Abstract
Current efforts to develop a vaccine against human respiratory syncytial virus (HRSV) are focused on live attenuated strains. However, the unstable nature of HRSV is a major challenge for the preparation, storage and distribution of live vaccine candidates. We report here that the stability of HRSV can be improved by incorporation of the GP64 glycoprotein from baculovirus Autographa californica multiple nucleopolyhedrovirus. GP64 was incorporated in place of or in addition to the homologous HRSV glycoproteins and was either expressed from the HRSV genome or provided by propagating the virus in a Vero cell line constitutively expressing GP64 (Vbac cells). The infectivity of the different virus stocks was monitored after storage at 4°C, 22°C or 37°C, over a period of 8 weeks. The results showed that the infectivity of HRSV could be stabilized by up to 10,000 fold by the GP64 protein, when stored at 22°C for six weeks. This approach for stabilizing live HRSV may be important for vaccine development and may also prove useful for stabilizing other enveloped viruses.
Keywords: Stability, GP64 protein, Human respiratory syncytial virus
1. INTRODUCTION
Human respiratory syncytial virus is the main viral cause of severe respiratory tract disease in infants and children under two years of age [1,2] and a common cause of morbidity in the elderly and immunocompromised individuals [3,4]. Despite considerable work, there is no vaccine available. In the late 1960s, a vaccine trial using formalin-inactivated HRSV, resulted in enhanced disease after exposure to wild type virus [5,6]. Enhanced HRSV disease does not occur upon natural re-infection, which is a factor supporting the development of live attenuated vaccines. To date several candidates have been evaluated in clinical trials, but they were either under attenuated or over attenuated [7–9]. Achieving a balance between attenuation and immunogenicity has proven to be a formidable challenge. Another difficulty with regard to a live HRSV vaccine, is the unstable nature of the virus [10–12] and this may be a critical obstacle for distribution and storage of a future live vaccine. One approach to overcome these limitations has been to incorporate the HRSV F and G glycoproteins genes into related paramyxoviruses that have greater stability, such as human parainfluenza virus or Newcastle disease virus [13–15]. However, these vectored vaccines deliver only a subset of HRSV antigens and notably lack important CTL targets contained in the M2 and N proteins [16,17]. Whether these limitations affect efficacy and safety remains to be determined. In the present study we show an approach to improve the stability of HRSV to facilitate its use as a live virus vaccine and as a potential delivery vector.
Heterologous glycoproteins are able to complement enveloped viral particles by pseudotyping and this has been shown to provide increased stability for retroviruses and other gene therapy vectors [18–22]. The VSV envelope glycoprotein (G) has been used extensively for this purpose, but it has several drawbacks, including cytotoxicity [23]. In recent work, the major envelope glycoprotein GP64 of baculovirus Autographa californica multiple nucleopolyhedrovirus was shown to be a highly suitable protein for pseudotyping [23–25]. GP64 is a type I glycoprotein that contains both fusion and attachment functions in a single polypeptide [26,27]. Pseudotyping with GP64 permitted production of high titers of lentiviral particles [23]. The GP64 pseudotyped lentivirus also displayed wide tissue tropism and lacked the associated cytotoxic effects observed with VSV G. Previous studies from our laboratory showed that the authentic GP64 protein as well as a version in which its cytoplasmic tail was replaced with amino acids 563–574 from the carboxi-terminal region of the HRSV F protein (GP64/F), were incorporated into the membrane of HRSV. GP64 and GP64/F were able to mediate infectivity of the virus, since viruses containing these proteins as their only transmembrane glycoprotein were neutralized with GP64-specific antibodies. This finding also demonstrated that GP64 could substitute for both the attachment protein and fusion protein of HRSV [24]. Further, this initial work indicated that GP64 enhanced the stability of HRSV upon prolonged storage at 4°C [24].
In the present work we investigated the extent to which GP64 confers stability to HRSV. To do this we provided the baculovirus transmembrane glycoprotein in place of, or in addition to the three HRSV transmembrane glycoproteins: the small hydrophobic protein (SH), the attachment protein (G) and the fusion protein (F). Two different approaches were used to provide GP64 to HRSV. We used either an HRSV having the GP64/F gene engineered into its genome where it was expressed concomitantly with the other HRSV gene products, or alternatively HRSV was propagated in a Vero cell line that constitutively expressed GP64/F (Vbac). HRSV complemented with the GP64/F protein by growth in Vbac cells, incorporated the GP64/F protein into its membrane as was shown by immuno-electro microscopy using an anti-GP64 monoclonal antibody [25].
In the work reported here, we compared the stability of HRSVs having GP64 provided by each of these two methods after storage at different temperatures (4°, 22° or 37°C) for intervals up to two months.
2. MATERIALS AND METHODS
2.1. Cell lines and antibodies
Vero 76 (Vero) cells were acquired from the American Type Culture Collection (ATCC) and grown at 37°C in Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 5% fetal bovine serum (FBS), 200 mM L-Glutamine and antibiotics (Penicillin G, Kanamycin and Streptomycin).
Vero cells that constitutively express the baculovirus GP64 protein modified to carry the C-terminal half of the HRSV F protein cytoplasmic tail (residues 563–574) in place of its own cytoplasmic tail (GP64/F), were isolated and characterized previously and designated Vbac cells [25]. These cells were maintained at 33°C in DMEM containing 5% FBS, 1 mg/ml of G418 sulfate (Geneticin, Invitrogen) and 25 mM HEPES.
Monoclonal antibody 6 (MAb 6) specific for the HRSV N protein was provided by Geraldine Taylor (Institute for Animal Health, Compton, United Kingdom) and MAb AcV5 specific for the GP64 protein was provided by Gary Blissard (Boyce Thompson Institute at Cornell University, Ithaca, N.Y.).
2.2. Gene content of engineered viruses
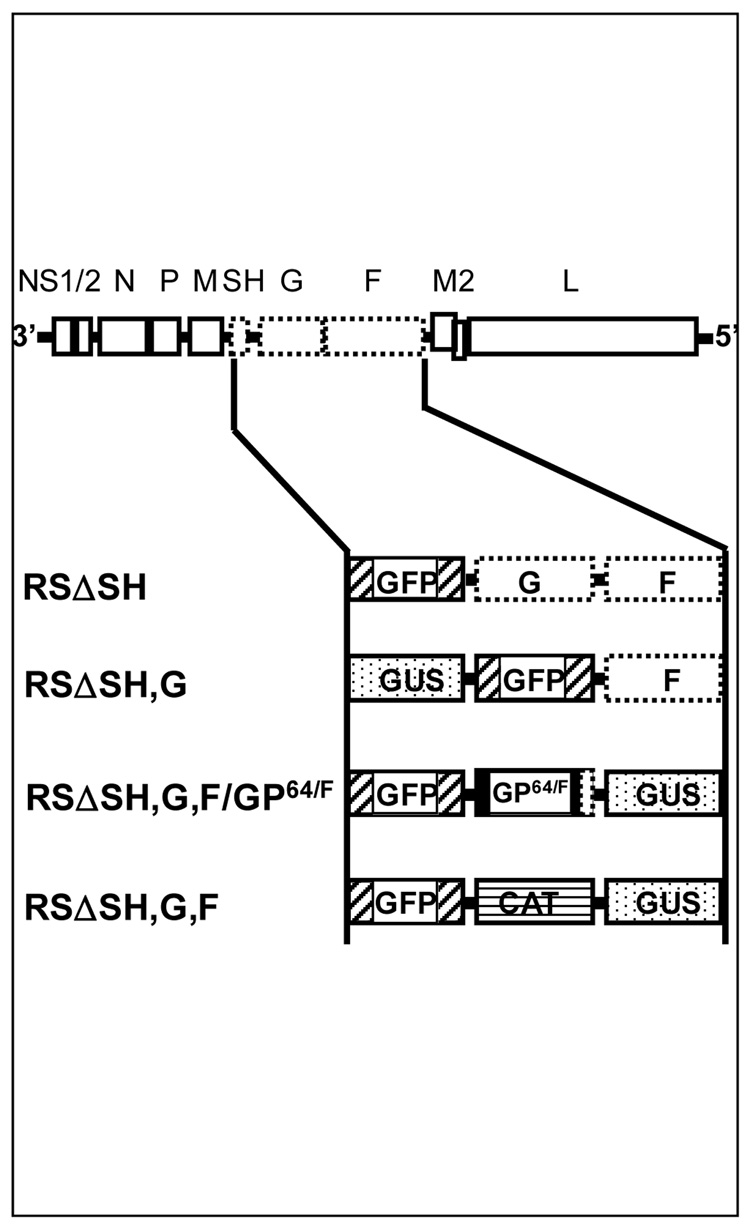
Several engineered HRSVs generated previously [24,28] and having a genome content as shown in Figure 1 were used for this study. Virus RSΔSH, a virus with the small hydrophobic (SH) protein open reading frame (ORF) deleted and replaced with that of the green fluorescent protein (GFP) has previously been shown to replicate in cell culture to similar levels as wild type HRSV [28]. To take advantage of the presence of GFP in the genome as a rapid marker of infectivity, we used the virus RSΔSH as a surrogate wild type virus. Virus RSΔSH,G,F/GP64/F, is a virus having all three HRSV transmembrane glycoproteins (SH, G and F) ORFs deleted and replaced with those of GFP, GP64/F and β-glucuronidase (GUS) respectively. Next, virus RSΔSH,G,F, is a virus having all three HRSV glycoproteins deleted and replaced with GFP, chloramphenicol acetyltransferase (CAT) and GUS respectively.
Figure 1.
Gene content of the engineered cDNAs. All engineered viruses were generated from a cDNA of the A2 strain of HRSV. Virus RSΔSH has the SH ORF deleted and replaced with that of GFP. Virus RSΔSH,G has the SH and G ORFs deleted and replaced with ORFs encoding marker proteins GUS and GFP. Virus RSΔSH,G,F/GP64/F has the SH, G and F ORFs deleted and replaced with the ORF of GP64/F along with ORFs encoding GFP and GUS. Finally, virus RSΔSH,G,F has the ORFs encoding the three HSRV glycoproteins replaced with that of reporter genes GFP, CAT and GUS.
Virus RSΔSH,G was generated and recovered for these studies. In this virus, the SH and G proteins ORFs were deleted and replaced with those of GUS and GFP surrounded by authentic HRSV transcription signals, while the wild type F gene of HRSV was maintained intact. Since the gene position relative to the 3’ promoter is important for control of gene expression in negative strand RNA viruses, the number of genes and gene junctions within all the engineered viruses was kept the same as in the wild type virus [29].
All engineered cDNAs were based on the A2 strain of HRSV and were constructed as previously described [28]. To generate the cDNA for virus RSΔSH,G, a shuttle vector containing the ORFs encoding GUS, GFP and HRSV F proteins and flanked by FseI and AscI restriction sites, was constructed. This FseI/AscI fragment was cloned into the A2 cDNA backbone that lacked SH, G and F ORFs and which contained the same restriction sites. To recover infectious virus, each of the engineered cDNAs was transfected into HEp-2 cells previously infected with modified vaccinia virus Ankara T7 [30] along with plasmids encoding each of the proteins required for viral transcription and replication (nucleocapsid (N) protein, phosphoprotein (P), polymerase (L) and M2-1 transcription factor), and a plasmid encoding the VSV G protein carrying the HRSV F protein cytoplasmic tail (VSV-GRS-F), using lipofectin (Invitrogen) as described previously [31]. Virus was collected from the supernatants at 2–3 days post transfection and amplified by passage in Vero cells. The genomes of engineered virus stocks were verified by RT-PCR and sequence analysis of the cloned regions. Passage 4 stocks were used for the experiments described.
2.3. Preparation of virus stocks and storage
Virus stocks for each of the engineered viruses were generated as previously described [24]. Briefly, Vero or Vbac cells were infected at low multiplicity (0.01–0.1) and stocks were harvested 6 days post infection by scraping cells into the supernatant, followed by gentle but extensive pipetting and removal of the cell debris by centrifugation at 750 × g for 4 minutes in a Sorvall RT6000B centrifuge. Stocks were divided into 100 µl aliquots and 25 tubes of each stock were stored at each of the indicated temperatures (4°C, 22°C and 37°C), always protected from light. Virus RSΔSH,G,F could only be propagated on Vbac cells, since this virus lacked all three HRSV glycoproteins.
2.4. Titration of virus stocks
Titers of all engineered virus stocks were determined in triplicate immediately after harvest (time zero) and at the indicated time intervals by a 50% tissue culture infective dose (TCID50) assay, as described previously [28]. Briefly, 10 fold serial dilutions of each virus were used to infect 3.5 × 103 Vero cells (3 × 103 Vbac cells for virus RSΔSH,G,F) in 96-well plates and incubated for eight days at 33°C. Since all of the engineered viruses contained the GFP gene, wells positive for viral infection were detected using a fluorescence microscope. Expression of GFP was previously shown to be a stable and accurate indicator of infectivity, that correlated with the number of plaque-forming units (PFU) [28]. The remaining infectivity at different time intervals was expressed as the percentage of the titer at time zero for the corresponding virus.
2.5. Concentration and partial purification of virus
Vero or Vbac cells were infected at low multiplicity with virus RSΔSH,G,F/GP64/F or RSΔSH,G,F respectively, and incubated at 33°C in DMEM supplemented with 3% FBS. Three days post-infection this medium was replaced with DMEM without FBS (VP-SFM, Invitrogen). Infected cells were then incubated for one more day and then the viruses were harvested from the supernatant. After low speed centrifugation (750 × g for 4 min) to remove cell debris, the supernatant was centrifuged in an AH-629 rotor at 20,000 × g for 30 minutes at 4°C. The pellet was resuspended in PBS and frozen at −80°C for further use. Mock infected Vero and Vbac cells treated in the same way were used as control antigens.
2.6. Detection of GP64 by ELISA and Western Blot
The GP64 protein was detected and quantitated by ELISA and Western Blot. For ELISA, viruses RSΔSH,G,F/GP64/F and RSΔSH,G,F (prepared as described above in section 2.5) were diluted in PBS and used to coat a 96-well microtiter plate. After overnight incubation at 4°C, the viruses were fixed with 80% acetone in PBS for 15 min at 4°C and then treated with 0.02% Triton X-100 in PBS. Wells were blocked for 30 min with 1% BSA in PBS. Monoclonal antibodies against N (MAb 6) and GP64 (AcV5) proteins, diluted in 0.1% BSA in PBS were added to the wells and incubated for 1 hour at room temperature. After washing with PBS, bound antibodies were detected via incubation with peroxidase-labelled anti mouse immunoglobulin and OPD as substrate, following the manufacturer’s instructions (Sigma-Aldrich). Mock infected Vero and Vbac cells were treated the same way as the isolated viruses and used as a control antigen.
Western Blot analysis was carried out by electrophoresing virus preparations on a 10% sodium dodecyl sulfate-polyacrylamide gel (SDS-PAGE) under reducing conditions. Detection of the proteins was followed by immunoblot using an anti-GP64 monoclonal antibody (AcV5) and a goat anti-mouse immunoglobulin conjugated with an infrared fluorophore (Alexa Fluor® 680, Molecular Probes, Eugene, OR) as a secondary antibody. Specific bands were visualized using the Odyssey Infrared Imaging System (LI-COR Biosciences).
3. RESULTS
3.1. GP64 expressed from the viral genome provides enhanced stability to glycoprotein deleted HRSV at 4°C, 22°C and 37°C
The unstable nature of HRSV is a significant problem for both basic research and the development of potential live vaccines. Although the cause of this instability is unknown, we previously reported that the instability of HRSV appeared to be associated with the attachment protein, G and/or the fusion protein F, as viruses lacking the genes for these two proteins and containing instead the baculovirus entry/exit protein (GP64) were significantly more stable than wild type HRSV upon storage at 4°C [24]. Moreover these viruses were infectious, indicating that GP64 could promote entry and exit of HRSV [24].
In the present work we extended these studies to examine whether GP64 when expressed from the viral genome in place of the HRSV glycoprotein genes, was able to impart stability for long periods of time not only at 4°C, but also at 22 °C and 37°C.
We first compared the stability of a virus having GP64 in place of all three authentic HRSV glycoproteins, with that of a virus having the homologous HRSV attachment and fusion proteins. The glycoprotein deleted HRSV had the SH, G and F ORFs deleted and replaced with those of GFP, the GP64 protein having the F protein cytoplasmic tail engineered into it (GP64/F) and GUS respectively. The three deleted genes were replaced in order to maintain the same number of transcriptional units in the viral genome. This virus was termed RSΔSH,G,F/GP64/F (Figure 1). The virus used for comparison was an HRSV having the authentic G and F genes, but having the SH protein ORF deleted and replaced with that of GFP, termed RSΔSH (Figure 1). Previous work showed that the growth characteristics and stability of RSΔSH at 4°C was similar to that of wild type A2 strain of HRSV in cell culture [24] and RSΔSH therefore was used as a surrogate wild type virus for these experiments. Stocks of virus RSΔSH and RSΔSH,G,F/GP64/F were prepared in Vero cells and identical, replicate aliquots of each stock were stored at 4°C and 22°C as described in Materials and Methods. The infectivity of triplicate samples of these viruses was measured by TCID50 at 1-week intervals over a period of 8 weeks and compared with titers determined at time zero.
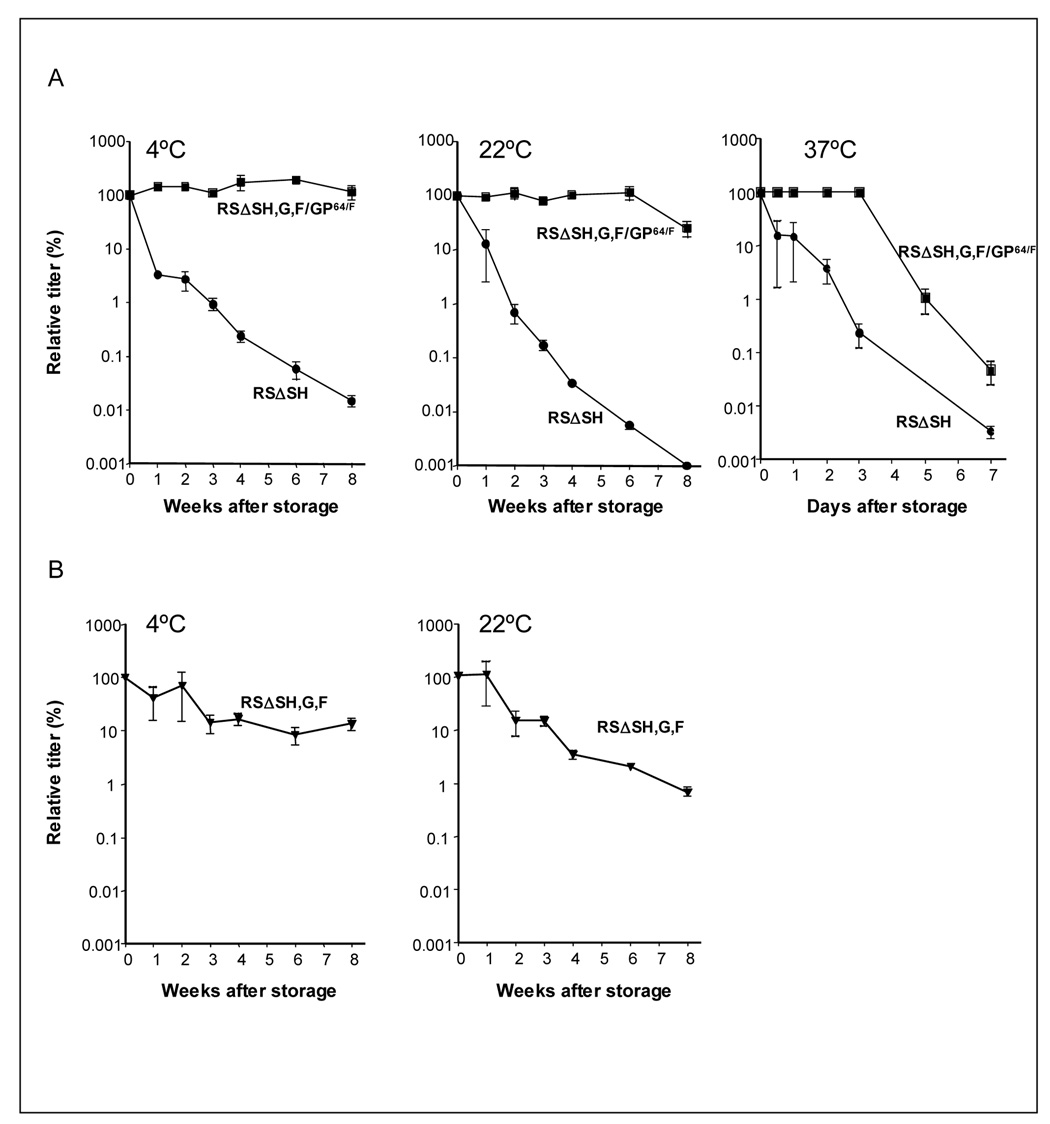
The results in Figure 2A (4°C) showed that infectivity of virus RSΔSH,G,F/GP64/F, which had all three HRSV glycoprotein genes deleted and replaced with GP64/F, was stable upon storage at 4°C and suffered no decrease in titer over an eight week period. In contrast, the titer of RSΔSH virus declined rapidly and was 10,000 times lower than the titer of the virus RSΔSH,G,F/GP64/F after eight weeks at 4°C. These data confirm and extend the results published previously by our laboratory [24]. When stability was examined at room temperature (Figure 2A, 22°C), the virus expressing GP64/F as its only viral transmembrane glycoprotein showed no loss of infectivity during six weeks of storage. Even after eight weeks of storage, the infectivity of virus RSΔSH,G,F/GP64/F was 10,000 fold higher than that of the surrogate wild type HRSV (RSΔSH), which had little remaining infectivity.
Figure 2.
Stabilizing effect of GP64 on HRSV lacking its homologous transmembrane glycoproteins. (A) Stability of virus having the GP64/F gene added to its genome (RSΔSH,G,F/GP64/F) and (B) stability of virus having the GP64/F protein provided by complementation from Vbac cells (RSΔSH,G,F). Stocks of viruses RSΔSH and RSΔSH,G,F/GP64/F were generated in Vero cells (A) and stocks of virus RSΔSH,G,F were prepared in Vbac cells (B), and then stored at 4°C , 22°C or 37°C. Titers were determined by TCID50 over different time intervals as indicated on the graphs and compared with the titers from the day of harvest. Infectivity was plotted as a percentage of the TCID50 at the start of the experiment (time 0). Error bars represent standard deviations from the mean of triplicate samples.
We next examined the stability of the GP64-containing virus when stored at higher temperature, 37°C. As before, stocks of viruses RSΔSH and RSΔSH,G,F/GP64/F were generated from Vero cells and equal aliquots of each were stored at 37°C. In this case, neither virus was stable over a period of weeks (data not shown). In place of weekly intervals, the remaining infectivity was measured at 12h, 24h, 2, 3, 5 and 7 days. The data show that the titer of both viruses decreased rapidly upon storage at 37°C. However, in contrast to the control virus RSΔSH, the infectivity of the virus containing GP64/F remained undiminished during the first three days of storage at 37°C before starting to decline (Figure 2A, 37°C). These results show that the stability of HRSV was substantially increased in the presence of the GP64 glycoprotein, not only upon storage at 4°C but also at higher temperatures.
3.2. Stability imparted by GP64 provided in trans by the complementing cell line, Vbac
We next examined the stabilizing effect of GP64 on HRSV, when GP64 was provided by propagating viruses in a cell line (Vbac) that constitutively expresses the GP64/F protein [25]. The Vbac cells were generated to provide a method to complement lethal mutations in the HRSV transmembrane glycoproteins in order to study the roles of these proteins in HRSV infectivity, and in previous work we showed that these cells effectively support replication of HRSV lacking all transmembrane glycoprotein genes [25,32].
In the present study, we used these cells to test whether providing the GP64 protein to HRSV by complementation in trans could also impart increased stability to virions. Stocks of virus lacking all three HRSV glycoproteins (RSΔSH,G,F) were prepared in Vbac cells and stored at 4°C and 22°C. The stability of infectivity after storage was measured by TCID50 at weekly intervals over an eight week period. The stability of HRSV infectivity was greatly improved at both 4°C and 22°C when GP64/F was provided from the complementing cell line (Figure 2B). The improvement was not as great as seen in Figure 2A, where GP64/F was expressed from the viral genome. Nevertheless, the stability of virus that acquired GP64/F by complementation from Vbac cells was 1,000 fold higher after eight weeks of storage at either 4 or 22°C than the surrogate wild type virus grown in Vero cells, RSΔSH (Compare Figure 2A and 2B). From these results we conclude that GP64 can provide enhanced stability to HRSV, not only when expressed from the viral genome, but also when it is provided by propagating the virus in the complementing cell line, Vbac.
3.3. Analysis of GP64 in virions
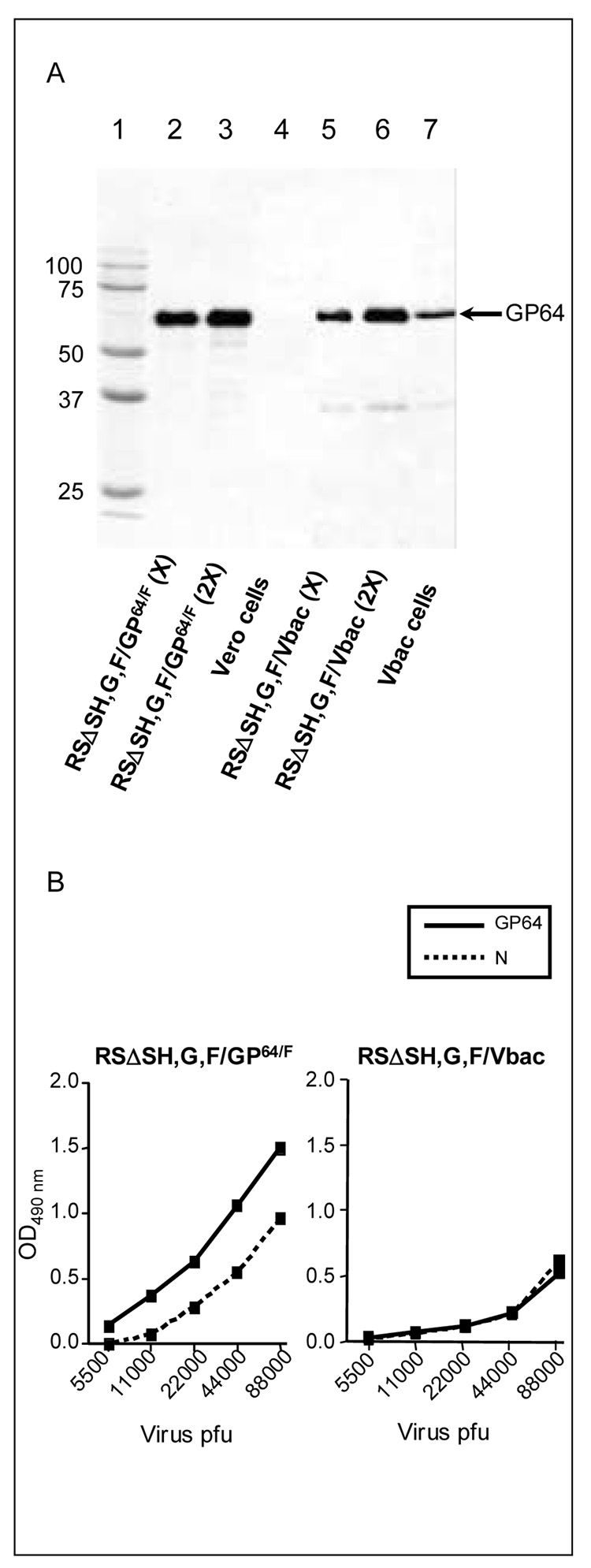
The difference in stability between the viruses having GP64 expressed from the genome (RSΔSH,G,F/GP64/F) or provided by complementation (RSΔSH,G,F grown in Vbac cells) was surprising, given that both had GP64/F as their only transmembrane glycoprotein. To investigate this difference in stability of viruses having GP64 provided by the two different methods, we analyzed the level of GP64 protein present in virions. Viruses with GP64 protein provided by complementation in cis or trans were isolated as described in Materials and Methods by ultracentrifugation from the supernatant fluids of infected cells. First, the presence and integrity of the GP64/F protein in the virions (virus RSΔSH,G,F/GP64/F and virus RSΔSH,G,F) was confirmed by Western Blot, using a monoclonal antibody to GP64, AcV5 [33,34]. An approximately 64 kDa band corresponding to the GP64/F protein was detected in viruses RSΔSH,G,F/GP64/F and RSΔSH,G,F (Figure 3A, lanes 2–3 and 5–6, respectively) and uninfected Vbac cells (Figure 3A, lane 7), but not in uninfected Vero cells (Figure 3A, lane 4).
Figure 3.
(A) Western Blot analysis of GP64 protein from isolated viruses and uninfected cells. Lane 1 shows the molecular weight markers. Lanes 2 and 3 correspond to virus RSΔSH,G,F/GP64/F; lane 3 contains double (2X) the amount of lane 2 (X). Lanes 5 and 6 correspond to virus RSΔSH,G,F; lane 6 contains double (2X) the amount of lane 5 (X). Lanes 4 and 7 show uninfected Vero and Vbac cells, respectively. The location of GP64, as determined by incubation with monoclonal antibody AcV5, is indicated with an arrow. (B) Comparison of GP64 levels in virions where GP64/F is expressed from the genome (RSΔSH,G,F/GP64/F) or where GP64/F is acquired by complementation (RSΔSH,G,F). Viruses were prepared from infected cells (Vero and Vbac respectively) as described in Materials and Methods, and the titer of each stock was determined by plaque assay. Relative GP64 and N levels of the isolated viruses were then determined simultaneously by ELISA using monoclonal antibodies (AcV5 and MAb 6, respectively) and plotted against the number of plaque-forming units (pfu).
To determine whether there was a difference in the quantity of GP64 protein between the two viruses, we measured the amount of GP64/F protein in each virus preparation relative to the viral nucleoprotein (N). Similar amounts of each virus, based on PFU, were coated onto 96 well plates and examined by ELISA. The results in Figure 3B show that virus RSΔSH,G,F/GP64/F had a higher amount of GP64/F protein relative to N than virus RSΔSH,G,F grown in Vbac cells, suggesting that the former virus contained more GP64/F protein per particle. The higher amount of GP64/F may contribute to the difference observed in thermostability between the two viruses.
3.4. Stability provided by GP64 to HRSV containing its homologous membrane glycoprotein genes
We next investigated whether addition of the GP64/F protein could provide enhanced stability to HRSV carrying its own F and G proteins, since these antigens are the main target of neutralizing antibodies against HRSV in experimental animal models as well as in humans [35–38].
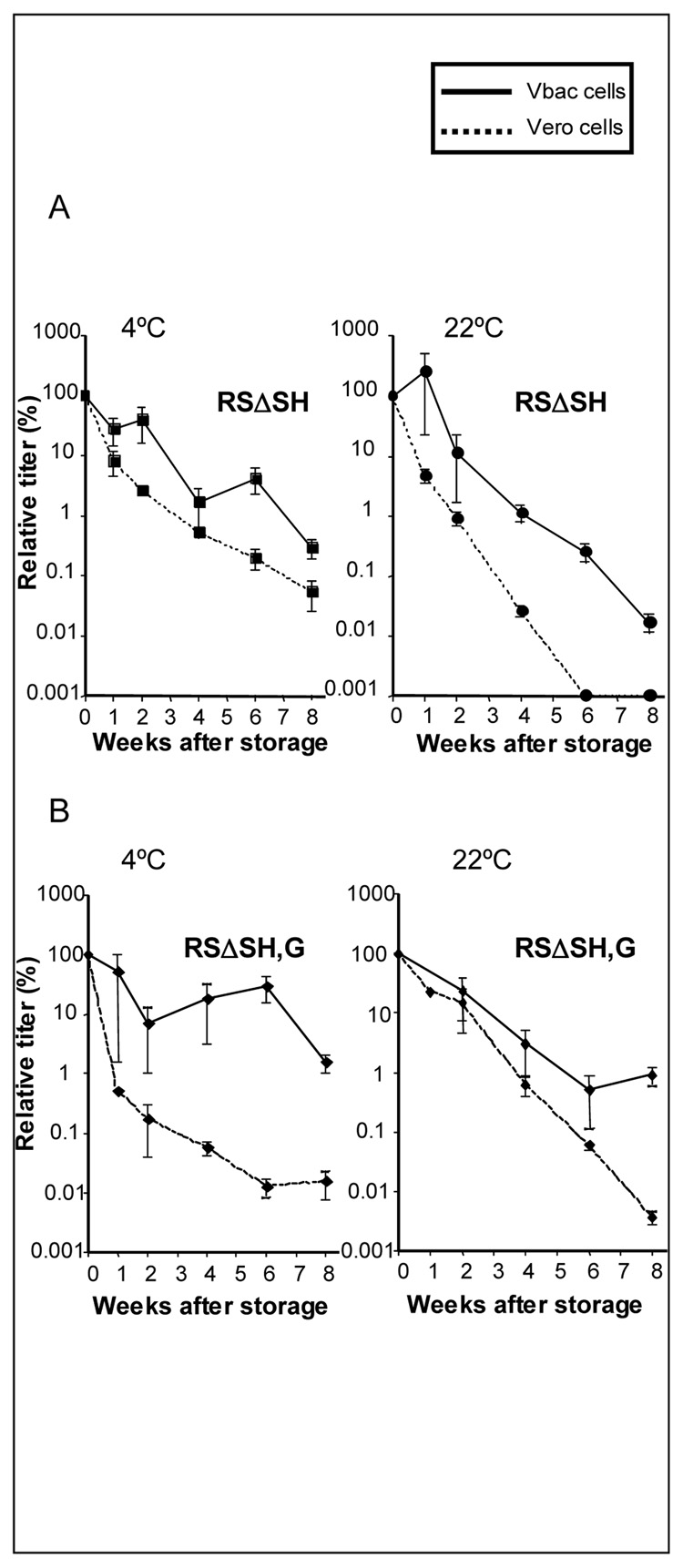
Stocks of virus RSΔSH, containing the F and G genes, were prepared by propagating the virus in either Vero or Vbac cells. The stability of the resulting viruses was compared after storage at 4°C or 22°C by measuring infectivity weekly over a period of 8 weeks. The data in Figure 4A show that the stability of RSΔSH was 10–100 fold higher either at 4°C or 22°C when propagated in the Vbac cells expressing GP64/F than when propagated in Vero cells. This level of increased stability provided by GP64/F was modest but consistent, and showed that the addition of the GP64/F protein by complementation of HRSV containing its own F and G proteins also increased virus stability.
Figure 4.
Comparison of the stability of HRSV cointaining F and G proteins (A) or F alone (B), when grown in Vbac cells versus Vero cells. Vero ( ) and Vbac (
) and Vbac ( ) cells were infected with virus RSΔSH (A) or RSΔSH,G (B) and stocks were generated. Aliquots of both viruses were stored at 4°C or 22°C and titers were determined by TCID50 at 1-week intervals over a period of 8 weeks.
) cells were infected with virus RSΔSH (A) or RSΔSH,G (B) and stocks were generated. Aliquots of both viruses were stored at 4°C or 22°C and titers were determined by TCID50 at 1-week intervals over a period of 8 weeks.
Of the three HRSV glycoproteins, F is the most critical for infectivity and therefore an important target of the immune response. Thus, we next tested the ability of GP64 to provide enhanced stability to a virus carrying the F protein as its only homologous glycoprotein (RSΔSH,G). Stocks of this virus were prepared by propagation in Vero or Vbac cells and their stability compared after storage at 4 or 22°C. A 100–1000 fold increase in stability was observed at 4°C when the virus RSΔSH,G was propagated in Vbac cells as compared to Vero cells (Figure 4B, 4°C). At 22°C, the increase in stability was approximately 10 fold, which was more modest than the stabilizing effect seen at 4°C (Figure 4B, 22°C). However, the results of Figure 4A and 4B show that the stability of HRSV containing GP64/F in addition to the F protein alone or both the F and G proteins was significantly improved.
4. DISCUSSION
Respiratory syncytial virus is a highly labile virus that loses substantial infectivity upon storage, even at temperatures below zero [10–12]. The instability of the virus is a serious hurdle for basic research as well as for vaccine development; especially since research to develop a pediatric HRSV vaccine has recently been focused on live attenuated strains. A number of compounds such as inorganic salts, some sugars and proteins have previously been added to the culture medium in order to increase the stability of HRSV and other viruses. For instance, MgSO4, sucrose or sorbitol helped stabilize the infectivity of viruses such as measles and HRSV for periods of 3 to 4 months at 4°C and temperatures below zero [10,11,39]. Influenza vaccine liquid formulation can be stored frozen at −20°C for a year in the presence of sucrose and for at least twenty days at 4°C by addition of deuterium oxide (D2O) [40,41]. Lyophilized formulations of measles and influenza can usually be stored long term at higher temperatures, although they need to be used as soon as possible after reconstitution [42,43]. Non enveloped viruses such as adenoviruses and polioviruses can be stabilized for longer periods of time at high temperatures such as 37°C and 45°C [39,44,45]. MgCl2 is used as a stabilizer for the oral poliovirus vaccine [39]. Such stabilized vaccine can be kept for 28 months at 2–8°C, for six weeks at 25°C and for three days at 37°C, with no loss of titer or immunogenicity. It is generally considered that enveloped viruses are more labile and susceptible to heat inactivation and therefore more difficult to stabilize than non-enveloped viruses, suggesting that the lipid bilayer is a major factor of virus instability. The aim of this study was to characterize the extent to which the stability of HRSV, a notoriously unstable enveloped virus, could be improved by incorporating a heterologous protein, the baculovirus membrane glycoprotein, GP64. The budded virus phenotype of baculovirus AcMNPV, of which GP64 is the major envelope glycoprotein, is a highly stable insect virus that can be stored at 4°C for more than a year without loss of infectivity, if protected from light [46].
We used two different approaches to pseudotype HRSV with GP64. First, we used an HRSV that had the GP64/F gene engineered into its genome, from which the homologous HRSV glycoproteins (SH, G and F) had been removed. This led to a substantial increase in stability as shown in Figure 2A. The infectivity of this virus was completely stable for at least two months upon storage at 4°C, for up to six weeks at 22°C and for three days at 37°C. These results indicate that, surprisingly, the viral nucleocapsid and the RNA dependent RNA polymerase are stable at room temperature for over 6 weeks and also suggest that the instability of HRSV is most likely associated with the viral glycoproteins and not the lipid envelope per se. Little is known about thermostability of the HRSV F and G proteins; one study suggested that the conformation of purified F protein and F protein in virus was not altered after brief exposure to high temperatures as indicated by circular dichroism and antibody binding [47]. However, infectivity of the virus after high temperature treatment was not examined.
In addition to providing GP64/F to HRSV by expressing it from the viral genome, we propagated the virus in Vbac cells that constitutively express GP64/F to complement the virus in trans. Virus RSΔSH,G,F complemented in this manner, also showed a significant improvement in stability when compared to the surrogate wild type virus ΔSH grown in Vero cells at 4°C and 22°C (Figures 2A and 2B). Moreover, this second approach of providing GP64 to HRSV may represent an advantage in terms of vaccine safety, since the GP64/F provided from the cell line is degraded after entry and no additional GP64/F would be expressed from the genome as when provided in cis. Therefore, viruses containing no other functional glycoproteins would be unable to spread after the first round of infection. Thus, this approach provides a live viral vector for delivery, but in a virus where infectivity will not progress. As was mentioned in the introduction, GP64 has been used to pseudotype viral particles for gene therapy purposes due to its wide tissue tropism. For HRSV vaccine development this may be not beneficial, since the disease is primarily respiratory. To address this question we are currently investigating the targeting in vivo of HRSV having GP64 in its membrane as compared to wild type virus.
The improvement in stability provided by GP64 protein to viruses lacking all three glycoproteins, was greater when GP64 was expressed from the viral genome (RSΔSH,G,F/GP64/F) than when it was provided via the cell line (i.e. virus RSΔSH,G,F grown in Vbac). Analysis of GP64 protein from these viruses by Western Blot revealed that the molecular weight and integrity of the protein in both cases was as expected. However, quantitation by ELISA showed that virus expressing GP64/F from the viral genome had higher amounts of GP64 protein per amount of viral nucleocapsid protein (Figure 3). The different amounts of GP64/F incorporated into virions prepared by the two methods may explain the different degrees of added stability; however this needs to be examined in more detail.
Since the F and G proteins are important protective viral antigens, we also examined the stability of an HRSV that retained its homologous membrane glycoproteins, F and G, when GP64/F was provided in trans. While titers of virus RSΔSH not supplemented with GP64 (grown in standard Vero cells) decreased significantly after storage, the same virus propagated in the GP64/F complementing Vbac cells was 10–100 times more stable at 4°C and 22°C, respectively (Figure 4A). The same was true for a virus carrying F as its only homologous glycoprotein (RSΔSH,G). After storage at 4°C or 22°C the infectivity of virus RSΔSH,G containing GP64/F by being propagated in Vbac cells was 100–1000 greater than when the same virus was grown in Vero cells (Figure 4B). Thus, GP64 can improve the stability of HRSV even in the presence of its homologous viral proteins, F and G. However, none of the above viruses (RSΔSH and RSΔSH,G) showed an improvement in stability as great as that achieved when the virus lacked all the three homologous viral glycoproteins. Possible explanations for this are that the presence of the G and/or F protein may impart instability regardless of the presence or absence of GP64, or that there is competition for incorporation into the membrane between GP64 carrying the F cytoplasmic tail and the homologous HRSV glycoproteins. Viruses RSΔSH and RSΔSH,G are the most interesting from a vaccine point of view since they retain the principal immunogens of the virus, the F and G proteins. Therefore, our next aim is to examine whether the presence of GP64 in the membrane of these viruses affect the immunogenicity of HRSV in vivo.
In conclusion, these findings demonstrate the potential of the GP64 protein as a stabilizer of HRSV. The ability to stabilize these viruses represents a significant advantage both for the use of the virus in the laboratory and for maintenance and transport of potential live vaccines against HRSV, in particular in cases where cold-chain infrastructure is lacking. Furthermore, this approach may well prove to be applicable for stabilizing other labile enveloped viruses of medical importance.
ACKNOWLEDGMENTS
We thank the members of the Wertz laboratory for helpful discussions during the preparation of the manuscript.
This work was supported by Public Health Service grant AI20181 to G.W.W. from the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Henderson FW, Collier AM, Clyde WA, Jr, Denny FW. Respiratory-syncytial-virus infections, reinfections and immunity. A prospective, longitudinal study in young children. N Engl J Med. 1979;300(10):530–534. doi: 10.1056/NEJM197903083001004. [DOI] [PubMed] [Google Scholar]
- 2.Glezen WP, Taber LH, Frank AL, Kasel JA. Risk of primary infection and reinfection with respiratory syncytial virus. Am J Dis Child. 1986;140(6):543–546. doi: 10.1001/archpedi.1986.02140200053026. [DOI] [PubMed] [Google Scholar]
- 3.Englund JA, Anderson LJ, Rhame FS. Nosocomial transmission of respiratory syncytial virus in immunocompromised adults. J Clin Microbiol. 1991;29(1):115–119. doi: 10.1128/jcm.29.1.115-119.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Falsey AR, McCann RM, Hall WJ, et al. Acute respiratory tract infection in daycare centers for older persons. J Am Geriatr Soc. 1995;43(1):30–36. doi: 10.1111/j.1532-5415.1995.tb06238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim HW, Canchola JG, Brandt CD, et al. Respiratory syncytial virus disease in infants despite prior administration of antigenic inactivated vaccine. Am J Epidemiol. 1969;89(4):422–434. doi: 10.1093/oxfordjournals.aje.a120955. [DOI] [PubMed] [Google Scholar]
- 6.Kapikian AZ, Mitchell RH, Chanock RM, Shvedoff RA, Stewart CE. An epidemiologic study of altered clinical reactivity to respiratory syncytial (RS) virus infection in children previously vaccinated with an inactivated RS virus vaccine. Am J Epidemiol. 1969;89(4):405–421. doi: 10.1093/oxfordjournals.aje.a120954. [DOI] [PubMed] [Google Scholar]
- 7.Karron RA, Ambrosino DM. Respiratory syncytial virus vaccines. Pediatr Infect Dis J. 1998;17(10):919–920. doi: 10.1097/00006454-199810000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Wright PF, Belshe RB, Kim HW, Van Voris LP, Chanock RM. Administration of a highly attenuated, live respiratory syncytial virus vaccine to adults and children. Infect Immun. 1982;37(1):397–400. doi: 10.1128/iai.37.1.397-400.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wright PF, Karron RA, Belshe RB, et al. Evaluation of a live, cold-passaged, temperature-sensitive, respiratory syncytial virus vaccine candidate in infancy. J Infect Dis. 2000;182(5):1331–1342. doi: 10.1086/315859. [DOI] [PubMed] [Google Scholar]
- 10.Fernie BF, Gerin JL. The stabilization and purification of respiratory syncytial virus using MgSO4. Virology. 1980;106(1):141–144. doi: 10.1016/0042-6822(80)90229-9. [DOI] [PubMed] [Google Scholar]
- 11.Gupta CK, Leszczynski J, Gupta RK, Siber GR. Stabilization of respiratory syncytial virus (RSV) against thermal inactivation and freeze-thaw cycles for development and control of RSV vaccines and immune globulin. Vaccine. 1996;14(15):1417–1420. doi: 10.1016/s0264-410x(96)00096-5. [DOI] [PubMed] [Google Scholar]
- 12.Hambling MH. Survival Of The Respiratory Syncytial Virus During Storage Under Various Conditions. Br J Exp Pathol. 1964;45:647–655. [PMC free article] [PubMed] [Google Scholar]
- 13.Collins PL, Murphy BR. New generation live vaccines against human respiratory syncytial virus designed by reverse genetics. Proc Am Thorac Soc. 2005;2(2):166–173. doi: 10.1513/pats.200501-011AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schmidt AC, Wenzke DR, McAuliffe JM, et al. Mucosal immunization of rhesus monkeys against respiratory syncytial virus subgroups A and B and human parainfluenza virus type 3 by using a live cDNA-derived vaccine based on a host range-attenuated bovine parainfluenza virus type 3 vector backbone. J Virol. 2002;76(3):1089–1099. doi: 10.1128/JVI.76.3.1089-1099.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez-Sobrido L, Gitiban N, Fernandez-Sesma A, et al. Protection against respiratory syncytial virus by a recombinant Newcastle disease virus vector. J Virol. 2006;80(3):1130–1139. doi: 10.1128/JVI.80.3.1130-1139.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bangham CR, Openshaw PJ, Ball LA, King AM, Wertz GW, Askonas BA. Human and murine cytotoxic T cells specific to respiratory syncytial virus recognize the viral nucleoprotein (N), but not the major glycoprotein (G), expressed by vaccinia virus recombinants. J Immunol. 1986;137(12):3973–3977. [PubMed] [Google Scholar]
- 17.Openshaw PJ, Anderson K, Wertz GW, Askonas BA. The 22,000-kilodalton protein of respiratory syncytial virus is a major target for Kd-restricted cytotoxic T lymphocytes from mice primed by infection. J Virol. 1990;64(4):1683–1689. doi: 10.1128/jvi.64.4.1683-1689.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guibinga GH, Friedmann T. Baculovirus GP64-pseudotyped HIV-based lentivirus vectors are stabilized against complement inactivation by codisplay of decay accelerating factor (DAF) or of a GP64-DAF fusion protein. Mol Ther. 2005;11(4):645–651. doi: 10.1016/j.ymthe.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Kang Y, Xie L, Tran DT, et al. Persistent expression of factor VIII in vivo following nonprimate lentiviral gene transfer. Blood. 2005;106(5):1552–1558. doi: 10.1182/blood-2004-11-4358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sinn PL, Burnight ER, Hickey MA, Blissard GW, McCray PB., Jr Persistent gene expression in mouse nasal epithelia following feline immunodeficiency virus-based vector gene transfer. J Virol. 2005;79(20):12818–12827. doi: 10.1128/JVI.79.20.12818-12827.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang Y, Vanin EF, Whitt MA, et al. Inducible, high-level production of infectious murine leukemia retroviral vector particles pseudotyped with vesicular stomatitis virus G envelope protein. Hum Gene Ther. 1995;6(9):1203–1213. doi: 10.1089/hum.1995.6.9-1203. [DOI] [PubMed] [Google Scholar]
- 22.Emi N, Friedmann T, Yee JK. Pseudotype formation of murine leukemia virus with the G protein of vesicular stomatitis virus. J Virol. 1991;65(3):1202–1207. doi: 10.1128/jvi.65.3.1202-1207.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumar M, Bradow BP, Zimmerberg J. Large-scale production of pseudotyped lentiviral vectors using baculovirus GP64. Hum Gene Ther. 2003;14(1):67–77. doi: 10.1089/10430340360464723. [DOI] [PubMed] [Google Scholar]
- 24.Oomens AG, Wertz GW. The baculovirus GP64 protein mediates highly stable infectivity of a human respiratory syncytial virus lacking its homologous transmembrane glycoproteins. J Virol. 2004;78(1):124–135. doi: 10.1128/JVI.78.1.124-135.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oomens AG, Wertz GW. trans-Complementation allows recovery of human respiratory syncytial viruses that are infectious but deficient in cell-to-cell transmission. J Virol. 2004;78(17):9064–9072. doi: 10.1128/JVI.78.17.9064-9072.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blissard GW, Wenz JR. Baculovirus gp64 envelope glycoprotein is sufficient to mediate pH-dependent membrane fusion. J Virol. 1992;66(11):6829–6835. doi: 10.1128/jvi.66.11.6829-6835.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hefferon KL, Oomens AG, Monsma SA, Finnerty CM, Blissard GW. Host cell receptor binding by baculovirus GP64 and kinetics of virion entry. Virology. 1999;258(2):455–468. doi: 10.1006/viro.1999.9758. [DOI] [PubMed] [Google Scholar]
- 28.Oomens AG, Megaw AG, Wertz GW. Infectivity of a human respiratory syncytial virus lacking the SH, G, and F proteins is efficiently mediated by the vesicular stomatitis virus G protein. J Virol. 2003;77(6):3785–3798. doi: 10.1128/JVI.77.6.3785-3798.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wertz GW, Perepelitsa VP, Ball LA. Gene rearrangement attenuates expression and lethality of a nonsegmented negative strand RNA virus. Proc Natl Acad Sci U S A. 1998;95(7):3501–3506. doi: 10.1073/pnas.95.7.3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wyatt LS, Moss B, Rozenblatt S. Replication-deficient vaccinia virus encoding bacteriophage T7 RNA polymerase for transient gene expression in mammalian cells. Virology. 1995;210(1):202–205. doi: 10.1006/viro.1995.1332. [DOI] [PubMed] [Google Scholar]
- 31.Hardy RW, Harmon SB, Wertz GW. Diverse gene junctions of respiratory syncytial virus modulate the efficiency of transcription termination and respond differently to M2-mediated antitermination. J Virol. 1999;73(1):170–176. doi: 10.1128/jvi.73.1.170-176.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oomens AG, Bevis KP, Wertz GW. The Cytoplasmic Tail of the Human Respiratory Syncytial Virus F Protein Plays a Critical Role in Cellular Localization of the F Protein and Infectious Progeny Production. J Virol. 2006 doi: 10.1128/JVI.01439-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blissard GW, Rohrmann GF. Location, sequence, transcriptional mapping, and temporal expression of the gp64 envelope glycoprotein gene of the Orgyia pseudotsugata multicapsid nuclear polyhedrosis virus. Virology. 1989;170(2):537–555. doi: 10.1016/0042-6822(89)90445-5. [DOI] [PubMed] [Google Scholar]
- 34.Hohmann AW, Faulkner P. Monoclonal antibodies to baculovirus structural proteins: determination of specificities by Western blot analysis. Virology. 1983;125(2):432–444. doi: 10.1016/0042-6822(83)90214-3. [DOI] [PubMed] [Google Scholar]
- 35.Connors M, Collins PL, Firestone CY, Murphy BR. Respiratory syncytial virus (RSV) F, G, M2 (22K), and N proteins each induce resistance to RSV challenge, but resistance induced by M2 and N proteins is relatively short-lived. J Virol. 1991;65(3):1634–1637. doi: 10.1128/jvi.65.3.1634-1637.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walsh EE, Hall CB, Briselli M, Brandriss MW, Schlesinger JJ. Immunization with glycoprotein subunits of respiratory syncytial virus to protect cotton rats against viral infection. J Infect Dis. 1987;155(6):1198–1204. doi: 10.1093/infdis/155.6.1198. [DOI] [PubMed] [Google Scholar]
- 37.Sastre P, Melero JA, Garcia-Barreno B, Palomo C. Comparison of affinity chromatography and adsorption to vaccinia virus recombinant infected cells for depletion of antibodies directed against respiratory syncytial virus glycoproteins present in a human immunoglobulin preparation. J Med Virol. 2005;76(2):248–255. doi: 10.1002/jmv.20349. [DOI] [PubMed] [Google Scholar]
- 38.Stott EJ, Taylor G, Ball LA, et al. Immune and histopathological responses in animals vaccinated with recombinant vaccinia viruses that express individual genes of human respiratory syncytial virus. J Virol. 1987;61(12):3855–3861. doi: 10.1128/jvi.61.12.3855-3861.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melnick JL. Thermostability of poliovirus and measles vaccines. Dev Biol Stand. 1996;87:155–160. [PubMed] [Google Scholar]
- 40.Ikizler MR, Wright PF. Thermostabilization of egg grown influenza viruses. Vaccine. 2002;20(9–10):1393–1399. doi: 10.1016/s0264-410x(01)00466-2. [DOI] [PubMed] [Google Scholar]
- 41.Yannarell DA, Goldberg KM, Hjorth RN. Stabilizing cold-adapted influenza virus vaccine under various storage conditions. J Virol Methods. 2002;102(1–2):15–25. doi: 10.1016/s0166-0934(01)00432-3. [DOI] [PubMed] [Google Scholar]
- 42.Arya SC, Agarwal N. Efficacy of measles vaccine interlinked with potency and storage. Acta Trop. 2004;90(2):223–225. doi: 10.1016/j.actatropica.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 43.Huang J, Garmise RJ, Crowder TM, et al. A novel dry powder influenza vaccine and intranasal delivery technology: induction of systemic and mucosal immune responses in rats. Vaccine. 2004;23(6):794–801. doi: 10.1016/j.vaccine.2004.06.049. [DOI] [PubMed] [Google Scholar]
- 44.Hosokawa M, Hama S, Mandai K, et al. Preparation of purified, sterilized, and stable adenovirus vectors using albumin. J Virol Methods. 2002;103(2):191–199. doi: 10.1016/s0166-0934(02)00028-9. [DOI] [PubMed] [Google Scholar]
- 45.Wu R, Georgescu MM, Delpeyroux F, et al. Thermostabilization of live virus vaccines by heavy water (D2O) Vaccine. 1995;13(12):1058–1063. doi: 10.1016/0264-410x(95)00068-c. [DOI] [PubMed] [Google Scholar]
- 46.Jarvis DL, Garcia A., Jr Long-term stability of baculoviruses stored under various conditions. Biotechniques. 1994;16(3):508–513. [PubMed] [Google Scholar]
- 47.Ruiz-Arguello MB, Martin D, Wharton SA, et al. Thermostability of the human respiratory syncytial virus fusion protein before and after activation: implications for the membrane-fusion mechanism. J Gen Virol. 2004;85(Pt 12):3677–3687. doi: 10.1099/vir.0.80318-0. [DOI] [PubMed] [Google Scholar]