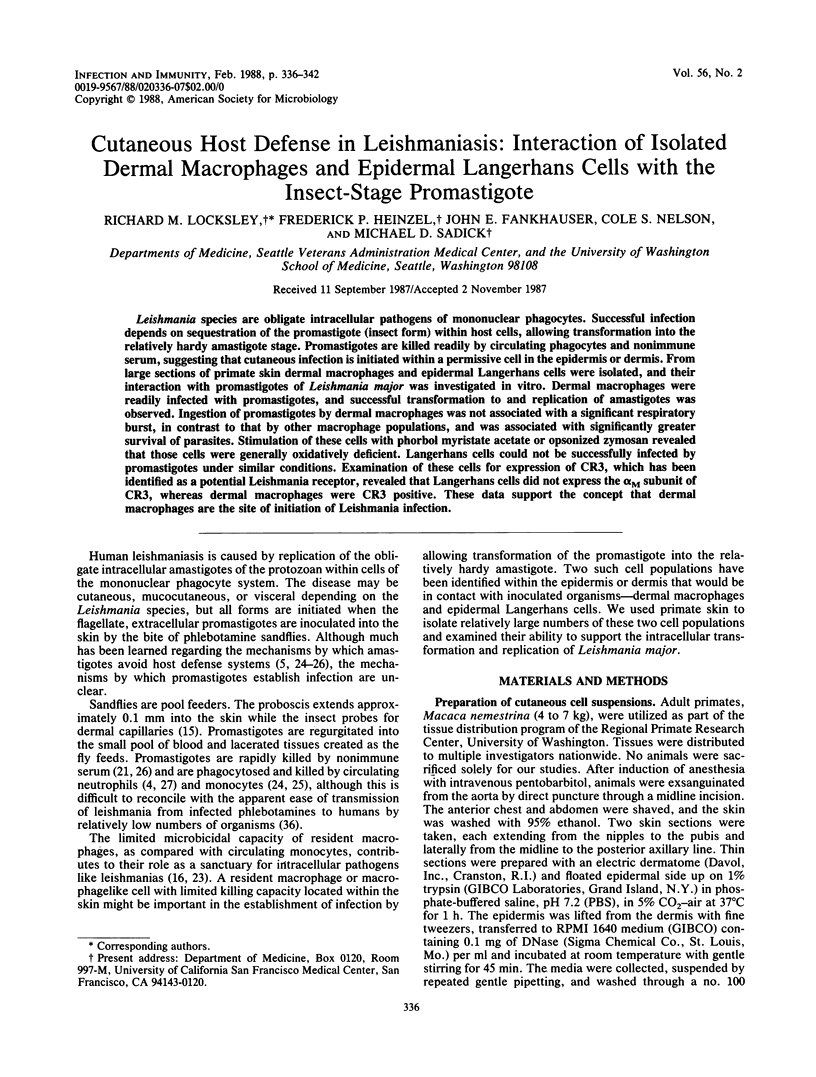



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beckstead J. H., Wood G. S., Turner R. R. Histiocytosis X cells and Langerhans cells: enzyme histochemical and immunologic similarities. Hum Pathol. 1984 Sep;15(9):826–833. doi: 10.1016/s0046-8177(84)80143-4. [DOI] [PubMed] [Google Scholar]
- Blackwell J. M., Ezekowitz R. A., Roberts M. B., Channon J. Y., Sim R. B., Gordon S. Macrophage complement and lectin-like receptors bind Leishmania in the absence of serum. J Exp Med. 1985 Jul 1;162(1):324–331. doi: 10.1084/jem.162.1.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braathen L. R., Thorsby E. Human epidermal Langerhans cells are more potent than blood monocytes in inducing some antigen-specific T-cell responses. Br J Dermatol. 1983 Feb;108(2):139–146. doi: 10.1111/j.1365-2133.1983.tb00055.x. [DOI] [PubMed] [Google Scholar]
- Chang K. P. Leishmanicidal mechanisms of human polymorphonuclear phagocytes. Am J Trop Med Hyg. 1981 Mar;30(2):322–333. doi: 10.4269/ajtmh.1981.30.322. [DOI] [PubMed] [Google Scholar]
- Channon J. Y., Roberts M. B., Blackwell J. M. A study of the differential respiratory burst activity elicited by promastigotes and amastigotes of Leishmania donovani in murine resident peritoneal macrophages. Immunology. 1984 Oct;53(2):345–355. [PMC free article] [PubMed] [Google Scholar]
- Fithian E., Kung P., Goldstein G., Rubenfeld M., Fenoglio C., Edelson R. Reactivity of Langerhans cells with hybridoma antibody. Proc Natl Acad Sci U S A. 1981 Apr;78(4):2541–2544. doi: 10.1073/pnas.78.4.2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin W. A., Mason D. Y., Pulford K., Falini B., Bliss E., Gatter K. C., Stein H., Clarke L. C., McGee J. O. Immunohistological analysis of human mononuclear phagocytes and dendritic cells by using monoclonal antibodies. Lab Invest. 1986 Mar;54(3):322–335. [PubMed] [Google Scholar]
- Haines K. A., Flotte T. J., Springer T. A., Gigli I., Thorbecke G. J. Staining of Langerhans cells with monoclonal antibodies to macrophages and lymphoid cells. Proc Natl Acad Sci U S A. 1983 Jun;80(11):3448–3451. doi: 10.1073/pnas.80.11.3448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickstein D. D., Smith A., Fisher W., Beatty P. G., Schwartz B. R., Harlan J. M., Root R. K., Locksley R. M. Expression of leukocyte adherence-related glycoproteins during differentiation of HL-60 promyelocytic leukemia cells. J Immunol. 1987 Jan 15;138(2):513–519. [PubMed] [Google Scholar]
- Hsu S. M., Raine L., Fanger H. The use of antiavidin antibody and avidin-biotin-peroxidase complex in immunoperoxidase technics. Am J Clin Pathol. 1981 Jun;75(6):816–821. doi: 10.1093/ajcp/75.6.816. [DOI] [PubMed] [Google Scholar]
- Inaba K., Schuler G., Witmer M. D., Valinksy J., Atassi B., Steinman R. M. Immunologic properties of purified epidermal Langerhans cells. Distinct requirements for stimulation of unprimed and sensitized T lymphocytes. J Exp Med. 1986 Aug 1;164(2):605–613. doi: 10.1084/jem.164.2.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juhlin L., Shelley W. B. New staining techniques for the Langerhans cell. Acta Derm Venereol. 1977;57(4):289–296. [PubMed] [Google Scholar]
- KAPLOW L. S. SIMPLIFIED MYELOPEROXIDASE STAIN USING BENZIDINE DIHYDROCHLORIDE. Blood. 1965 Aug;26:215–219. [PubMed] [Google Scholar]
- Lepay D. A., Nathan C. F., Steinman R. M., Murray H. W., Cohn Z. A. Murine Kupffer cells. Mononuclear phagocytes deficient in the generation of reactive oxygen intermediates. J Exp Med. 1985 May 1;161(5):1079–1096. doi: 10.1084/jem.161.5.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locksley R. M., Klebanoff S. J. Oxygen-dependent microbicidal systems of phagocytes and host defense against intracellular protozoa. J Cell Biochem. 1983;22(3):173–185. doi: 10.1002/jcb.240220306. [DOI] [PubMed] [Google Scholar]
- Locksley R. M., Wilson C. B., Klebanoff S. J. Role for endogenous and acquired peroxidase in the toxoplasmacidal activity of murine and human mononuclear phagocytes. J Clin Invest. 1982 May;69(5):1099–1111. doi: 10.1172/JCI110545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauel J., Behin R., Biroum-Noerjasin Quantitative release of live microorganisms from infected macrophages by sodium dodecyl sulphate. Nat New Biol. 1973 Jul 18;244(133):93–94. doi: 10.1038/newbio244093a0. [DOI] [PubMed] [Google Scholar]
- Mittag H., Klingmüller G. Langerhans cells in granulomatous syphilis. Arch Dermatol Res. 1983;275(3):190–196. doi: 10.1007/BF00510051. [DOI] [PubMed] [Google Scholar]
- Mosser D. M., Edelson P. J. Activation of the alternative complement pathway by Leishmania promastigotes: parasite lysis and attachment to macrophages. J Immunol. 1984 Mar;132(3):1501–1505. [PubMed] [Google Scholar]
- Mosser D. M., Edelson P. J. The mouse macrophage receptor for C3bi (CR3) is a major mechanism in the phagocytosis of Leishmania promastigotes. J Immunol. 1985 Oct;135(4):2785–2789. [PubMed] [Google Scholar]
- Murray H. W., Cartelli D. M. Killing of intracellular Leishmania donovani by human mononuclear phagocytes. Evidence for oxygen-dependent and -independent leishmanicidal activity. J Clin Invest. 1983 Jul;72(1):32–44. doi: 10.1172/JCI110972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray H. W. Cell-mediated immune response in experimental visceral leishmaniasis. II. Oxygen-dependent killing of intracellular Leishmania donovani amastigotes. J Immunol. 1982 Jul;129(1):351–357. [PubMed] [Google Scholar]
- Pearson R. D., Steigbigel R. T. Mechanism of lethal effect of human serum upon Leishmania donovani. J Immunol. 1980 Nov;125(5):2195–2201. [PubMed] [Google Scholar]
- Pearson R. D., Steigbigel R. T. Phagocytosis and killing of the protozoan Leishmania donovani by human polymorphonuclear leukocytes. J Immunol. 1981 Oct;127(4):1438–1443. [PubMed] [Google Scholar]
- Poulter L. W., Collings L. A., Tung K. S., Waters M. F. Parasitism of antigen presenting cells in hyperbacillary leprosy. Clin Exp Immunol. 1984 Mar;55(3):611–617. [PMC free article] [PubMed] [Google Scholar]
- Sadick M. D., Locksley R. M., Tubbs C., Raff H. V. Murine cutaneous leishmaniasis: resistance correlates with the capacity to generate interferon-gamma in response to Leishmania antigens in vitro. J Immunol. 1986 Jan;136(2):655–661. [PubMed] [Google Scholar]
- Sanchez-Madrid F., Nagy J. A., Robbins E., Simon P., Springer T. A. A human leukocyte differentiation antigen family with distinct alpha-subunits and a common beta-subunit: the lymphocyte function-associated antigen (LFA-1), the C3bi complement receptor (OKM1/Mac-1), and the p150,95 molecule. J Exp Med. 1983 Dec 1;158(6):1785–1803. doi: 10.1084/jem.158.6.1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauder D. N., Dinarello C. A., Morhenn V. B. Langerhans cell production of interleukin-1. J Invest Dermatol. 1984 Jun;82(6):605–607. doi: 10.1111/1523-1747.ep12261439. [DOI] [PubMed] [Google Scholar]
- Schuler G., Steinman R. M. Murine epidermal Langerhans cells mature into potent immunostimulatory dendritic cells in vitro. J Exp Med. 1985 Mar 1;161(3):526–546. doi: 10.1084/jem.161.3.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelley W. B., Juhlin L. Langerhans cells form a reticuloepithelial trap for external contact antigens. Nature. 1976 May 6;261(5555):46–47. doi: 10.1038/261046a0. [DOI] [PubMed] [Google Scholar]
- Silberberg-Sinakin I., Gigli I., Baer R. L., Thorbecke G. J. Langerhans cells: role in contact hypersensitivity and relationship to lymphoid dendritic cells and to macrophages. Immunol Rev. 1980;53:203–232. doi: 10.1111/j.1600-065x.1980.tb01045.x. [DOI] [PubMed] [Google Scholar]
- Silberberg-Sinakin I., Thorbecke G. J., Baer R. L., Rosenthal S. A., Berezowsky V. Antigen-bearing langerhans cells in skin, dermal lymphatics and in lymph nodes. Cell Immunol. 1976 Aug;25(2):137–151. doi: 10.1016/0008-8749(76)90105-2. [DOI] [PubMed] [Google Scholar]
- Van Voorhis W. C., Kaplan G., Sarno E. N., Horwitz M. A., Steinman R. M., Levis W. R., Nogueira N., Hair L. S., Gattass C. R., Arrick B. A. The cutaneous infiltrates of leprosy: cellular characteristics and the predominant T-cell phenotypes. N Engl J Med. 1982 Dec 23;307(26):1593–1597. doi: 10.1056/NEJM198212233072601. [DOI] [PubMed] [Google Scholar]
- Wilson C. B., Tsai V., Remington J. S. Failure to trigger the oxidative metabolic burst by normal macrophages: possible mechanism for survival of intracellular pathogens. J Exp Med. 1980 Feb 1;151(2):328–346. doi: 10.1084/jem.151.2.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyler D. J., Suzuki K. In vitro parasite-monocyte interactions in human leishmaniasis: effect of enzyme treatments on attachment. Infect Immun. 1983 Oct;42(1):356–361. doi: 10.1128/iai.42.1.356-361.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki L. J., Sato V. L. "Panning" for lymphocytes: a method for cell selection. Proc Natl Acad Sci U S A. 1978 Jun;75(6):2844–2848. doi: 10.1073/pnas.75.6.2844. [DOI] [PMC free article] [PubMed] [Google Scholar]