Abstract
Objective
To evaluate the psychosocial and behavioural impact of the first ever national level comprehensive workplace smoke‐free law, implemented in Ireland in March 2004.
Design
Quasi‐experimental prospective cohort survey: parallel cohort telephone surveys of national representative samples of adult smokers in Ireland (n = 769) and the UK (n = 416), surveyed before the law (December 2003 to January 2004) and 8–9 months after the law (December 2004 to January 2005).
Main outcome measures
Respondents' reports of smoking in key public venues, support for total bans in those key venues, and behavioural changes due to the law.
Results
The Irish law led to dramatic declines in reported smoking in all venues, including workplaces (62% to 14%), restaurants (85% to 3%), and bars/pubs (98% to 5%). Support for total bans among Irish smokers increased in all venues, including workplaces (43% to 67%), restaurants (45% to 77%), and bars/pubs (13% to 46%). Overall, 83% of Irish smokers reported that the smoke‐free law was a “good” or “very good” thing. The proportion of Irish homes with smoking bans also increased. Approximately 46% of Irish smokers reported that the law had made them more likely to quit. Among Irish smokers who had quit at post‐legislation, 80% reported that the law had helped them quit and 88% reported that the law helped them stay quit.
Conclusion
The Ireland smoke‐free law stands as a positive example of how a population‐level policy intervention can achieve its public health goals while achieving a high level of acceptance among smokers. These findings support initiatives in many countries toward implementing smoke‐free legislation, particularly those who have ratified the Framework Convention on Tobacco Control, which calls for legislation to reduce tobacco smoke pollution.
Keywords: Framework Convention on Tobacco Control, FCTC, tobacco smoke pollution, environmental tobacco smoke, secondhand smoke, smoke‐free laws, tobacco control policy, policy evaluation
Tobacco smoke pollution (TSP) has been causally linked to adverse health effects, including lung cancer, heart disease, asthma in children, and sudden infant death syndrome.1,2 Workplace smoke‐free policies are an effective means of reducing exposure to TSP and its public health burden.3,4,5,6,7 The respiratory health of workers has also been shown to improve following a workplace smoking law.8 There also exists evidence that smoke‐free policies increase cessation and decrease consumption among continuing smokers.3,4,5,6,7,8,9,10
Most studies of smoke‐free policies have focused on individual workplaces.3,4,5,6 However, as community‐ and state/province‐wide smoke‐free laws have been implemented, studies have demonstrated their positive impact on reducing TSP exposure.11,12,13 Moreover, these benefits have been realised without the negative economic consequences that have been predicted by opponents of smoke‐free laws.14
One important barrier to implementing smoke‐free laws is the perception among policymakers of low support among smokers. Indeed, support among smokers for comprehensive bans, particularly in bars, tends to be low.15 However, studies show that support for smoke‐free policies increases after their implementation in workplaces4,16,17,18,19,20 and in restaurants.15
The Framework Convention on Tobacco Control (FCTC), the first‐ever treaty devoted to public health, calls for legislation to reduce or eliminate TSP. Currently, over 120 countries have ratified the FCTC and are thus obligated to implement some form of smoke‐free legislation. There is thus an urgent need to rigorously evaluate the effects of national‐level smoke‐free legislation.
On 29 March 2004, the Republic of Ireland became the first country in the world to implement comprehensive smoke‐free legislation in all workplaces, including restaurants and pubs, with no allowance for designated smoking rooms, and few exemptions. As of 1 May 2006, a number of jurisdictions have implemented or passed legislation to implement similarly strict, 100% smoke‐free laws (for example, four other countries: Norway, New Zealand, Bhutan, and Uruguay; 14 US states (including the District of Columbia); nine Canadian provinces and territories; seven Australian states and territories; as well as Scotland).21
We took advantage of this natural experiment to conduct the first prospective cohort study of a national comprehensive smoke‐free workplace law, in the Republic of Ireland. Because most of the potentially controversial effects of such policies relate to their impact on smokers, our study focuses on smokers. The objective of the present study was to measure, among a nationally representative sample of adult Irish smokers, the effects of the Irish law on: (1) reported smoking in key venues (for example, restaurants, pubs); (2) support for smoke‐free venues and the Irish law; and (3) self reported effects of the law on consumption and quitting. This prospective study followed a quasi‐experimental design, with the inclusion of a nationally representative sample of adult smokers in the UK.
METHODS
Sample
Participants were 1679 adult smokers (⩾ 18 years old) from Ireland (n = 1071; 70.9% cooperation rate) and the United Kingdom (n = 608; 70.3% cooperation rate) of which 1185 respondents completed the follow up survey (Ireland = 769; UK = 416; overall follow up rate = 70.6%). Completers and non‐completers did not differ on baseline measures of cigarettes per day, intentions to quit, income, or sex; however, non‐completers were younger (M = 36.0 years) than completers (M = 41.7 years), t = 7.31, p < 0.001 and less likely to be white, χ2 = 8.02, p = 0.005. Table 1 presents the unweighted and weighted sample characteristics for respondents at baseline who also completed the follow up survey.
Table 1 Baseline characteristics (weighted and unweighted) of the study cohort in Ireland (n = 769) and in the UK (n = 416).
| Characteristic | Unweighted | Weighted | |||
|---|---|---|---|---|---|
| Ireland | UK | Ireland | UK | p Value | |
| Sex | 0.663 | ||||
| Female | 58.3 | 55.5 | 48.7 | 50.0 | |
| Male | 41.7 | 44.5 | 51.3 | 50.0 | |
| Age (years) | 0.001 | ||||
| 18–24 | 10.5 | 5.3 | 20.9 | 13.7 | |
| 25–39 | 26.1 | 38.2 | 34.3 | 38.3 | |
| 40–54 | 39.3 | 30.5 | 26.9 | 23.6 | |
| 55+ | 24.1 | 26.0 | 17.8 | 24.4 | |
| Education | 0.304 | ||||
| 12 years or less | 69.2 | 59.1 | 63.6 | 60.5 | |
| More than 12 years | 30.8 | 40.9 | 36.4 | 39.5 | |
| Ethnicity | 0.484 | ||||
| White | 94.4 | 96.4 | 95.1 | 96.0 | |
| Other/mixed | 5.6 | 3.6 | 4.9 | 4.0 | |
| Average cigarettes per day (SD) | 17.9 (10.3) | 17.9 (11.3) | 17.6 (10.5) | 18.0 (11.7) | 0.530 |
| Quit attempt(s) in past year | 0.008 | ||||
| No attempt in past year | 55.6 | 60.6 | 51.1 | 59.2 | |
| At least one attempt in past year | 44.4 | 39.4 | 48.9 | 40.8 | |
Procedure
Respondents were recruited using probability sampling methods with telephone numbers selected at random from the population of each country, within strata defined by geographic region and community size. List assisted telephone numbers were obtained from Survey Sampling International. Eligible households were identified by asking a household informant to provide the number of adult smokers. The next birthday method22 was used to select the respondent in households with more than one eligible adult smoker.
The baseline, pre‐legislation survey was conducted from December 2003 to January 2004, using computer assisted telephone interviewing (CATI) software. The survey fieldwork was conducted by Roy Morgan Research, Melbourne, Australia. Respondents were re‐contacted from December 2004 to January 2005, for the post‐legislation survey. Each survey took an average of 40 minutes to complete. Participants were mailed compensation equivalent to £7 (UK) or €10 (Ireland) following each survey. The study protocol was standardised across the two countries, and was reviewed and cleared by the Research Ethics Board of the University of Waterloo.
Measures
The ITC Ireland/UK Survey was adapted from the International Tobacco Control (ITC) Four Country Survey (ITC‐4), a cohort telephone survey of over 2000 adult smokers in each of four countries—Canada, USA, UK, and Australia.15,23 All questions were asked at both survey waves unless otherwise indicated.
Demographics
Level of education was categorised into: 12 years or less, versus more than 12 years of education. Annual income was categorised into: “€15 000 or under”, “€15 001–€30 000”, and “€30 001 and over” in Ireland (£ in the UK). Respondent ethnicity was obtained using each country's census question and then dichotomised (“white” v “non‐white and mixed race”). These were asked only at pre‐legislation.
Smoking behaviour
Respondents reported the mean number of cigarettes smoked per day. Responses were then categorised into 1–10, 11–20, 21–30, and > 30. Respondents reported time after waking before the first cigarette of the day.24 Responses were then categorised into > 60 minutes, 31–60 minutes, 6–30 minutes, and ⩽ 5 minutes, in order of increasing physical dependence.
Reported smoking in public venues
Respondents were asked: “The last time you visited a [venue], was there smoking inside? Yes or No” for four venues: drinking establishments (bars and pubs), restaurants and cafés, public buses, and enclosed shopping centres or malls. Each was asked only of those respondents who indicated visiting the venue in the past six months. Workplace smoking prevalence was asked only of respondents who reported working outside of the home: “In the last month, have people smoked in indoor areas where you work? Yes or No.” The workplace measure was thus a more stringent measure (report over a month v last time) of smoke‐free status. Because our respondents were a representative sample of smokers in each country, their responses constitute a reasonably representative sample of estimates of smoking prevalence in each type of venue in each country.
Respondents were asked about perceived levels of smoke in pubs: “Compared to a year ago, would you say that there is less smoke in the air, more, or about the same amount of smoke in the air in pubs and bars?” Irish respondents at post‐legislation were asked about enforcement: “In your experience, to what extent are your local pubs and bars enforcing the smoke‐free law: Not at all, somewhat, or totally?”
Smoking policies in private venues: homes and cars
Respondents were asked about their smoking in two important private venues—home: “Which of the following best describes smoking in your home: smoking is allowed anywhere in your home, smoking is never allowed anywhere in your home, or “something in‐between?”; and cars: “When you are in a car or other private vehicle with non‐smokers, do you: (1) smoke as you normally smoke, (2) never smoke, or (3) something in‐between?”
Visits to pubs and length of visit
At post‐legislation, respondents were asked two questions: “Do you visit pubs more often than a year ago, less often, or about the same?”; and “When you visit, do you tend to stay longer, less time, or the same amount of time as a year ago?”
Support for smoke‐free laws
Policy support was assessed in three ways. First, all respondents were asked whether smoking should be allowed in “all indoor areas, in some indoor areas, or not allowed indoors at all” in each of 10 public places: hospitals, workplaces, public buses, trains, major railway stations, restaurants and cafés, fast food outlets, drinking establishments (for example, pubs or bars), enclosed shopping centres and shopping malls, and covered stands in football grounds.
Policy support for total bans on smoking in pubs were asked in two additional ways. At post‐legislation, respondents were asked a direct question about support for banning smoking in pubs: “Do you support or oppose [Ireland: “the”; UK: “a”] total ban on smoking inside pubs?” Finally, at post‐legislation, Irish respondents were also asked for their overall assessment of the smoke‐free legislation in Ireland in this way: “Overall, would you say that the bans on smoking in pubs and other places in Ireland has been a good thing or a bad thing?”
Reported behavioural impact of the Irish law
At post‐legislation, Irish respondents were presented with a list of behaviours (table 2) that they might have adopted to adjust to the law, and responded yes, no, or not applicable for each. Those responding “not applicable” were not included in the analysis.
Table 2 Reported behavioural impact of the smoke‐free law among Irish smokers (n = 769).
| Irish smokers at post‐legislation wave (n = 640) | % “Yes” (95% CI) |
|---|---|
| Has the smoke‐free law: | |
| Made you more likely to quit smoking? (n = 636) | 46 (41 to 50) |
| [made you] cut down on the number of cigarettes you smoke? (n = 639) | 60 (55 to 64) |
| [made you] go outside to smoke when at a pub or restaurant? (n = 638) | 94 (92 to 96) |
| [led you to] use stop‐smoking medications like the nicotine patch or gum? (n = 626) | 14 (11 to 17) |
| Have you avoided going to pubs because of the law? (n = 632) | 35 (30 to 39) |
| Have you avoided going to restaurants because of the law? (n = 640) | 18 (15 to 22) |
| Irish smokers who reported quitting at post‐legislation wave (n = 119) | |
| Did the smoke‐free law make you more likely to quit smoking? (n = 116) | 80 (71 to 88) |
| Has the law helped you stay quit? (n = 118) | 88 (81 to 95) |
| Has it made you more likely to use stop‐smoking medications like the nicotine patch or gum? (n = 119) | 34 (24 to 45) |
| Have you avoided going to pubs because of the law? (n = 112) | 16 (8 to 24) |
| Have you avoided going to restaurants because of the law? (n = 110) | 8 (2 to 13) |
Survey weights
Survey weights for pre‐legislation respondents were constructed beginning with reciprocals of inclusion probabilities. The sample of households was self weighting, and within a sampled household, the inclusion probability for a sampled individual was the reciprocal of the number of adult smokers in the household. Adjustments were made for departures from proportional allocation to strata and were calibrated to sum to numbers of smokers in age‐sex groups, according to data from the 2002 National Health and Lifestyle Survey for Ireland25 and the 2001 General Household Survey for the UK.26 For post‐legislation respondents, pre‐legislation wave weights were adjusted for differential attrition in geographic strata and were again calibrated to the prevalence numbers from each country's reference surveys.
Analyses
Generalised estimating equation models (GEE)27 were fitted and their associated odds ratios computed in analyses of: (1) whether reported smoking in key venues decreased to a greater extent in Ireland from pre‐legislation to post‐legislation, than it did in the UK; and (2) whether support for smoke‐free policies (specifically, support for a total ban) increased to a greater extent in Ireland from pre‐ to post‐legislation, than it did in the UK, controlling for age, sex, ethnicity, education, income, cigarettes per day, time after waking until first cigarette, and prior quit attempts. For example, the between‐country difference in support for a complete ban in a particular venue (for example, restaurants) was tested as the country X wave interaction effect in the GEE model. Analyses and descriptive statistics were weighted as described above. For consistency in reporting, odds ratios were inverted, where necessary, so that those greater than 1 indicate favourable changes due to the Ireland law (lower reported smoking; greater support for the law). McNemar's tests were conducted for changes in proportions over time. T tests were conducted for differences in country means, and χ2 tests were conducted for differences in country proportions. Additional analyses were also performed to check the robustness of the results across alternative analytic approaches: (1) unweighted versions of the GEE models described above; and (2) multiple logistic regression with respondents' reported smoking or support for smoke‐free policies at post‐legislation as the dependent variables, with their pre‐legislation responses as an additional covariate; these logistic regression analyses were conducted in two ways—weighted and unweighted. The results of the analyses from these alternative approaches are not presented here because they yielded similar conclusions and point estimates as the weighted GEE approach, thus demonstrating the robustness of the findings that are presented. All analyses were conducted using SAS version 9.1.
RESULTS
Reported smoking in public venues
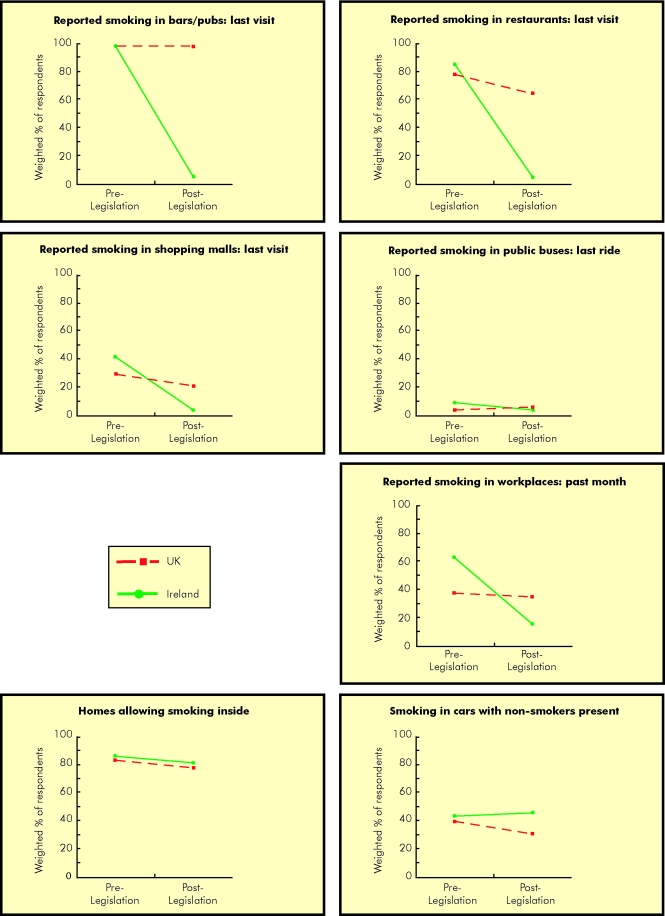
Figure 1 presents the percentage of smokers that observed smoking in key venues in Ireland and the UK both before and after the implementation of the Irish smoke‐free law. In the four venues at the top of fig 1, there was a near total absence of smoking at last visit. Most dramatic was the change in bars/pubs, where smoking in Ireland went from 98% to 5% (p < 0.0001), but remained nearly unchanged in the UK, from 98% to 97% (p = 0.462). The difference in restaurants was also dramatic, with Ireland decreasing from 85% to 3% (p < 0.0001) and the UK going from 78% to 62% (p < 0.001). Reported smoking in shopping malls decreased from 40% to 3% in Ireland (p < 0.0001), and from 29% to 22% in the UK (p = 0.012). These declines in Ireland from pre‐legislation to post‐legislation, relative to the UK, were significant in three of the four venues—bars/pubs, restaurants, and shopping malls (all p < 0.001; all adjusted odds ratios (OR) > 9); it was not significant for public buses (p = 0.121). Reported smoking in workplaces over the last month declined dramatically in Ireland (62% to 14%), relative to the UK (37% to 34%) (adjusted OR 8.89, 95% confidence interval (CI) 8.14 to 9.33, p < 0.0001).
Figure 1 Reported smoking in key venues at pre‐ and post‐legislation by country.
Perceptions of level of smoke in pubs
At post‐legislation, 98% of Irish smokers said that there was less smoke in pubs than one year ago, 1% said “the same”, and 1% said that there was more smoke. The corresponding percentages in the UK were 36% “less smoke”, 61% “the same”, and 3% “more”.
Smoking policies in private venues: homes and cars
At the bottom of fig 1 are reported smoking policies in two private venues—homes and cars. Inconsistent with the speculation that reductions of smoking in public venues might lead to greater levels of smoking in private venues,28 there was a significant decrease in the percentage of Irish homes where smoking was allowed (from 85% to 80%, p = 0.002), similar to the decrease in the UK (from 82% to 76%, p = 0.003). There was no significant change in reported smoking in cars in Ireland (42% to 45%, p = 0.33), whereas there was a decrease in the UK (from 38% to 30%, p = 0.005).
Enforcement of the law in pubs
At the post‐legislation wave, 94% of Irish smokers reported that pubs were enforcing the law “totally”, 5% said “somewhat”, and 2% said “not at all.”
Visits and length of visits to pubs
At post‐legislation, 41% of Irish smokers reported visiting pubs less often than a year ago, 57% said the same, and 3% reported visiting pubs more often. The corresponding percentages in the UK were 21% less often, 72% same, and 7% more often. About 34% of Irish smokers reported spending less time in pubs, 64% reported spending the same amount of time, and 2% reported spending more time. The corresponding percentages in the UK were 14% less time, 81% same, and 5% more time.
Support for smoke‐free laws
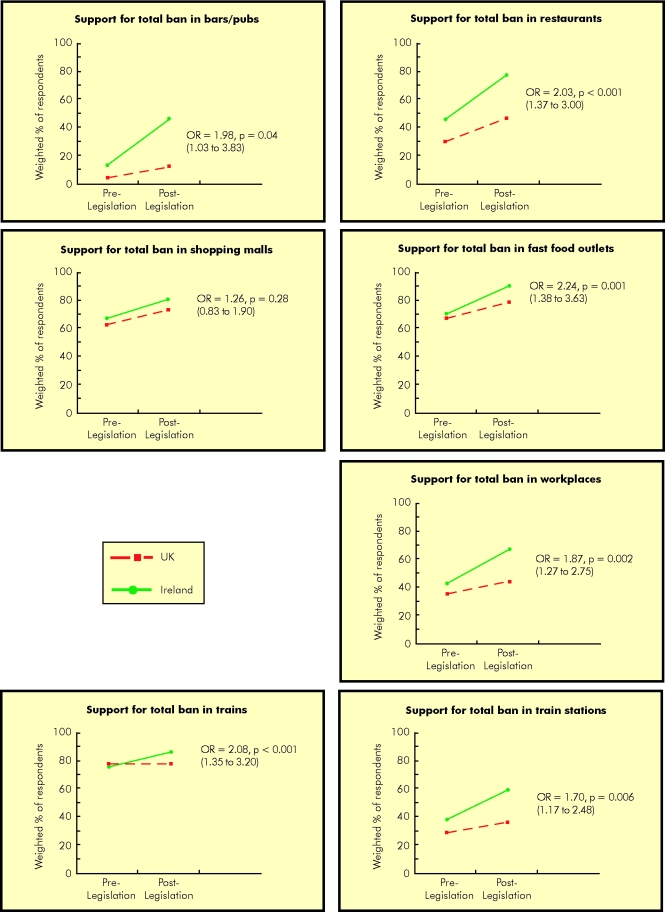
Figure 2 presents support for total bans on smoking in seven key venues, accompanied by the odds ratios for the difference in support for a ban in a given venue among Irish smokers from pre‐legislation to post‐legislation, compared to that difference among UK smokers over the same period of time, controlling for support at pre‐legislation, age, sex, ethnicity, education, income, cigarettes/day, time after waking until first cigarette, and prior quit attempts. In each venue, the level of support in Ireland increased, both in absolute terms and in comparison to the UK. The most striking result was support for a total ban in bars/pubs, where Ireland increased from 13% to 46%.
Figure 2 Support for total bans in key venues at pre‐ and post‐legislation by country.
The direct question regarding support for a total smoking ban in pubs yielded similar results: 64% of Irish smokers supported or strongly supported a total ban in pubs, compared to 25% of UK smokers (p < 0.0001). And in the question asking Irish smokers for their overall assessment of the smoke‐free legislation, 83% reported that the smoke‐free law was a “good” or a “very good” thing.
Reported behavioural impact of the smoke‐free law among Irish smokers
Table 2 presents the reactions to the smoke‐free law at post‐legislation among Irish smokers who were still smoking and among those who had quit. Of note, nearly half (46%) of smokers reported that the smoke‐free law had made them more likely to quit smoking. Of those who had quit, 80% reported that the law helped them to quit and 88% said it helped them to stay quit.
Table 2 also presents reported avoidance behaviours: 35% of smokers and 16% of quitters reported avoiding going to pubs because of the law and 18% of smokers and 8% of quitters reported avoiding going to restaurants because of the law. However, the proportion of Irish respondents reporting visiting a pub at least once in the last six months did not change significantly after the law was implemented (96% to 93%), compared to UK respondents (85% to 83%) (difference between Ireland and UK over time was not significant, p = 0.18).
DISCUSSION
This quasi‐experimental national cohort study demonstrates that the Ireland smoke‐free workplace law has led to near total reductions in observed tobacco smoke pollution in key public venues, notably restaurants and bars/pubs. These findings presage considerable reduction of the death and disability due to TSP among Irish pub workers29 and, more generally, among Irish workers and the Irish population as a whole. Evidence of the positive health impact of the Irish law has been found in a recent study of Irish pub workers.30
The level of compliance with the Irish law is striking. The point prevalence of smoking in bars/pubs of 5% in Ireland at post‐legislation compares favourably to past studies.31,32,33 There was no evidence that the reduction in smoking in public venues was associated with increased smoking in private venues. There was actually a significant decrease in the proportion of Irish homes where smoking was allowed inside (that is, an increase in home bans).
The dramatic reduction in TSP across all public venues was accompanied by a significant increase in support for a total ban in seven venues, consistent with past studies16,17,18,19,21,34,35 and with findings in social psychology that changing behaviour is often followed by changes in attitudes and beliefs consistent with the behaviour change. Increase in support was most dramatic in venues where pre‐policy support was lowest (for example, bars/pubs and restaurants), suggesting that policymakers that stay the course in implementing comprehensive smoke‐free policies are likely to experience increased support among smokers after implementation.
What this paper adds
Tobacco smoke pollution (TSP) poses a significant risk to public health, and thus smoke‐free laws are a critical policy for tobacco control. Past research suggests that such laws can be effective in reducing TSP and some evidence suggests that support for smoke‐free laws increases among smokers. In March 2004, the Republic of Ireland was the first country to implement a comprehensive smoke‐free law with few exemptions and no allowances for designated smoking areas within restaurants and bars.
The ITC Ireland/UK Survey, a cohort survey of nationally representative samples of adult smokers in Ireland before and after the implementation of the Ireland law, and a comparison sample in the UK, is the first evaluation of the effects of a national level comprehensive smoke‐free law. The findings demonstrate that the law led to near total elimination of tobacco smoke pollution across a wide range of public venues, including restaurants and bars, and that this was accompanied by increasing support among smokers for smoke‐free laws in public venues. The findings from this quasi‐experimental study provide strong evidence supporting comprehensive smoke‐free laws, as called for in the Framework Convention on Tobacco Control.
Although not a direct goal, the Irish law was also associated with favourable movement toward quitting, consistent with other studies,9,10,36 supporting the view that the absence of smoking in public venues, particularly those formerly associated with cues for smoking, encourages quitting and increases the likelihood of successful quitting.37
This study focuses on the effects of the Irish smoke‐free law, but the “control” group was a national representative sample of adult smokers in the UK, which at the time of Wave 2 was considering its own level and timing of a smoke‐free law. Since that time, Scotland has passed its own comprehensive smoke‐free law, which was implemented in March 2006, and Northern Ireland will also be going smoke‐free in April 2007. A Health Bill which incorporates new comprehensive smoke‐free legislation for England and Wales is currently before Parliament and likely to be implemented in mid‐2007. The ITC Project will continue to evaluate the implementation of smoke-free legislation in Scotland38 and then in England, with expanded samples in both countries.
The current study provides evidence relevant to the UK. At post‐legislation, the percentage of UK workplaces where smoking was reported in the last month was significantly lower (34%) than it had been in Ireland before their smoke‐free law (62%, p < 0.0001). In addition, support for total bans in five venues (restaurants, shopping malls, fast food outlets, trains, and “workplaces”) in the UK was equal to or higher than the level of support in Ireland at the pre‐legislation wave. Thus, all things being equal, implementation of a comprehensive smoke‐free law in the UK would seem to be an easier proposition than it was in Ireland.
The present study includes only smokers and is thus, by itself, insufficient to evaluate fully the economic impact of the Irish smoke‐free law on the hospitality trade. Reviews of economic impact conclude that smoke‐free laws lead to either no effect or a slight positive effect,14,39 suggesting that reported declines in patronage among smokers are compensated for by increased patronage among non‐smokers, as occurred in New York City after its 1995 smoke‐free restaurant law.40,41 In Ireland, non‐smokers outnumber smokers by a factor of over three.
In conclusion, this study of smokers demonstrates the success of Ireland's comprehensive smoke‐free law. The pre‐legislation campaign was successful in diffusing criticism and countering the arguments of the opponents,42 and the law was well implemented. The Irish law is increasingly popular and is bringing public health benefits to smokers and non‐smokers alike. These findings support comprehensive smoke‐free laws, as called for in the FCTC. More generally, these findings demonstrate the power of tobacco control policies as population‐level interventions that can effect sweeping and dramatic changes in cultural norms in the service of public health. The transformation of smoke‐free laws in Ireland from unthinkable imposition to commonsense public health initiative is a remarkable example for the rest of the world.
ACKNOWLEDGEMENTS
We thank Taryn Sendzik, Ruth Loewen, Bruce Packard, Lauren Salter, Mark Harris, Pat Timmins, and Tara Elton‐Marshall for their assistance. We thank Richard J O'Connor and Christian Boudreau for their comments on preliminary versions of this article.
DETAILS OF AUTHORS' CONTRIBUTIONS TO THIS MANUSCRIPT
All authors reviewed and approved the final version of this manuscript.
Geoffrey T Fong is the guarantor of this paper. He participated in the research design, preparation of study materials and protocol, had oversight and management of the data collection process, the data analysis, interpretation of the data analysis, and led the preparation of drafts of this manuscript.
Andrew Hyland participated in the research design, preparation of study materials and protocol, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Ron Borland participated in the research design, preparation of study materials and protocol, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
David Hammond participated in the research design, preparation of study materials and protocol, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Gerard Hastings participated in the research design, preparation of study materials and protocol, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Ann McNeill participated in the research design, preparation of study materials and protocol, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Susan Anderson participated in the research design, preparation of study materials and protocol, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
K Michael Cummings participated in the research design, preparation of study materials and protocol, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Shane Allwright participated in the preparation of study materials, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Maurice Mulcahy participated in the interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Fenton Howell participated in the interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Luke Clancy participated in the interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Mary E Thompson participated in the research design, preparation of study materials and protocol, interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Greg Connolly participated in the interpretation of the data analysis, and in the preparation of drafts of this manuscript.
Pete Driezen conducted the data analysis, and participated in the interpretation of the data analysis and in the preparation of drafts of this manuscript.
Abbreviations
CATI - computer assisted telephone interviewing
FCTC - Framework Convention on Tobacco Control
GEE - generalised estimating equation
ITC‐4 - International Tobacco Control Four Country Survey
TSP - tobacco smoke pollution
Footnotes
* We use the term “tobacco smoke pollution” although other terms, such as “environmental tobacco smoke”, “secondhand smoke”, and “passive smoke” have been used.
† For the proportions in figs 1 and 2, approximate sampling standard errors may be computed by taking the simple random sampling (unweighted) standard error (square root of (p(1–p)/n), where p is the observed proportion, and n is 769 in Ireland and 416 in the UK) and then multiplying by a factor of 1.2 to account for the variation in the sampling weights.
Funding for this study was provided by grants from the National Cancer Institute of the USA (through R01 CA 90955 and through the Roswell Park Transdisciplinary Tobacco Use Research Center, P50 CA111236), Cancer Research UK, Flight Attendants' Medical Research Institute (012525), Research Institute for a Tobacco‐Free Society, Dublin, and unrestricted grants from Glaxo Smith Kline and from Pfizer. The funding sources had no role in the study design, in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the paper for publication.
Competing interest statement: All authors declare that the answer to the questions on your competing interest form www.bmj.com/cgi/content/full/317/7154/291/DC1 are all “No” and therefore have nothing to declare.
Ethics approval: As indicated in the manuscript, the study protocol was reviewed and cleared by the Research Ethics Board of the University of Waterloo.
References
- 1.California Environmental Protection Agency Health effects of exposure to environmental tobacco smoke. Smoking and Tobacco Control Monograph, 10. Bethesda, Maryland: National Cancer Institute, 2001
- 2.Glantz S A, Parmley W. Passive smoking and heart disease: epidemiology, physiology, and biochemistry. Circulation 1991831–12. [DOI] [PubMed] [Google Scholar]
- 3.Borland R, Chapman S, Owen N.et al Effects of workplace bans on cigarette consumption. Am J Public Health 199080178–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borland R, Owen N, Hocking B. Changes in smoking behaviour after a total workplace smoking ban. Aust J Public Health 199115130–134. [DOI] [PubMed] [Google Scholar]
- 5.Stillman F A, Becker D M, Swank R T.et al Ending smoking at the Johns Hopkins Medical Institutions. An evaluation of smoking prevalence and indoor air pollution. JAMA 19902541565–1569. [PubMed] [Google Scholar]
- 6.Brownson R C, Hopkins D P, Wakefield M A. Effects of smoking restrictions in the workplace. Ann Rev Public Health 200223333–348. [DOI] [PubMed] [Google Scholar]
- 7.Borland R, Davey C. Impacts of smoke‐free bans and restrictions (chapter 14). In: Boyle P, Gray N, Henningfield J, et al, eds. Tobacco: science, policy and public health. Oxford: Oxford University Press, 2004
- 8.Eisner M D, Smith S K, Blanc P D. Bartenders' respiratory health after establishment of smoke‐free bars and taverns. JAMA 19982801909–1914. [DOI] [PubMed] [Google Scholar]
- 9.Fichtenberg C M, Glantz S A. Effect of smoke‐free workplaces on smoking behaviour: systematic review. BMJ 2002325188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glasgow R, Cummings K M, Hyland A. Relationship of worksite smoking policy to changes in employee tobacco use: findings from COMMIT. Tob Control 19976(suppl 2)S44–S48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Repace J. Respirable particles and carcinogens in the air of Delaware hospitality venues before and after a smoking ban. J Occup Environ Med 200446887–905. [DOI] [PubMed] [Google Scholar]
- 12.Travers J M, Cummings K M, Hyland A.et al Indoor air quality in hospitality venues before and after implementation of a clean indoor air law—New York, 2003. MMWR Morb Mortal Wkly Rep 2004531038–1041. [PubMed] [Google Scholar]
- 13.Sargent R P, Shepard R M, Glantz S A. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. BMJ 2004328977–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scollo M, Lal A, Hyland A.et al Review of the quality of studies on the economic effects of smoke‐free policies on the hospitality industry. Tob Control 20031213–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borland R, Yong H H, Siahpush M.et al Support for and reported compliance with smoke‐free restaurants and bars by smokers in four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control 200615(suppl III)iii34–iii41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andrews J. Reducing smoking in the hospital. An effective model program. Chest 198384206–209. [DOI] [PubMed] [Google Scholar]
- 17.Becker D M, Conner H F, Waranch R.et al The impact of a total ban on smoking in the Johns Hopkins Children's Center. JAMA 1989262799–802. [PubMed] [Google Scholar]
- 18.Biener L, Abrams D B, Emmons K.et al Evaluating worksite smoking policies: Methodologic issues. New York State J Med 1989895–10. [PubMed] [Google Scholar]
- 19.Gottlieb N H, Eriksen M P, Lovato C Y.et al Impact of a restrictive worksite smoking policy on smoking behavior, attitudes, and norms. J Occup Med 19903216–23. [DOI] [PubMed] [Google Scholar]
- 20.Borland R, Owen N, Hill D.et al Changes in acceptance of workplace smoking bans following their implementation: a prospective study. Prev Med 199019314–322. [DOI] [PubMed] [Google Scholar]
- 21.Cunningham R. National and subnational legislation requiring 100% smoke‐free restaurants and bars. Report by the Canadian Cancer Society, 1 May 2006
- 22.Binson D, Canchola J A, Catania J A. Random selection in a national telephone survey: a comparison of the Kish, next‐birthday, and last‐birthday methods. J Off Stat 20001653–60. [Google Scholar]
- 23.Fong G T, Hammond D, Laux F L.et al The near‐universal experience of regret among smokers in four countries: findings from the International Tobacco Control Policy Evaluation Survey. Nicotine Tob Res 20046(suppl 3)S341–S351. [DOI] [PubMed] [Google Scholar]
- 24.Fagerstrom K O. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav 19783235–241. [DOI] [PubMed] [Google Scholar]
- 25.Department of Health and Children, Health Promotion Unit National health and lifestyle survey. Dublin 2003
- 26. Office for National Statistics, Social Survey Division, General household survey, 2001–2002 [computer file]. 2nd ed. Colchester, Essex: UK Data Archive [distributor], July 2003, SN4646
- 27.Liang K Y, Zeger S L. Longitudinal data analysis using generalized linear models. Biometrika 19867313–22. [Google Scholar]
- 28.Reid J. (The Secretary of State for Health, England). Testimony. The government's public health white paper (Cm 6374). Hearing Before the House of Commons Health Committee, UK, 23 February 2005
- 29.Mulcahy M, Repace J L. Passive smoking exposure and risk for Irish bar staff. Proceedings Indoor Air 2002: 9th International Conference on Indoor Air Quality and Climate. 2002 June 30–July 5; Monterey, California 2002
- 30.Allwright S, Paul G, Greiner B.et al Legislation for smoke‐free workplaces and health of bar workers in Ireland: before and after study. BMJ 20053311117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weber M D, Bagwell D A S, Fielding J E.et al Long term compliance with California's Smoke‐Free Workplace Law among bars and restaurants in Los Angeles County. Tob Control 200312269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chapman S, Borland R, Lal A. Has the ban on smoking in New South Wales restaurants worked? A comparison of restaurants in Sydney and Melbourne. Med J Australia 2001174512–515. [DOI] [PubMed] [Google Scholar]
- 33.Borland R, Pierce J P, Burns D M.et al Protection from environmental tobacco smoke in California. JAMA 1992268749–752. [PubMed] [Google Scholar]
- 34.Tang H, Cowling D W, Lloyd J C.et al Changes of attitudes and patronage behaviors in response to a smoke‐free bar law. Am J Public Health 200393611–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gilpin E A, Lee L, Pierce J P. Changes in population attitudes about where smoking should not be allowed: California versus the rest of the USA. Tob Control 20041338–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bauer J E, Hyland A, Li Q.et al Longitudinal assessment of the impact of smoke‐free worksite policies on tobacco use. Am J Public Health 2005951024–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trotter L, Wakefield M, Borland R. Social cued smoking in bars, night clubs, and gaming venues: a case for introducing smoke‐free policies. Tob Control 200211300–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haw S J, Gruer L, Amos A.et al Legislation on smoking in enclosed public places in Scotland: how will we evaluate the impact? J Public Health 20062824–30. [DOI] [PubMed] [Google Scholar]
- 39.Smoke Free Europe Partnership Smoke Free Europe makes economic sense: A report on the economic aspects of smokefree policies. 2005 [cited 2005 Oct 3]. http://www.smokefreeeurope.com/economic_report.htm
- 40.Hyland A, Cummings K M. Consumer response to the New York City Smoke‐Free Air Act. J Public Health Management Practice 1999528–36. [DOI] [PubMed] [Google Scholar]
- 41.Corsun D L, Young C A, Enz C A. Should NYC's restaurateurs lighten up? Effects of the city's smoke‐free air act. Cornell Hotel and Restaurant Admin Quarterly, April 199625–33.
- 42.Howell F. Ireland's workplaces, going smoke free. BMJ 2004328847–848. [DOI] [PMC free article] [PubMed] [Google Scholar]