Abstract
Purpose
To study the β-catenin gene in a group of Mayer-Rokitansky-Küster-Hauser patients.
Methods
Twelve patients with the Mayer-Rokitansky-Küster-Hauser syndrome were included in this study. DNA was extracted from peripheral blood and the region codifying β-catenin GSK-3β phosphorylation sites on exon 3 was amplified. PCR products were purified and directly sequenced.
Results
No mutations were found in the GSK-3β phosphorylation sites on exon 3 of β-catenin gene in this group of patients with the MRKH syndrome.
Conclusions
β-catenin gene mutations are an unlikely cause of the MRKH syndrome.
Keywords: Mayer-Rokitansky-Küster-Hauser syndrome, β-catenin, molecular analysis, Müllerian ducts, anti-Müllerian hormone
Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome (MIM *277000), a congenital malformation of the Müllerian ducts, is the second most common cause of primary amenorrhea, occurring in one in every 4,000 to 5,000 female live births. The extent of MRKH anomaly is variable, ranging from upper vaginal atresia and rudimentary uterus to total uterine, fallopian tubes and upper vaginal agenesis. Additional congenital skeletal and renal abnormalities are present in approximately 30% of the patients [1]. Clinically, the diagnosis should be suspected if primary amenorrhea and infertility are present in 46, XX individuals with normal ovaries and normal secondary sexual characteristics.
The cause of the MRKH syndrome remains unexplained. The presence of familial clustering described in previous studies suggests a genetic defect [2, 3]. Nevertheless, the molecular basis of the MRKH syndrome has not yet been established. The putative defective gene could be either involved in the process of Müllerian duct formation, or associated with abnormal activation of the anti-Müllerian hormone (AMH) signaling pathway, leading to Müllerian duct regression. Indeed, both hypotheses could ultimately result in the MRKH syndrome phenotype.
Comprising the first group, several genes encoding transcription factors and signaling molecules have been studied. WT1, PAX-2, WNT-7a, RXR-alpha, RXR-gamma, HOXA-7 to HOXA-13, and PBX-1 are genes required for Müllerian duct formation and differentiation, which have been evaluated in different groups of patients and were all excluded as causes of the MRKH syndrome [4–8]. Analysis of WNT4, a gene encoding a signaling molecule crucial for ovarian and uterine development, has provided us with interesting information. WNT4 gene mutations have been described in patients with Mullerian duct abnormalities and hyperandrogenism [9–11], but were not found in patients with the classic MRKH syndrome phenotype [6, 11–13]. These results suggest that WNT4 gene mutation is a clinical phenotype distinct from the isolated MRKH, and exclude it as a major cause of the MRKH syndrome. Among the genes involved in the AMH signaling pathway, the AMH gene has been studied for activating mutations, which were not detected [14,15]. AMH type 2 receptor gene (AMHRII) and the three potential AMH type 1 receptor genes (AMHRI) were also investigated and no mutations were found [12, 14, 16].
This consistently negative data has prompted us to search for other candidate genes involved in Müllerian duct development during embryogenesis. β-catenin, a multi-functional protein that can affect both cell—cell adhesion and signal transduction [17], has been shown to mediate AMH dependent Müllerian degeneration. AMH acts on the Müllerian epithelium through a paracrine mechanism originating in the periductal mesenchyme. This member of the TGF-β family signals through receptor complexes of two related serine/threonine kinase transmembrane receptors, which must be co-expressed for appropriate signal transduction [18]. Whereas AMHRI is ubiquitous, AMHRII is expressed only in the mesenchymal cells surrounding the Müllerian ducts [19]. The AMH action in peri-Müllerian cells leads to accumulation of cytoplasmatic β-catenin in a cranial-caudal fashion, correlating with the pattern of Müllerian duct regression. Interestingly, nuclear β-catenin immunoreactivity is also observed, co-localized with lymphoid enhancer factor-1 (LEF-1) [20]. This finding suggests that AMH induced β-catenin expression could be involved in gene transcription regulation. Heterodimerization of β-catenin with LEF/TCF family members generates an efficient complex able to activate or repress gene transcription. It has been demonstrated that β-catenin is essential for the activation of AMHRII gene promoter [21]. Thus, it is possible that mutations in the β-catenin gene (CTNNB1) could be the cause of the Müllerian defect observed in patients with MRKH syndrome. β-catenin cytoplasmatic and nuclear accumulation occur as consequences of mutations on exon 3 of the CTNNB1 gene, which affect serine/threonine phosphorylation by glycogen synthase kinase-3β (GSK-3β), and protect the β-catenin protein from degradation [22, 23]. Mutations affecting GSK-3β phosphorylation residues could result in abnormal activation of the AMHRII gene promoter, even in absence of AMH, and could ultimately cause abnormal regression of the Müllerian ducts in MRKH patients.
Material and methods
Twelve patients (age 16 to 36 years) with the MRKS syndrome referred to a tertiary infertility center complaining of primary amenorrhea were included in this study. Ten patients were unrelated, while the remaining two cases were sisters. All patients had normal female karyotype (46, XX) and normal secondary sexual characteristics. Pelvic ultrasound examination revealed rudimentary uterus and upper vagina atresia in ten of the patients, while the uterus was not visualized in the remaining two—laparotomy confirmed uterine agenesis in one of these patients. Four patients presented unilateral renal agenesis; while one patient presented duplication of the renal collecting system. None of the twelve patients had clinical or laboratorial evidence of hyperandrogenism. Skeletal or other associated malformations were not present in this group of patients.
After informed consent, peripheral blood was collected from patients and controls (six individuals) and the samples were stored in −20°C until DNA was extracted with Invitrogen DNA extraction Kit. DNA samples were then subjected to polymerase chain reaction (PCR). The following oligonucleotide primers, encompassing GSK-3β phosphorylation sites on exon 3 of the CTNNB1 gene were used: sense: 5′-GATTTGATGGAGTTGGACATGG-3′ and antisense: 5′-TGTTCTTGAGTGAAGGACTGAG-3′ (226 base pairs). Standard PCR reactions were set up in a total volume of 50 μl, containing 100 ng of genomic DNA, 10 pM of each primer, 5 μl reaction buffer (10X), 200 μM of each dNTP, and 1U of Taq polymerase (Invitrogen, Carlsbad, CA). After an initial 5 min denaturation step at 95°C, the reactions were subjected to 35 amplification cycles of 94°C × 30 sec, 55° × 40 sec, 72° × 40 sec, followed by 5 min final incubation at 72°. PCR products were purified with GFX PCR DNA and Gel band Purification Kit (Amersham Biosciences, Piscataway, NJ) and directly sequenced on an ABI PRISM 310 Genetic Analyser (Applied Biosystems, Foster City, CA), using the Big Dye Terminator method according to the manufacturer’s instructions.
Results
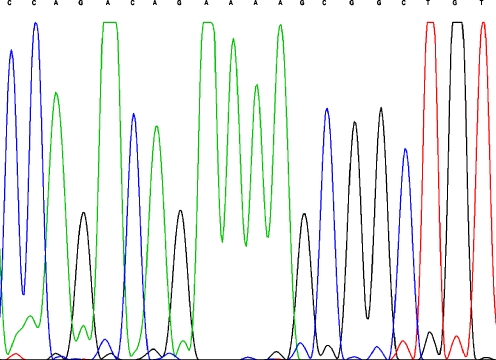
Sequencing analyses performed on PCR products detected no nucleotide variation in the sequence that codifies β-catenin GSK-3β phosphorylation sites on exon 3 of the CTNNB1 gene in this group of patients with the MRKH syndrome (Fig. 1) nor in the controls.
Fig. 1.
Chromatogram of the CTNNB1 gene in a MRKH patient showing no nucleotide variation in the sequence codifying β-catenin GSK-3β phosphorylation sites
Discussion
The genetic factors regulating female sexual differentiation have not yet been clarified. Undoubtedly, it is far more complicated than the previous belief that the female represented the default pathway in mammalian reproductive tract development. Elucidation of the molecular basis of the MRKH syndrome could not only shed light upon the pathogenesis of the syndrome, but could greatly contribute to the general understanding of the genetic control of human fetal sexual development.
CTNNB1 seemed a particularly interesting candidate gene, since β-catenin is a downstream effector of both AMH and WNT signaling pathways, which may function cooperatively in mediating Müllerian duct regression [24]. Whether the effect of AMH involves WNT signaling in the Müllerian mesenchyme is unknown. To date, activation of β-catenin/ TCF signaling has only been described in association with the canonical WNT/ β-catenin pathway. Activation of this pathway inhibits β-catenin phosphorylation, thus creating a large pool of soluble non-phosphorylated β-catenin [17]. In fact, WNT7a expression in the Müllerian duct epithelium is essential for the expression of AMHRII in both sexes [25]. However, in mammals, β-catenin accumulation during the critical period of Müllerian duct regression is independent of Wnt7a action as the cytoplasmatic accumulation of β-catenin occurs well after the effects of Wnt7a on AMHRII gene expression [20]. Although we still do not completely understand how AMH and WNT signaling pathways interact, enough evidence indicates that β-catenin plays a major role in the activation of AMHRII promoter during Müllerian duct regression [21]. Since abnormal cytoplasmatic and nuclear β-catenin accumulation had been described as a consequence of mutations on the CTNNB1 gene [22], the hypothesis that CTNNB1 gene mutations caused Müllerian duct derivative abnormalities was very attractive.
We studied the exon 3 of the CTNNB1 gene, the region codifying β-catenin GSK-3β phosphorilation sites. Mutations affecting this region interfere with β-catenin serine/threonine phosphorylation by GSK-3β, leading to β-catenin accumulation [22]. The evaluation of 12 patients with the MRKH syndrome did not reveal any mutations on exon 3 of CTNNB1 gene. Since mutation detection using direct DNA sequence analysis is regarded as the most sensitive strategy, we conclude that CTNNB1 exon 3 mutations are an unlikely cause of the MRKH syndrome.
The molecular mechanisms regulating the cross-talk between the mesenchyme and the epithelium during Müllerian duct regression are unclear. Further studies are required in order to clarify how AMH induces β-catenin accumulation, whether AMH activates simultaneously the bone morphogenetic pathway (BMP) and the β-catenin/LEF-1 pathway in periductal mesenchymal cells and what other AMH downstream signaling events are crucial for Müllerian duct regression. The answer to these questions can perhaps provide new insights into the elucidation of the genetic basis of the MRKH syndrome.
Acknowledgement
This work was partially supported by FAPEMIG and CNPq (#473169/2004-5), Brasil.
Footnotes
Capsule β-catenin gene mutations were not detected in a group of twelve patients with the Mayer-Rokitansky Küster-Hauser (MRKH) anomaly.
References
- 1.Oppelt P, Renner SP, Kellerman A, Brucker S, Hauser GA, Ludwig KS, et al. Clinical aspects of Mayer-Rokitansky-Kuester-Hauser syndrome: recommendations for clinical diagnosis and staging. Hum Reprod 2006;21:792–7. doi:10.1093/humrep/dei381. [DOI] [PubMed]
- 2.Griffin JE, Edwards C, Madden JD, Harrod MJ, Wilson JD. Congenital absence of the vagina. The Mayer-Rokitansky-Küster-Hauser syndrome. Ann Intern Med 1976;85:224–36. [DOI] [PubMed]
- 3.Kobayashi A, Behringer RR. Developmental genetics of the female reproductive tract in mammals. Nat Rev Genet. 2003;4:969–80. doi:10.1038/nrg1225. [DOI] [PubMed]
- 4.Van Lingen BL, Reindollar RH, Davis AG, Gray MR. Further evidence that the WT1 gene does not have a role in the development of the derivatives of the mullerian duct. Am J Obstet Gynecol. 1998;179:597–603. doi:10.1016/S0002-9378(98)70051-1. [DOI] [PubMed]
- 5.Van Lingen BL, Eccles N, Reindollar RH, Gray MR. Molecular Genetic Analysis of the PAX2 gene in patients with congenital absence of the uterus and vagina. Fertil Steril. 1998;70:S42.
- 6.Cheroki C, Krepischi-Santos AC, Rosenberg C, Jehee FS, Mingroni-Netto RC, Pavanello Filho I, et al. Report of a del22q11 in a patient with Mayer-Rokitansky-Kuster-Hauser (MRKH) anomaly and exclusion of WNT4, RAR-gamma and RXR-alpha as major genes determining MRKH anomaly in a study of 25 affected women. Am J Med Genet A. 2006;140:1339–42. doi:10.1002/ajmg.a.31254. [DOI] [PubMed]
- 7.Timmreck L, Pan H, Reindollar R, Gray MR. WNT7A mutations in patients with Mullerian duct abnormalities. J Pediatr Adolesc Gynecol. 2003;16:217–22. doi:10.1016/S1083-3188(03)00124-4. [DOI] [PubMed]
- 8.Burel A, Mouchel T, Odent S, Tiker F, Knebelmann B, Pellerin I, Guerrier D. Role of HOXA7 to HOXA 13 and PBX1 genes in various forms of MRKH syndrome (congenital absence of uterus and vagina). J Negat Results Biomed. 2006;5:4. doi:10.1186/1477-5751-5-4. [DOI] [PMC free article] [PubMed]
- 9.Biason-Lauber A, Konrad D, Navratil F, Schoenle EJ. A WNT4 mutation associated with Mullerian-duct regression in a 46, XX woman. N Engl J Med. 2004;351:792–8. doi:10.1056/NEJMoa040533. [DOI] [PubMed]
- 10.Biason-Lauber A, De Filippo G, Konrad D, Scarano G, Nazzaro A, Schoenle EJ. WNT4 deficiency—a clinical phenotype distinct from the classic Mayer-Rokitansky-Kuster-Hauser syndrome: a case report. Hum Reprod. 2007;22:224–9. doi:10.1093/humrep/del360. [DOI] [PubMed]
- 11.Philibert P, Biason-Lauber A, Rouzier R. Identification and functional analysis of a new WNT4 gene mutation among 28 adolescent girls with primary amenorrhea and müllerian duct abnormalities: a French collaborative study. J Clin Endocrinol Metab. 2008;93:895–900. doi:10.1210/jc.2007-2023. [DOI] [PubMed]
- 12.Clement-Ziza M, Khen N, Gonzales J. Exclusion of WNT4 as a major gene in Rokitansky-Kuster-Hauser anomaly. Am J Med Genet A. 2005;137:98–9. doi:10.1002/ajmg.a.30833. [DOI] [PubMed]
- 13.Drummond JB, Reis FM, Boson WL, Silveira LF, Bicalho MA, De Marco L. Molecular analysis of the WNT4 gene in 6 patients with Mayer-Rokitansky-Küster-Hauser syndrome. Fertil Steril. doi:10.1016/j.fertnstert.2007.07.1319 [DOI] [PubMed]
- 14.Zenteno J, Carranza-Lira S, Kofman-Alfaro S. Molecular analysis of the anti-Mullerian hormone, the anti-Mullerian hormone receptor, and galactose-1-phosphate uridyl transferase genes in patients with the Mayer-Rokitansky-Kuster-Hauser syndrome. Arch Gynecol Obstet. 2004;269:270–3. doi:10.1007/s00404-002-0456-7. [DOI] [PubMed]
- 15.Oppelt P, Strissel PL, Kellermann A, Seeber S, Humeny A, Beckmann MW, et al. DNA sequence variations of the entire anti-Mullerian hormone (AMH) gene promoter and AMH protein expression in patients with the Mayer-Rokitansky-Kuster-Hauser syndrome. Hum Reprod. 2005;20:149–57. doi:10.1093/humrep/deh547. [DOI] [PubMed]
- 16.Resendes BL, Sohn SH, Stelling JR, Tineo R, Davis AJ, Gray MR, et al. Role of anti-Mullerian hormone in congenital absence of the uterus and -vagina. Am J Med Genet. 2001;98:129–36. doi:10.1002/1096-8628(20010115)98:2<129::AID-AJMG1021>3.0.CO;2-3. [DOI] [PubMed]
- 17.Resnik E. β-catenin—one player, two games. Nat Genet. 1997;16:9–11. doi:10.1038/ng0597-9. [DOI] [PubMed]
- 18.Massagué J. How cells read TGF-beta signals. Nat Rev Mol Cell Biol. 2000;1:169–78. doi:10.1038/35043051. [DOI] [PubMed]
- 19.Josso N, Clemente N. Transduction pathway of anti-Mullerian hormone, a sex-specific member of the TGF-beta family. Trends Endocrinol Metab. 2003;14:91–7. doi:10.1016/S1043-2760(03)00005-5. [DOI] [PubMed]
- 20.Allard S, Adin P, Gouédard L, di Clemente N, Josso N, Orgebin-Crist MC, et al. Molecular mechanisms of hormone-mediated duct regression: involvement of beta-catenin. Development. 2000;127:3349–60. [DOI] [PubMed]
- 21.Hossain A, Saunders GF. Synergistic cooperation between the β-catenin signaling pathway and steroidogenic factor 1 in the activation of the mullerian inhibiting substance type II receptor. J Biol Chem. 2003;278:26511–6. doi:10.1074/jbc.M300804200. [DOI] [PubMed]
- 22.Polakis P. Wnt signaling and cancer. Genes Dev. 2000;14:1837–51. [PubMed]
- 23.Kikuchi A. Tumor formation by genetic mutations in the components of Wnt signaling pathway. Biochem Biophys Res Commun. 2000;2:243–8. doi:10.1006/bbrc.1999.1860. [DOI] [PubMed]
- 24.Zhan Y, Fujino A, Maclaughlin D, Manganaro TF, Szotek PP, Arango NA, et al. Mullerian inhibiting sustance regulates its receptors/SMAD signaling and causes mesenchymal transition of the coelomic epithelial cells early in Mullerian duct regression. Development. 2006;133:2359–69. doi:10.1242/dev.02383. [DOI] [PubMed]
- 25.Parr B, McMahon AP. Sexually dimorphic development of the mammalian reproductive tract requires Wnt-7a. Nature. 1998;395:707–10. doi:10.1038/27221. [DOI] [PubMed]