Abstract
Objectives
In 2003 an estimated 87 000 AIDS deaths and approximately 110 000 new infections occurred in Malawi. This paper aimed to analyse and review HIV prevalence trends in conjunction with other second generation surveillance data including behavioural data and, therefore, to describe trends in HIV prevalence and behaviours related to HIV transmission.
Methods
In order to determine the extent of the problem, HIV prevalence in Malawi has been monitored through testing women attending antenatal clinics in 19 sentinel sites consistently since 1994. These sites are classified as urban, semi‐urban, and rural.
Results
The overall HIV prevalence for all 19 ANC sentinel sites in 2003 was 19.8% (95% CI 19.0% to 20.7%). The central region urban/semi‐urban sites showed a decline in prevalence from 1999 to 2003. Since 1997, overall national incidence estimates remained stable. This stable incidence estimate is supported by the proxy of fairly stable prevalence in ANC attendees aged 15–24 years. HIV sentinel surveillance data for Lilongwe city showed a significant linear decline in prevalence (p<0.00001) over the last seven years for both all ANC attendees and those aged 15–24 years suggesting that incidence has declined over the time period.
Conclusion
The available epidemiological and behavioural surveillance data show that HIV prevalence has declined in several urban and semi‐urban areas, specifically in the central region with Lilongwe (capital of Malawi) showing exceptionally strong evidence of decline. In some rural areas, particularly in the northern region there is some evidence of an increasing trend in HIV prevalence.
Keywords: HIV surveillance, HIV prevalence, Malawi
HIV/AIDS is a leading cause of death in the economically productive age group in Malawi. In 2003 an estimated 87 000 of Malawi's 12 million people died from AIDS, and approximately 110 000 new infections occurred.1 The 2003 HIV positive rate in women attending antenatal clinics (ANCs) was 19.8% among all clients, and estimated at 21.2% in urban areas and 14.5% in rural areas.2 The HIV/AIDS epidemic in the country has resulted in a major increase in the number of patients with tuberculosis and other related diseases. A 2004 countrywide survey of patients with tuberculosis found an HIV seroprevalence rate of 72%.3
In monitoring the HIV epidemic in Malawi, information is regularly collected on the HIV epidemic through selected ANC sentinel sites using consistent methods. The main objective of these surveys is to provide data on the occurrence, spread, and distribution of HIV infection among ANC attendees. HIV prevalence data was originally collected at only one site in 1985, but the number of sites steadily increased to 19 in 1994 as the National AIDS Control Programme became particularly interested in monitoring prevalence trends.
This paper aims to analyse and review trends in HIV prevalence in conjunction with other second generation surveillance data including behavioural data to obtain a more complete picture of the epidemic and interpret the HIV situation, with the objective of describing trends in HIV prevalence and behaviours related to HIV transmission. Analysis of trends in HIV seroprevalence data over time is key to understanding the dynamics of the epidemic.
Methods
HIV sentinel surveillance
There has been consistent monitoring of HIV prevalence at the 19 ANC sentinel sites (see above) since 1994 (fig 1). The sites are classified as urban (major cities), semi‐urban (district hospitals), and rural (health centres) to monitor HIV prevalence in the three subpopulations. The urban sites were purposefully selected whereas the semi‐urban and rural sites were selected through simple random sampling after stratifying by region (north, central, south). This was because of differences in progression of the HIV epidemic in the regions, with the southern regions having high HIV prevalence followed by the central and northern regions. The rural ANC sites are mostly located in smaller population centres (areas with relatively higher socioeconomic status compared with the true rural areas) and therefore may not represent the true picture of HIV in Malawi's rural population.
Figure 1 Map of Malawi showing HIV sentinel antenatal clinic sites. HC, health centre; DH, district hospital; H, hospital.
During the period of sample collection all consecutive women attending ANC services for the first time during the current pregnancy were eligible for enrolment. Enrolment continued either until the predetermined sample sizes were reached or to eight weeks, based on World Health Organization (WHO) recommendations.4 The sample sizes were determined on the basis of likelihood of achieving the set sample sizes during the eight week period of data collection. The desired sample sizes were: 200 women in rural sites, 500 women in semi‐urban sites, and 800 women in urban sites. In some rural sites the sample size of 200 was not achieved even after the eight week period of data collection was over because of low attendance.
Routine demographic data and blood left over from routine syphilis testing were used in the analysis. Samples were anonymous and unlinked, in accordance with the WHO guidelines on HIV surveillance.5 Testing for HIV was done centrally using a single enzyme immunoassay (EIA assay; Vironostika HIV Uniform II Plus, Biomerieux, the Netherlands) in accordance with the recommendations of the WHO on HIV testing for surveillance purposes.4
We analysed HIV prevalence trends for sentinel surveillance sites by individual sites using χ2 for linear trends. Trends are also presented by region, looking at mean prevalence in urban/semi‐urban, and rural sites. We did not calculate the medians as there were only three to four sites in each group. The Joint United Nations Programme on AIDS (UNAIDS)/WHO Estimation and Projection Package (EPP) and Spectrum modelling software6 was used to develop national HIV prevalence estimates. This method of estimating HIV prevalence has been described elsewhere.1 Epidemic trend curves were fit to each sentinel site using EPP and then assigned to represent the urban or semi‐urban and rural prevalence for each district. Prevalence was multiplied by the urban/semi‐urban and rural adult population estimates for the district and the estimated number of HIV positive individuals was summed and divided by the national population estimate for individuals between the ages of 15 and 49 years. Other variables considered in the estimation process have been described elsewhere.1
Behavioural surveys
The main sources of knowledge and behavioural data in Malawi are the two Malawi Demographic and Health Surveys (1992 MDHS and 2000 MDHS) and the Malawi Knowledge, Attitudes, and Practices in Health survey (1996 MKAPH). These surveys used a nationally representative sampling frame to select male and female respondents of reproductive age, women aged 15–49 years and men aged 15–54 years. Data on a variety of demographic and health variables were collected; however, some questions changed over time. The 1992 MDHS primarily asked questions regarding knowledge of HIV, modes of transmission, misconceptions, and knowledge and use of condoms. By the mid‐1990s knowledge of HIV was nearly universal, so later surveys focused on preventive behaviours.5 The 1996 MKAPH and the 2000 MDHS asked questions on sexual behaviour, such as number of partners and status of relationships, abstinence, and use of condoms with various partners. The 2000 MDHS included a newly developed HIV/AIDS module that collected data to calculate the national response indicators recommended by UNAIDS.7,8,9
Sample sizes for each of the three surveys were different because of the differences in the areas of focus in the said surveys: in the 1992 survey there were 4549 women and 1151 men; in the 1996 survey there were 683 women and 2658 men; and in the 2000 survey there were 13 220 women and 3092 men. The samples for 1992 and 1996 were drawn from the 1987 National Census sampling frame, whereas the 2000 survey used the new 1998 Census.10
Ethical approval was obtained from the Malawi National Health Sciences Research Committee of the Malawi Ministry of Health.
Results
HIV prevalence
In 2003, the overall HIV prevalence for all 19 ANC sentinel sites was 19.8% (95% CI 19.0% to 20.7%), with a median of 17.0% among the sites.2 The highest prevalence was in Nsanje District Hospital (32.9%), a semi‐urban site in the southern region, and the lowest prevalence was in Kamboni Health Centre (6.7%), a rural site in the central region. The prevalence at the sites varied widely by urban/rural status and by region. Prevalence is quite high in all three urban sites (above 15 percent), and six of the eight rural sites have a prevalence above 10 percent. Eight of the 19 total sites have prevalence above 20 percent. The sample sizes provide prevalence estimates with an error of about ±5 percentage points for rural sites (n = 200) to ±3 per cent in urban sites (n = 800). The prevalence figures in Malawi are consistent with patterns of a generalised epidemic, similar to many other countries in sub‐Saharan Africa.
Figure 2 shows trends of mean HIV prevalence for urban/semi‐urban and rural sites by region. HIV prevalence has been consistently higher in the urban/semi‐urban sites than in the rural sites since in 1994. HIV prevalence is clearly highest in the southern region, where it is about double the level in the central and northern regions. The exact pattern of increase in prevalence by region before 1994 is uncertain since there is very little surveillance information available for that period and in many sites that started in 1994 had already reached stable prevalence. Therefore, assessing timing of the start of epidemic, which may affect epidemic progression, is not possible.
Figure 2 Trends of mean HIV prevalence for HIV sentinel site antenatal clinic attendees by region and urban/semi‐urban and rural status, 1994–2003.
The central urban/semi‐urban sites show a decline in prevalence from 26.9% in 1999 to 16.7% in 2003. Three of the four urban/semi‐urban sites show a significant linear decline (p<0.001) since 1999. The southern sites also show some decline in prevalence in urban/semi‐urban sites, with two of the four sites reporting a decline in the same time period, though neither of the two is significant. Over the 10 year period, both the southern and central rural sites have had an indefinite trend, suggesting a stable prevalence. The northern region shows an indefinite trend in the urban/semi‐urban sites (none of the three sites show a consistent decline or increase) and an upward, although not significant, trend in prevalence in rural sites since 1999.
National adult HIV prevalence for 2003 was estimated at 14.4% based on ANC surveillance data using the EPP and Spectrum software packages.1 The prevalence trend modelled in Spectrum has remained fairly stable for the past seven years. Prior to that, infections increased rapidly in the early 1990s, after which prevalence increased at a slower pace. Also, national urban and rural adult prevalence rates were estimated at 23.0% and 12.3%, respectively. Similar to sentinel surveillance, HIV prevalence in adults in the southern region (19.1%) was significantly higher than prevalence in the central (9.8%) and northern (10.5%) regions since the beginning of the epidemic in 2003.
In order to validate HIV prevalence data obtained from ANC sentinel surveillance, a comparison was made between rural sites in Karonga and the Karonga Prevention study.11 The ANC sentinel surveillance prevalence for Kaporo Health Centre in Karonga district for 1999 and 2001 combined was 14.6% (95% CI 11.4% to 18.7%). In the Karonga Prevention Study, conducted in the mostly rural district in northern Malawi, 250 samples were collected from each of four ANC clinics representing the district for each year from 1999 to 2001. The prevalence was 10.4% (95% CI 9.3% to 11.5%) for 1999–2001.11 Although the Kaporo Health Centre catchment area may represent an area of higher population density than much of rural Karonga, these results have overlapping confidence intervals indicating their similarity. In the Karonga study community prevalence data also was collected for adults aged 15 and older for three periods from 1989 to 2001. These Karonga community prevalence study data compare well with Karonga district prevalence data modelled in EPP and national rural prevalence trends estimated using Spectrum: 1989, 2.9%, 2.3%, 2.5%; 1992, 7.3%, 8.6%, 6.7%; 2000, 13.8%, 16.3%, 12.3%, respectively.
Incidence
HIV incidence could crudely be estimated from the HIV prevalence among the youngest individuals, such as 15–24 year olds in ANC surveys. Because these individuals would not have been sexually active for very long, their infections were likely to be relatively recent. Therefore, incidence trends in Malawi have been estimated using prevalence trends in young adults aged 15–24 years. This age group has been analysed as a proxy for incidence trends in the population. HIV prevalence for ANC attendees aged 15–24 years at all sentinel surveillance sites was fairly stable from 1995 (19.5%) to 2003 (18.3%)2 (fig 3).
Figure 3 Trends of HIV prevalence: HIV sentinel antenatal clinic (ANC) Lilongwe and national data for selected age groups, 1987–2003.
Overall HIV sentinel surveillance data for the capital city of Lilongwe (Bottom Hospital site) showed a significant linear decline (p<0.00001) in prevalence over the last seven years (fig 3). This longer decline is unique compared with the other sites in Malawi. Prevalence was 8.2% in 1987 when surveillance began, increased to peak at 27% by 1996, and declined to 16.9% in 2003.2 The linear decline is also seen in women aged 15–24 years (p<0.00001), a proxy for incidence trends. This is suggestive of behavioural change among young people in Lilongwe. However, further research is necessary to verify this observation and to characterise the behavioural change. Unfortunately no behavioural data specific to Lilongwe are available for thorough analysis of the observed trends.
Another proxy for incidence trends is prevalence in pregnant women expecting their first child. Prevalence stratified by gravidity is only available for 1999, 2001, and 2003, and is 22%, 15%, and 16%, respectively, for women with gravidity (National AIDS Commission, 2004, unpublished data). Given the limited data for the time period, it is difficult to interpret the trend as decreasing, though it does suggest that incidence has not been increasing over the last five years.
Using Spectrum software for national prevalence estimates, HIV incidence was estimated to be 1.8% per year in adults in 2003.1 Incidence peaked at 2.5% in 1992 and declined slightly until 1997, likely due to AIDS deaths reducing HIV infection among sexual contacts. Since 1997, prevalence estimates have remained stable possibly due to balancing between deaths and incidence.1
Sexual behaviour and knowledge
General awareness and knowledge
General awareness of HIV and AIDS is very high in Malawi according to the MDHS with 99% of women and 100% men reporting having heard of AIDS by 2000,9 however, comprehensive knowledge on prevention and transmission is low. Furthermore, comprehensive knowledge has not translated into behaviour change. Results from the three MDHS studies follow.4 Knowledge that an individual infected with HIV can appear healthy has increased steadily from 1992 to 1996 to 2000: from 65% to 72% to 84%, respectively, in women, and 81% to 85% to 92%, respectively, in men. Women and men who know someone with or someone who has died of HIV/AIDS has also increased from 1996 to 2000 (from 68% to 72% and from 68% to 82%, respectively). The percentage of women and men who spontaneously knew that condoms can be used to avoid HIV was low, but has been steadily rising among women; 8%, 21%, and 55% in 1992, 1996, and 2000, respectively. Similarly, the rise has been steady among men (26%, 47%, and 71% in 1992, 1996 and 2000, respectively). The increase is even more pronounced in young adults aged 15–24 years, in 2000 reaching 58% for women and 76% for men. Knowledge that HIV can be avoided through total abstinence also increased (women 24%, 18%, 66% and men 37%, 38%, and 72% in 1992, 1996, and 2000, respectively).
Comprehensive knowledge
From 1992 to 1996 there was an increase in the proportion of respondents in the MDHS reporting both condom use and limiting number of partners as ways of avoiding HIV (women 4% to 11% and men 18% to 21%, respectively). Comparison with 2000 data is difficult due to changes in the questionnaire. In 2000, 68% of women and 74% of men knew of both means to avoid HIV based on responses to prompted questions compared with only 15% and 12% who spontaneously offered the response.
Sexual behaviour
MDHS describes stable trends in abstinence among adult women from 1996 to 2000, with 21% and 22% of adult women reporting not having sex within 12 months of the survey, and a slight increase among adult men, 17% and 20% for the same years. Unmarried urban young men (aged 15–24 years) reported an increase in abstaining from sex from 45.1% in 1996 to 55.8% in 2000. Their rural counterparts reported stable levels (48.7% and 49.6%), as did both urban and rural young women (68.5% and 71.1%, and 67.4% and 75.2%, respectively).
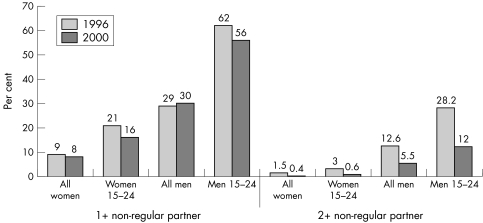
The MDHS indicates that whereas the number of adults having sex with one or more non‐regular partners was stable between 1996 and 2000, there was a decline among young adults (15–24 years): women 21% and 16%, and men 62% and 56%, in 1996 and 2000, respectively. While the proportions of those having sex with two or more non‐regular partners are lower, the decline between 1996 and 2000 is quite pronounced: 3.0% to 0.6% for women and 28.2% to 12.0%, for men from 1996 to 2000 (fig 4). The proportions of people having sex with non‐regular partners are likely adequate to sustain the epidemic.
Figure 4 Proportion of people having sex with non‐regular partners in the last 12 months by age and sex. Sources: 1996 Malawi Knowledge, Attitudes, and Practices in Health Survey; 2000 Malawi Demographic and Health Survey.
Condom use
Despite knowledge that condoms can be used to avoid HIV, their use in Malawi has remained low. In the 2000 MDHS, only 38% of men had ever used a condom, up from 24% in 1992. Also in 2000, only 8% of women had ever used a condom, almost the same level as in 1992 (7%). Although condom use at last sex with a non‐regular partner among all adult women and among those aged 15–24 years increased from 1996 to 2000, there has been no change among all adult men or young men (fig 5).
Figure 5 Proportion of people using a condom at last sex with non‐regular partners by age and sex. Sources: 1996 Malawi Knowledge, Attitudes, and Practices in Health Survey; 2000 Malawi Demographic and Health Survey.
Trends in other sexually transmitted infections
In 2000 the MDHS revealed a self‐reported prevalence of STI symptoms within the last 12 months of 1% among women and 2% among men.9 Sentinel surveillance surveys indicate a declining trend in syphilis. In 2003, prevalence of syphilis among pregnant women in Malawi attending ANC services was 2.7% compared with 4%, 7%, and 4% in 1995, 1996, and 1998.2
Mortality
The 1992 MDHS reported 6.5 female deaths per 1000 and 6.3 male deaths per 1000.7
The 2000 DHS showed an increase in death rate as follows; 11.3 female deaths per 1000 and 11.1 male deaths per 1000.9 Annual death rates have doubled in all age groups for women 20 years and older, whereas among men death rates have doubled only in the age group of 30 years and above.7,9 Crude death rates in the three Malawian censuses were as follows: 25 per 1000, 14.1 per 1000 and 21.1 per 1000 in 1977, 1987, and 1998, respectively.10 It seems the declining trend in mortality from 1977 to 1987 has been reversed with mortality significantly increasing during the 10 year period from 1987 to 1998.
Discussion
It is important to monitor the HIV/AIDS epidemic for identification of needs and opportunities for intervention. Efforts have been made to undertake second generation HIV surveillance designed to track and link behaviour to trends in biological data, to increase the explanatory power of surveillance data.
From the data presented above, it can be seen that HIV/AIDS remains a great challenge in Malawi. The epidemic has affected all districts and localities with HIV prevalence consistently and significantly higher in urban and semi‐urban areas compared with rural areas. There has been a significant linear decline from 1999 to 2003 in HIV prevalence in some urban and semi‐urban sites. Unlike the urban/semi‐urban sites, prevalence in some rural sites increased from 1999 to 2003. Socioeconomic dynamics in rural sites, which are located in smaller population centres, may be affecting these trends. For instance, Kaporo Health Centre, which is located along an economically active route in the north, and Mianga Health Centre, which is located near commercial tea estates, may increasingly have characteristics similar to those of urban areas, such as an increasing population with expanded sexual networks.
The HIV prevalence trends reflect regional differences, with the southern region consistently registering HIV prevalence higher than in the other two regions. From 1999, the trend for the central region has been declining prevalence. The reason for this is not clear. Similar declines are not seen in the north or south. Further research is necessary to explain the observed trends. Population and socioeconomic growth in Mzuzu city and areas along major transportation routes may be having an effect on the observed prevalence in the northern region.
National ANC prevalence data for women aged 15–24 years suggest that the rate of new infections in the newly sexually active young adult population has remained fairly stable, at least since 1995. Similarly, modelled incidence estimates have remained stable since 1997. This trend is a familiar curve where incidence peaks several years before prevalence as stable incidence balances with deaths due to AIDS and leads to stabilising of prevalence.
Overall HIV prevalence among antenatal attendees in Lilongwe (Bottom Hospital), one of the three major cities in Malawi, showed a long term decline over the past seven years, from 27% in 1996 to 16.9% in 2003. The decline was observed across all age groups. The linear decline present in women aged 15–24 years at this site suggests a decline in the incidence of HIV infection. Reasons for this decline are not clearly known in the absence of behavioural data specific to Lilongwe City. It should also be noted that the observed decline in HIV prevalence among the older age groups 25 years and above may in part be explained by increased mortality in this age group and reduced fertility (those previously HIV positive are less fertile and so not captured in subsequent ANC surveys) resulting in the decline of HIV prevalence. There is a need for locally specific complementary data for better interpretation of these results.
Prevalence of HIV is determined by the number of new HIV infections and the duration of disease or deaths. The doubling of mortality rates between the 1992 and 2000 DHS surveys may directly affect prevalence levels. Declines in HIV prevalence may also be due in part to reduced fertility among women as a result of HIV infection, though no information was analysed regarding this effect. On the other hand, declines could be due to reduced new HIV infection rates resulting from increased access to HIV information and other services in urban areas prompting a reduction in number of sex partners and increased condom use.
Data from behavioural surveys show that comprehensive knowledge of HIV and AIDS, reflected in the knowledge that using condoms and limiting sex partners can prevent infection, remains limited in Malawi. Large proportions of the population are still engaging in sex with non‐regular partners though there is some reduction in the number of both men and women with multiple partners. Condom use is increasing among women but remains low, and while higher among men remained stable in the late 1990s. Self‐reported STI indicates that people still engage in unsafe sex. This may explain why Malawi has not yet experienced prevalence decline at the national level. It appears that intervention programmes have left risky behaviour at substantial levels, although they could have contributed to the levelling‐off of the epidemic.
It should be noted that though intervention programmes have been implemented in some areas, multisectoral approaches were only initiated in 2001 and only began scaling up in 2003. For example, access to and use of voluntary counselling and testing (VCT) is very low. MDHS 2000 reported a demand for VCT in 81 percent of women and 87% for men, yet, VCT client levels reached a high of only 87 000 persons in 2002. Also, in 2003 less than 10% of primary and secondary schools reported having teachers who were both trained in and teaching life skills based HIV/AIDS education (Malawi National AIDS Commission, unpublished Monitoring and Evaluation data, 2004).
Conclusion
HIV prevalence among antenatal attendees has declined in several urban and semi‐urban areas, specifically in the central region. However there is possible evidence of an increasing trend in HIV prevalence in some rural areas, particularly in the northern region. Overall prevalence for ANC attendees aged 15–24 years aggregated from all sentinel sites has remained fairly stable from 1995 to 2003. Modelled incidence suggests a peak in 1992, a slight decline till 1997 and stable since then. Persistent levels of risky sexual behaviour in much of the population likely sustain HIV transmission and preclude a decline in the level of infections in the country.
Abbreviations
AIDS - acquired immune deficiency syndrome
ANC - antenatal clinic
MDHS - Malawi Demographic and Health Surveys
MKAPH - Malawi Knowledge, Attitudes, and Practices in Health Survey
HIV - human immunodeficiency virus
STI - sexually transmitted infection
VCT - voluntary counselling and testing
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Competing interests: none declared
References
- 1.National AIDS Commission Malawi national HIV/AIDS estimates 2003; Technical report. Malawi: NAC, January, 2004
- 2.National AIDS Commission HIV sentinel surveillance report 2003. Malawi: NAC, 2003
- 3.National Tuberculosis Control Program Report of a country‐wide survey of HIV/AIDS services in Malawi for year 2004. Malawi: NTP, MOH, 2005
- 4.MEASURE Evaluation AIDS in Africa during the Nineties: Malawi. A review and analysis of survey and research results. Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill, 2004
- 5.Joint United Nations Programme on AIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance Guidelines for conducting HIV sentinel serosurveys among pregnant women and other groups. Geneva: WHO, 2003
- 6.Ghys P D, Brown T, Grassly N C.et al The UNAIDS Estimation and Projection Package: a software package to estimate and project national HIV epidemics. Sex Transm Inf 200480(suppl 1)i5–i9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Statistics Office and Macro International Inc Malawi Demographic and Health Survey 1992, Malawi final report. Calverton, MD: Macro International Inc, 1994
- 8.National Statistics Office and Macro International Inc Malawi Knowledge, Attitudes, and Practices in Health Survey 1996, Malawi final report. Calverton, MD: Macro International Inc, 1997
- 9.National Statistics Office and Macro International Inc Malawi Demographic and Health Survey 2000, Malawi final report. Calverton, MD: Macro International Inc, 2001
- 10.National Statistics Office of Malawi 1998 Population and Housing Census. Zomba, Malawi 2000
- 11.Crimpin A C, Glynn J R, Ngwira B M.et al Trends and measurement of HIV prevalence in northern Malawi. AIDS 2003171817–1825. [DOI] [PubMed] [Google Scholar]