Abstract
A sample of 124 women with osteoarthritis (OA) and/or fibromyalgia (FMS) completed initial assessments for demographic data, health status, and personality traits and 10 to 12 weekly interviews regarding pain, stress, negative affect, and positive affect. Multilevel modeling analyses indicated that weekly elevations of pain and stress predicted increases in negative affect. Both higher weekly positive affect as well as greater positive affect on average resulted in lower negative affect both directly and in interaction with pain and stress. Finally, increases in weekly negative affect and higher average negative affect related to greater levels of pain in subsequent weeks. In contrast, higher levels of overall positive affect predicted lower levels of pain in subsequent weeks.
Keywords: Positive affect, negative affect, chronic pain, stress, resilience
Traditionally, pain research has focused on the relationship between stress, pain, and negative affectivity. People with pain conditions consistently show elevations in negative affects, including higher depression and anxiety, in comparison to those without a chronic pain condition (Hawley & Wolfe, 1993; Hudson & Pope, 1989, 1990). In turn, people with elevations in these negative affective states often show greater sensitivity to pain stimuli (Beckham, Keefe, Caldwell, & Roodman, 1991; Geisser, et al., 2003). Further, everyday stressors have been shown to lower pain tolerance and increase pain unpleasantness among those with chronic pain conditions like Fibromyalgia (FMS) and Osteoarthritis (OA) (Affleck, Urrows, Tennen, Higgins, Pav, & Aloisi, 1997; Geisser, et al., 2003). Little empirical attention has been given, however, to the role of resilience resources that may aid in the recovery from pain or stress for populations with chronic pain. Positive emotions, in particular, may play an important role in fostering recovery following episodes of high pain (Zautra, Smith, Affleck, & Tennen, 2001). The purpose of this study was to examine the role of positive affect in blunting the impact of exacerbation of pain and interpersonal stress on negative affective states among women with OA and/or FMS.
Watson and Clark (1992) have proposed that positive affects are relatively independent from negative affect. Since pain has been shown to increase negative affective states primarily, and have a more limited influence on positive affects (Zautra, et al., 1995), their theoretical model would not appear to predict any central role for positive emotions in protecting against declines in well being, such as increases in negative affect, among those in chronic pain. However, recent evidence appears to contradict Watson and Clark's model by showing that positive affect is relevant to recovery from pain (Zautra, et al., 2001), and that patients with FMS, a chronic pain condition, show a relative deficit in positive affect (Davis, Zautra, & Reich, 2001; Zautra, Hamilton, & Burke, 1999).
One mechanism by which positive emotions may play a role in the regulation of negative states that accompany pain has been proposed recently by Zautra et al. (2001) in their dynamic model of affect (DMA). In this DMA, the degree of complexity in individuals’ awareness of their own emotions is significantly reduced during times of stress. Heightened pain, as a stressor, would narrow the range of emotional experiences leading to an increasingly inverse relationship between positive and negative emotions during pain episodes. Thus, the presence of positive emotions may become more critical to preservation of well-being during times of high pain as well as during other stressful times. A relative deficit in positive emotions would increase vulnerability to negative emotions during stressful times.
Some investigators have further proposed that positive emotions are important psychological resources that a person may gather over time and employ to aid in coping efforts during stressful occasions (Fredrickson & Joiner, 2002; Hobfoll, 1989). In Fredrickson and Joiner's (2002) model, positive emotions may be said to enhance well-being by broadening and building a sense of well-being. Hobfoll (1989) suggested that positive gains would add up over time to serve as a resource during subsequent times of social stress. Thus, people who tend to experience more positive emotions would be expected to be more resistant to stressful events, and thus more resilient than those participants without a steady diet of positive emotion.
The DMA and the Fredrickson and Hobfoll models provide complementary predictions for the most part. Both models predict individual differences in the vulnerability of chronic pain patients to negative affect during pain and other stressful events, where they differ is in the relative emphasis on trait versus state components of positive emotional resources. Fredrickson and Hobfoll's model focuses on the stable differences in affect between people over time, while the DMA focuses on changes within a person's current state of affect independent of their trait level of affect. The DMA also predicts that the timing of the affects matters, such that elevations in positive affect during times of heightened stress, including pain, are particularly important in the regulation of negative affective states.
Based on prior research applying the DMA to pain populations (Zautra et al., 2001), we theorized that deficits in positive affect during times of high pain and stress may increase vulnerability to more negative affective states during these times. Further, we hypothesized that participants who tended to experience more positive affect on average, would experience lower levels of negative affect during times of stress and pain, as predicted by Fredickson and Hobfoll's model. To pursue these questions, we formulated the following specific hypotheses:
Pain elevations will increase negative affect less when weekly positive affect is high.
Stress elevations will increase negative affect less when weekly positive affect is high.
Pain elevations will increase negative affect less for participants who have higher overall levels of positive affect.
Stress elevations will increase negative affect less for participants who have higher overall levels of positive affect.
To determine the utility of the above hypotheses to the subsequent experience of pain, we also tested whether higher levels of negative affect increased vulnerability to future pain episodes, promoting a cycle of increasing pain and emotional disturbance that would be mutually reinforcing. Formally, this constituted a fifth hypothesis:
5. Weekly negative affect will increase the likelihood of pain elevations on subsequent weeks.
We tested these hypotheses in two chronic pain conditions common among women in mid-life: Osteoarthritis and Fibromyalgia. Osteoarthritis is a common inflammatory joint disease that afflicts women and men with increasing prevalence as they age, characterized by pain and swelling in weight-bearing joints such as the knee and/or hip. Fibromyalgia, on the other hand, is a syndrome of unknown etiology, characterized by widespread pain in the soft tissue rather than in the joints and no inflammation. Since these two chronic pain conditions are different from one another, it was also possible that positive affect would be less protective for FMS patients compared with OAs, so tests were planned to examine differences in the relationships between positive affective and negative affective states as a function of diagnosis.
Method
Participants
Participants were 124 women between the ages of 35 and 72 (FMS, N = 86, OA, N = 38; Mean age = 54.6 at initial assessment) who had a rheumatologist-confirmed diagnosis of Fibromyalgia (FMS) and/or Osteoarthritis (OA). If women had both FMS and OA, they had to report FMS as the most disabling of the two conditions to be classified in the FMS group. Further, the OA group had to have some amount of pain and disability to be comparable to the FMS group, which limited our pool of eligible OAs. The sample was comprised of Caucasian women (96%) predominantly, who were educated at a post-high school education level (80%). The average household income of the participants fell within the range of $50,000 to $59,999, and 62% were not employed at the beginning of the study.
Study criteria dictated that each participant had a pain level over the past week that was more than 20 or the mean average pain over the past week and the average pain over the past month was more than 25 on a 0 to 100 scale, where 0 is “no pain” and 100 is “pain as bad as it can be,” was not currently involved in any health-related litigation, was living with a romantic partner who also was willing to participate in the study, and was diagnosed after 1988.
There were two reasons for the requirement of a participating partner. First, we planned to carry out separate studies of congruence with reporting support using partner data (Davis, Zautra, & Smith, in press). Second, the requirement that all participants be living with a romantic partner allowed for more uniformity across the sample in terms of interpersonal stress. We have found in our prior work that stresses emanating from intimate relations were the most impactful and thus people without partners may not have comparable stress scores. The criteria that diagnosis needed to be made after 1988 coincided with increasing awareness and standardization in the diagnosis of Fibromyalgia (Wolfe et al., 1990). Further, if participants had illnesses other than FMS or OA, they were allowed to participate only if they ranked their FMS or OA as causing them the most difficulty of all their conditions. Participants were recruited through a variety of means including flyers placed in physicians’ offices and other public locations, physicians passing along information to their patients, newspaper ads, senior citizens’ groups, arthritis groups, and mass mailings to members of the Arthritis Foundation. Two major components of the study provided data for this investigation: an initial assessment, and 10 to 12 weekly telephone interviews.
Of the 332 participants who were screened, 39% were ineligible based on the criteria set for this study. The main reasons that made potential participants ineligible included that FMS or OA pain was not their primary pain condition, their pain level was too low based on study criteria, they were involved in health-related litigation, they had other health conditions that made them excluded from the study, such as rheumatoid arthritis and lupus, or that they had a diagnosis of FMS or OA prior to 1988. We had incomplete data for refusal rates because we lost contact with some eligible potential participants prior to their completion of the initial questionnaire. Of the eligible participants, 9% declined to participate giving one of the following reasons: the time commitment being too high, they were already participating in another study, or that they were just not interested after description of the study. Our attrition rate was approximately 5% including participants who stopped participation after we received their initial questionnaire, but before they began the weekly phase of the study. There were 130 participants who completed an initial questionnaire and 124 participants who completed an initial questionnaire and at least one of the weekly interviews. Participation in the weekly phase of the study was considered in these analyses if the participant completed at least one weekly questionnaire.
Procedure
Initial assessment
All participants returned an informed consent form by mail. Upon receipt of these forms, participants were mailed an initial questionnaire that contained items to assess demographic data and health status, including average pain and fatigue, as well as personality traits, such as neuroticism and extraversion (John, Donahue, & Kentle, 1991). These questionnaires were picked up at the time of an in-home visit. Home visits consisted of an interviewer-administered questionnaire assessing mental and physical health and a physical assessment of pain using the multiple tender point examination (Okifuji, Turk, Sinclair, Starz, & Marcus, 1997).
Weekly interviews
At the end of the visit, participants were thanked and given $25 in appreciation for their time. After the home visit, participants entered the Weekly Interview phase of the study. At this point, all participants were assigned an interviewer, who was a research assistant trained to perform a standardized 45-minute telephone interview. The study called for each participant to be interviewed once a week for 10 to 12 weeks. Each weekly interview included the following measures: a numerical pain index (the participants rated their pain on a scale from 0 to 100), a series of probes of the frequency of everyday life events and ratings of interpersonal stress (ISLE; Zautra, Reich, & Guarnaccia, 1990), and measures of positive and negative affect (PANAS; Watson & Clark, 1999). The interviews were terminated after Week 10 if the participant completed each weekly interview and experienced a “stress week,” defined as a week where relations with friends, spouse, family or work were highly stressful, as judged by self-report. If any weeks were missed or the participant did not report a stressful week, the weekly interviews continued through Week 12. If an interview did not occur at its regularly scheduled time, the interviewer attempted to contact the participant for up to 3 days. After 3 days of no contact, data for that week were considered missing. The average number of weekly interviews for each subject was 9.0, with 5.8% of weekly interviews missing.
Measures
Weekly pain
Weekly pain was assessed during each weekly interview with the standard instruction for a numerical rating scale (Jensen, Karoly, & Braver, 1988; Zautra et al., 2001), “Please choose a number between 0 and 100 that best describes the average level of pain you have experienced over the past week due to your fibromyalgia or osteoarthritis. A zero (0) would mean ‘no pain’ and a one hundred (100) would mean ‘pain as bad as it can be.’” In order to estimate reliability for this single item measure, test-retest reliabilities were conducted across the 10−12 weeks. This yielded an average week-to-week correlation of .69.
Positive affect and negative affect
Positive affect and negative affect were measured during each weekly interview using the Positive and Negative Affect Schedule-Expanded Form (Watson & Clark, 1999). Participants were asked to indicate on a 5-point scale (from 1, very slightly or not at all, to 5, extremely) the extent to which they had experienced each of 10 positive affects during the past week. The positive affect items were “interested,” excited,” “strong,” “enthusiastic,” “proud,” alert,” “inspired,” “determined,” “attentive,” and “active.” Positive affect scores represent the mean for the 10 items. Week 1 scores were analyzed to obtain alphas for each weekly measure. Cronbach's (1951) alpha for the positive affect scale was .88 in the present study.
Negative affect was also measured with 10 items using the same format as positive affect. The negative affect items were “distressed,” “upset,” “nervous,” “scared,” “hostile,” “irritable,” “ashamed,” “jittery,” “afraid,” and “guilty.” Negative affect scores represent the mean for the 10 items. Cronbach's alpha for the negative affect scale was estimated at .84 in the present study using week 1 data.
Perceived interpersonal stress
We focused on the assessment of perceived interpersonal stress in this study because stresses of an interpersonal nature have been found to be especially salient, particularly for women (Davis, Matthews, & Twamley, 1999). During each weekly interview, perceived interpersonal stress was measured within four interpersonal domains: (1) friends and acquaintances, (2) spouse or live-in partner, (3) family members, and (4) coworkers following methods used in prior studies (e.g. Zautra & Smith, 2001). First, the interviewer read a series of items that identified stressful and non-stressful events within each interpersonal domain, and asked participants to report on the frequency of those events over the past week, using items from the Inventory of Small Life Events (Zautra, Reich, & Guarnaccia, 1990). For example, in the friends/acquaintances domain, participants were probed in the frequency of the following events: “argued with friend/acquaintance” or “met an unfriendly or rude person.” For spouse/partner, items were used such as “criticized by spouse/partner” or “argued with spouse/partner.” For family, items such as “had an argument with family member other than spouse” or “criticized or blamed for something by a family member other than spouse/partner” were probed. For coworkers, items such as “got a negative job performance review” or “disagreement with others about your job assignment(s)” were queried. This procedure was used to provide an event-related context for ratings of stressfulness. Following the reports of events in each domain, the interviewer asked the participant to rate how stressful they felt overall about relationships in that domain with the following instruction, “Overall, how stressful were your relations with (friends/spouse/family members/coworkers) this past week?” Participants were asked to rate using a 4-point Likert scale (from 0, Not stressful at all to 3, Extremely stressful) how stressful the relations were in the past week for each domain. The total score was created by calculating the mean for the items from the domains that applied to the participant. If items from one domain was missing (e.g., because they were not employed), then the average of the remaining items was taken. Cronbach's alpha was not computed because the items were designed to measure non-overlapping interpersonal domains, such that stress in one domain is not necessarily indicative of stress in other domains. Instead, test-retest reliabilities were computed across weeks yielding an average week-to-week correlation of .51. (“Perceived interpersonal stress” will be abbreviated to “interpersonal stress” for the remainder of the article.)
Neuroticism
Neuroticism was assessed in the initial questionnaire, completed by the participant and picked up at the home visit. Eight neuroticism items from the John, Donahue, and Kentle (1991) measure of the Big 5 traits were used. Participants rated their agreement with each statement beginning with “I see myself as someone who...” on a 5-point scale, with 1 representing “Disagree strongly,” 3 representing “Neither agree nor disagree,” and 5 representing “Agree strongly.” Examples of neuroticism items included “Can be moody,” “Can be tense,” and “Gets nervous easily.” Cronbach's alpha was .81 for neuroticism in the present study. This scale was used to control for differences in predisposition to experience positive and negative affect that could be a source of confounding in the current study.
Data Analysis Methods
Weekly data from the OA and FMS samples were used to probe the predicted role of positive affect as a resource for adaptation to chronic pain and interpersonal stress. Multilevel modeling was used as the primary data-analytic tool to analyze the weekly data. This method is particularly useful for the analysis of data that have a nested hierarchical structure. The weekly data take a hierarchical form, with up to 10−12 observations nested within each of the 124 participants. All multilevel analyses were conducted using the SAS PROC MIXED software (Littell, Milliken, Stroup, & Wolfinger, 1996).
Weekly negative affect was the primary criterion variable to be predicted in the analyses. There were two basic types of prediction equations in the multilevel analyses: A level 1 equation which examined the influence of within person variations of key variables on negative affect, and a level 2 equation which tested the effects of between person variations on key variables. In essence, the level 2 variables address questions regarding between-person differences, and take the following form: Do people who score higher on the predictor (e.g., average positive affect) also have less negative affect? Level 1 questions address questions about when rather than who. They take the following form: When a person has higher positive affect, do they also report lower negative affect? We asked questions that assessed interactions between two Level 1 variables. For example, when people have more positive affect, is there a weaker relation between pain and negative affect? We also assessed interactions across levels, for example: Do people who have high average positive affect show less negative affect when pain is high than people who have low positive affect?
The Level 1 equation examined within-person variation in positive affect (weekly positive affect), pain reports (weekly pain), and interpersonal stress (weekly interpersonal stress) related to weekly negative affect. To prepare for this analysis, weekly deviation scores on positive affect, stress, and pain were computed by subtracting each participant's average score on those variables across the 10−12 weeks from her weekly report on each variable. The subtraction yielded weekly deviation scores from the participant's own average score on each of the key variables: pain, positive affect (PA), interpersonal stress, and two interaction terms, obtained from the products of interpersonal stress × PA, and pain × PA.
The equation was initially specified at Level 1 as follows:
Level 1: weekly negative affect = β0 + β1 pain + β2 positive affect + β3 stress + β4 pain × positive affect + β5 stress × positive affect + r
β0 yields an estimate of the average weekly negative affect and β1-β5 provide slope estimates of the effects of predictor variables on weekly negative affect. In addition to pain, stress, positive affect and their interactions, initial models also included the week number in the study to test for any effects of the week of assessment on these prediction equations. The linear or fixed effect of week was non-significant and therefore was dropped from the prediction equation (The random effect was significant as shown in Table 2).
Table 2.
Multilevel Regressions Predicting Weekly Negative Affect
| Random Effects | |||||
|---|---|---|---|---|---|
| Covariance Parameter Estimates | Subject | β | SE | Z | p |
| Intercept | ID | 0.08 | .015 | 4.97 | <.001 |
| ΔPA | ID | 0.50 | .017 | 2.97 | .002 |
| ΔIS | ID | 0.06 | .025 | 2.22 | .013 |
| Week | ID | 0.00 | .000 | 4.00 | <.001 |
| Residual | ID | 0.12 | .006 | 19.55 | <.001 |
| Fixed Effects | ||||||
|---|---|---|---|---|---|---|
| Predictor Variables | β | SE | r2 | 95% CI | t | p |
| Level 1 (df = 1038) | ||||||
| Δ in Weekly Pain (ΔWP) | 0.022 | .004 | .24 | [.01, .03] | 5.04 | <.001 |
| Δ in Positive Affect (ΔPA) | −0.234 | .035 | .03 | [−.30, −.17] | −6.75 | <.001 |
| ΔWP × ΔPA | −0.005 | .002 | .01 | [−.01, −.001] | −3.25 | .001 |
| Δ in Interpersonal Stress (ΔIS) | 0.639 | .216 | .13 | [.22, 1.06] | 2.96 | .003 |
| ΔIS × ΔPA | −0.160 | .070 | .01 | [−.30, −.02] | −2.28 | .023 |
| Level 2 (df = 117) | ||||||
| Avg. Positive Affect (AvgPA) | −0.072 | .059 | --- | --- | −1.21 | .227 |
| Avg. Inter. Stress (AvgIS) | 0.575 | .094 | .11 | [.39, .76] | 6.15 | <.001 |
| Average Pain (AvgP) | 0.002 | .002 | --- | --- | 1.13 | .263 |
| Neuroticism | 0.206 | .046 | .07 | [.12, .30] | 4.44 | <.001 |
| Age | −0.004 | .004 | --- | --- | −1.02 | .311 |
| Diagnosis | −0.095 | .074 | --- | --- | −1.28 | .204 |
| Level 1 × Level 2 (df = 1038) | ||||||
| ΔWP × AvgPA | −0.005 | .001 | .11 | [−.01, −.003] | −3.83 | .001 |
| ΔIS × AvgPA | −0.132 | .068 | .16 | [−.27, .001] | −1.93 | .054 |
| ΔWP × AvgIS | −0.006 | .003 | .01 | [−.01, −1.2*10−4] | −2.42 | .016 |
| ΔIS × AvgIS | 0.332 | .116 | .03 | [.10, .56] | 2.87 | .004 |
Note. An autoregressive matrix was used to model the error variance on the dependent variable.
Individual differences in the average level of the weekly variables were also probed through analyses at Level 2. For these analyses, we focused on the individual differences in levels of pain, stress, and positive affect, reflected in the averaged scores of each of these variables for each participant across the 10 to 12 weekly interviews. In addition to these variables, diagnosis, age, and neuroticism were also added to further examine individual differences. These variables were used as predictors of variance in level 1 weekly negative affect (the Level 1 intercept: β0) and slopes of the relationships between deviation scores and NA (β1, β2 ,& β3 in the level 1 equation above).
The first Level 2 equation for this model was as follows:
Level 2: β0 = γ00 + γ01 average pain + γ02 average stress + γ03 average positive affect + γ04 age + γ05 diagnosis + γ06 neuroticism + u0
A second set of Level 2 equations tested for differences in slopes β1, β2, & β3 provided in the Level 1 equation reported above. Each of these equations provide for tests of interaction between individual differences on key variables and the influence of Level 1 variables on negative affect. For example, the test of individual differences in the relationship between pain and negative affect would be designated as:
Level 2: β1 = γ10 + γ11 average pain + γ12average stress + γ13 average positive affect + γ14age + γ15 diagnosis + γ16neuroticism + u1
In this equation the slope (β1) designates the estimated relationship between pain and negative affect for each participant. This variable is predicted by individual differences in average pain (γ11), average stress (γ12), average positive affect (γ13), age (γ14), etc. A separate equation (not shown) examines the parameter β3 (the slope of the relationship between stress and negative affect). The other specifications for this model were selected following Singer (Singer, 1998) to identify the best fitting model of the variances and covariances of the variables under study. The dependent variable was modeled as a random variable, and goodness of fit tests were employed to examine whether the weekly deviations in pain, interpersonal stress, and positive affect also varied randomly across participants. Week number, deviations in positive affect, and interpersonal stress showed significant random effects in the mixed models predicting negative affect. A first-order autoregressive variance-covariance matrix was chosen to model the within-subjects covariance on the dependent variable. The first-order autoregressive function models a linear relationship between adjacent scores and an exponential decay in that relationship, with increasing time between measures.
Results
Table 1 displays the means, SD's, and t-tests of differences on the variables under study for the two groups: OA and FMS participants. Both groups reported significant pain and moderately high negative affect, according to the PANAS-X norms (Watson & Clark, 1999). In our sample, FMS participants reported somewhat higher average pain than OA participants (approximately 10 points on a 0 to 100 numeric scale; t = −2.17, p < .05), higher interpersonal stress, marginally higher NA, and lower PA than the OA sample. The OA samples were older by an average of 6 years, and tended to report less neuroticism than the FMS group.
Table 1.
Scores on Study Variables for Participants with Osteoarthritis and Fibromyalgia on Key Weekly and Demographic Variables
| Osteoarthritis | Fibromyalgia | |||||
|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | t | p |
| Age | 59.38 | 9.13 | 52.76 | 7.21 | 4.31 | .0001 |
| Neuroticism | 2.93 | 0.81 | 3.38 | 0.76 | −2.94 | .004 |
| Avg. Pain | 48.30 | 19.32 | 55.75 | 16.71 | −2.17 | .032 |
| NA | 1.66 | 0.47 | 1.83 | 0.51 | −1.75 | .083 |
| PA | 3.16 | 0.55 | 2.78 | 0.58 | 3.36 | .001 |
| Interpersonal Stress | 0.44 | 0.40 | 0.60 | 0.34 | −2.23 | .027 |
Note. Age differences were controlled for in tests of differences between groups.
The findings for the prediction of weekly negative affect are shown in Table 2. All within-person predictors were significant: pain, positive affect, stress, stress × positive affect, and pain × positive affect. Negative affect was highest during weeks when pain was high, interpersonal stress was high, and positive affect was low. Further, the absence of positive affect showed its strongest association with negative affect during weeks of high pain and stress, as evidenced by the significant interactions between pain and positive affect, and stress and positive affect predicting negative affect (p's < .05). Table 2 also shows that weekly changes in positive affect and stress along with the intercept and the week of the assessment were modeled as random variables. Pain did not display significant random variation and was not modeled for random effects.
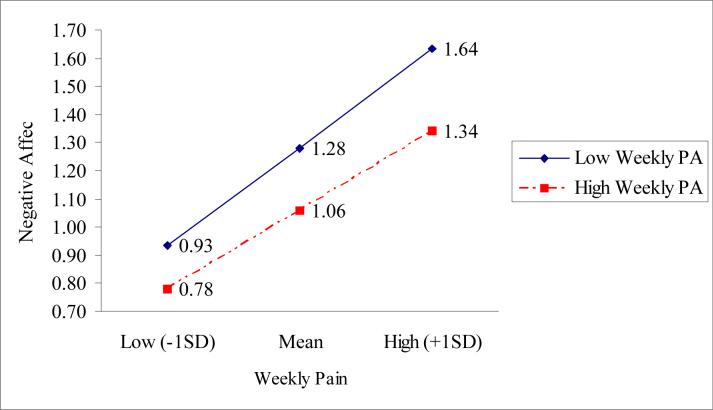
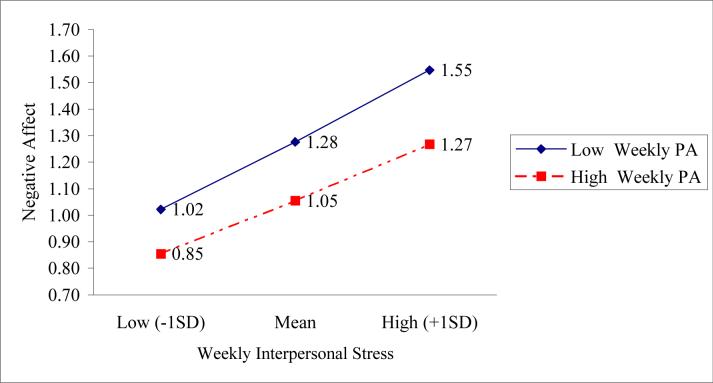
We summarized the findings of the significant interactions from two of the multilevel analyses in Figures 1 and 2 according to procedures outlined in Aiken and West (1991). The figures display how the relative absence of weekly positive affect interacts with pain and stress to increase levels of negative affect and may play an insidious role in a chronic pain disorder. As shown in Figures 1 and 2, a rise in positive affect not only lowers negative affect directly, but also blunts the effects of high pain and high interpersonal stress on negative affect.
Figure 1.
Interaction of weekly pain and weekly positive affect on negative affect
Figure 2.
Interaction of weekly interpersonal stress and weekly positive affect on negative affect
We next examined whether individual differences on key variables influenced these relationships through a series of analyses following the equations specified above for testing Level 2 effects. As expected, those participants lower in neuroticism, or who reported less stress overall also reported less negative affect from week to week (p's <.001).
Interactions between Level 2 variables and weekly covariations between stress, pain, and affect also revealed significant relationships. Individual differences in average positive affect showed some of the strongest effects. Participants with greater positive affect on average across the 10−12 weeks of interviews showed a muted rise in negative affect during high pain weeks (p < .01), or during weeks of higher interpersonal stress (p = .054) relative to those with lower average positive affect. These relationships were comparable to those presented in Figures 1 and 2 for weekly positive affect. In addition, participants who reported more interpersonal stress across weeks showed stronger elevations in negative affect during stressful weeks (p < .001). There was one counterintuitive finding; participants who tended to report more interpersonal stress did not appear to react as negatively to high pain weeks (p < .05). Finally, diagnosis, age, and the participant's average pain level did not influence the Level 1 relationships among the variables.
We next sought to determine whether weekly affect predicted reports of pain the following week. To test this model, Level 1 and Level 2 equations were examined using pain on the subsequent week as the criterion variable, controlling for pain on the prior week. We tested whether changes in negative and positive affect the prior week were predictors of future pain. The same control variables used in the prediction of negative affect were also used in this prediction equation. The effects of stress were also tested but were found to be nonsignificant.
The results from this analysis are shown in Table 3. An increase in negative affect the prior week predicted greater pain, as did the person's average negative affect. In addition, participants with relatively more positive affect averaged across the study weeks also were less likely to show increases in pain from week-to-week. Since greater pain led to higher levels of negative affect, especially when accompanied by low positive affect, the model posits a set of relationships that would sustain a cycle of increased pain and negative affect so frequently observed in chronic pain conditions. This cycle is driven, at least in part, by the more subtle influence of low positive affect, a condition that appears to occur more frequently in FMS in comparison to OA. Tables 2 and 3 also display effect sizes (r2) and 95% confidence intervals for all of the significant predictor variables. Effect sizes were computed by squaring the standardized beta values for each prediction.
Table 3.
Multilevel Regressions Predicting Pain the Following Week
| Random Effects | |||||
|---|---|---|---|---|---|
| Covariance Parameter Estimates | Subject | β | SE | Z | p |
| UN (1, 1) | ID | 221.84 | 37.18 | 5.97 | <.001 |
| AR (1) | ID | 0.34 | .07 | 4.56 | <.001 |
| Residual | . | 226.62 | 19.54 | 11.60 | <.001 |
| Fixed Effects | ||||||
|---|---|---|---|---|---|---|
| Predictor Variables | β | SE | r2 | 95% CI | t | p |
| Level 1 (df = 828) | ||||||
| Δ in Weekly Pain | −0.026 | .036 | --- | --- | −0.72 | .469 |
| Δ in Negative Affect | 2.457 | 1.100 | .003 | [.30, 4.61] | 2.23 | .026 |
| Δ in Positive Affect | 1.385 | 1.049 | --- | --- | 1.32 | .187 |
| Level 2 (df = 117) | ||||||
| Average Negative Affect | 7.215 | 3.152 | .03 | [1.04, 13.39] | 2.29 | .024 |
| Average Positive Affect | −7.612 | 2.623 | .04 | [−12.75, −2.47] | −2.90 | .004 |
Given that participants in the two pain groups had distinctly different profiles (See Table 1), we conducted tests of interactions between positive affect and negative affect with diagnosis to determine whether there were diagnostic differences between the relationships of the variables within our model. All of these interactions were not significant, indicating that positive affect did not interact with pain or stress to influence negative affect differently for the FMS group.
Discussion
In this study, we sought to expand upon previous work highlighting the role of positive affect in adaptation to pain, and also to examine the role of positive affect in moderating the effects of interpersonal stress and pain on negative affect (Zautra, Berkhof, & Nicolson, 2002; Zautra, et al., 2001). Our aim was to examine empirical support for two complementary models. Each model addresses how positive emotions may benefit someone in chronic pain, and how the absence of positive affect during times of stress may be particularly troublesome. Fredrickson's “broaden and build” model (Fredrickson & Joiner, 2002) predicted that people with more positive affect overall would adapt more readily during times of stress. The second model emphasized the dynamic quality of the relationships between positive and negative affect, predicting that during times of stress, higher positive affect would also be associated with less negative affect as a consequence of increasing bipolarity of these affective states.
We found evidence for both models, broadening the applicability of both. People with greater average positive affect were less likely to show higher negative affect during high pain weeks, and during weeks characterized by high levels of interpersonal conflict. These findings are consistent with the interpretation that high positive affect characterized those participants who were more resilient in the face of both increased bodily pain and mounting interpersonal conflict.
The data also were consistent with a dynamic view of affect relationships. During weeks when pain was elevated, high positive affect during that same week was more highly associated with low negative affect. These relationships were found over and above the findings for average levels of stress and positive affect. The relationship may also be stated in the negative to reveal the potential vulnerability that low positive affect engenders. When positive affect is low at the same time that pain or stress are elevated, people are much more likely to experience negative affective states than with either condition alone. These effects appear to be multiplicative rather than additive.
Support for both of these models does not diminish the importance of interpersonal stress and pain as threats to the regulation of negative emotion. Both variables had a significant association with higher negative affect. However, from these data, a model for understanding the development of chronic pain conditions should rely not only on sources of stress, but also on failures of resilience that may arise from a relative deficit of positive emotional resources. Stating the problem in these terms provides greater specificity to the claim that chronic pain conditions, such as FMS, may involve failures of emotion-regulation, specifically in individuals’ ability to reduce negative affect and also mount positive affect. However, the standard approach to identifying emotional difficulties through the study of personality factors such as neuroticism may be called into question based on these data. The deficit appears to be more apparent in the relative absence of positive affective resources, rather than a surfeit of negative affect.
This study found evidence primarily of relationships among variables from assessments taken at the same time, limiting the scope of the inferences we can make about positive affect's causal role. Nonetheless the robust patterns of relationships, showing beneficial outcomes relating to both having greater average positive affect and having positive affect during times of pain and stress invites further inquiry with measures taken closer in time than week-to-week. Diary studies, which assess key variables daily or even more frequently, would permit the evaluation of lagged relationships over a briefer interval, permitting the testing of competing causal orders that may underlie the relationships uncovered here.
The effects over time that we did observe from one week to the next were consistent with a model of an indirect link between positive affect and generalized pain disorders, mediated through negative affect. The results indicated that elevations in negative affect appeared to lead to greater pain reports during the subsequent week. The lagged effects of negative affect on pain the following week were not strong, however. Although people who tended to have higher levels of positive affect also had less pain week-to-week, decreases in positive affect one week were not followed reliably by increases in pain the next week. These data point to the need for further research on how affective states evolve over time to influence one another and key health outcomes such as pain and disablement.
One important set of null findings deserves additional comment. Although we found differences between FMS and OA samples on levels of positive affect, we found no evidence that the weekly relationships among the study variables were different between groups. Positive affect was not more or less correlated with pain, negative affect, or stress, and positive affect did not interact with pain and stress to influence negative affect differently for FMS patients compared to OA patients. Apparently, positive affect, when present, is a resource of comparable value for both groups.
The sample drawn for this study is biased in favor of European-American women with slightly higher income and education than average in the population of women. Further, we purposefully selected only women 35 years of age and older so that our participants with FMS would be similar in age to those with OA. These constraints on representativeness of the sample raise some questions about the generalizability of the findings to younger people, men, and those in lower income and ethnic minority groups.
These findings are valuable from several perspectives. First, these results promote further inquiry of the process of both models regarding positive affect as a source of resilience to pain and stress. Second, the relative absence of positive affect in FMS along with evidence of the importance of this set of emotions for well-being among both chronic pain populations studied here urges further research on the determinants of positive affect in healthy and chronically ill populations. Positive affect is known to be fairly stable over time but also to be influenced by everyday life events (Potter, Zautra, & Reich, 2000; Zautra, Berkhof, & Nicolson, 2002; Zautra, Reich, Davis, Potter, & Nicolson, 2000). We do not know whether the positive affect deficits we have observed among those with FMS are best characterized as trait or state, or some combination of both. Fatigue may also play an important role as a cause and a consequence of lower positive affect in chronic pain syndromes, as well. Further work is needed in identifying the factors associated with low levels of positive affect in these populations.
If the ability to sustain positive affect protects against increases in negative affect during times of increased pain or stress, then intervention efforts directed at enhancing individuals’ ability to process affect with greater complexity may prove useful. One such approach, centering on the use of mindfulness meditation, has been garnering empirical support over the past decade in the treatment of pain and prevention of depression relapse (Kabat-Zinn, Lipworth, & Burney, 1985; Segal, Williams, & Teasdale, 2002; Teasdale, Moore, Hayhurst, Pope, Williams, & Segal, 2002). In contrast to the automatic processing that occurs during pain and other stressors, mindfulness fosters effortful processing of mental events by increasing conscious attention to and nonjudgmental acceptance of thoughts and feelings. The goal is to develop the ability to recognize negative thoughts, feelings, and sensations as momentary objects of awareness, and to acknowledge that thoughts are not facts but rather interpretations of events that reflect a variety of influences, including past learning and current mood states. An optimal outgrowth of such an approach for those in chronic pain would be an increase in their emotional complexity, such that they would be able to sustain access to positive affective resources even when they encounter difficult or painful experiences.
In sum, the results support a model where average positive affect and positive affect during the same week affect the relationship of both pain and interpersonal stress to negative affect. Specifically, deficits in positive affect were related to increased negative affect during times of high stress and high pain. These elevations in negative affect predicted an increase in pain during subsequent weeks. Future research is needed to provide evidence of how a cycle of pain and distress is maintained, particularly for patients with few positive affective resources.
Acknowledgements
This research was supported by a grant from the Arthritis Foundation (Principal Investigator: Alex J. Zautra, PhD).
References
- Affleck G, Urrows S, Tennen H, Higgins P, Pav D, Aloisi R. A dual pathway model of daily stressor effects on rheumatoid arthritis. Annals of Behavioral Medicine. 1997;19(2):161–170. doi: 10.1007/BF02883333. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- Beckham JC, Keefe FJ, Caldwell DS, Roodman AA. Pain coping strategies in rheumatoid arthritis: Relationships to pain, disability, depression, and daily hassles. Behavior Therapy. 1991;22(1):113–124. [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:227–234. [Google Scholar]
- Davis MC, Matthews KA, Twamley EW. Is life more difficult on Mars or Venus? A meta-analytic review of sex differences in major and minor life events. Annals of Behavioral Medicine. 1999;21(1):83–97. doi: 10.1007/BF02895038. [DOI] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, Reich JW. Vulnerability to stress among women in chronic pain from fibromyalgia and osteoarthritis. Annals of Behavioral Medicine. 2001;23(3):215–226. doi: 10.1207/S15324796ABM2303_9. [DOI] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, Smith B. Chronic pain, stress, and the dynamics of affective differentiation. Journal of Personality. doi: 10.1111/j.1467-6494.2004.00293.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychol Sci. 2002;13(2):172–175. doi: 10.1111/1467-9280.00431. [DOI] [PubMed] [Google Scholar]
- Geisser ME, Casey KL, Brucksch CB, Ribbens CM, Appleton BB, Crofford LJ. Perception of noxious and innocuous heat stimulation among health women and women with fibromyalgia: association with mood, somatic focus, and catastrophizing. Pain. 2003;102(3):243–250. doi: 10.1016/S0304-3959(02)00417-7. [DOI] [PubMed] [Google Scholar]
- Hawley DJ, Wolfe F. Depression is not more common in rheumatoid arthritis: A 10-year longitudinal study of 6,153 patients with rheumatic disease. The Journal of Rheumatology. 1993;20:2025–2031. [PubMed] [Google Scholar]
- Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist. 1989;44:513–524. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Pope HG. Is fibromyalgia a form of “affective spectrum disorder?”. Journal of Rheumatology. 1989;19:15–22. [PubMed] [Google Scholar]
- Hudson JI, Pope HG. Affective spectrum disorder: Does antidepressant response identify a family of disorders with common pathophysiology? American Journal of Psychiatry. 1990;147:552–564. doi: 10.1176/ajp.147.5.552. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: A comparison of six methods. Pain. 1988;27(1):117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- John OP, Donahue EM, Kentle RL. The “Big Five” Inventory - Versions 4a and 54. University of California, Berkeley, Institute of Personality and Social Research; Berkeley: 1991. [Google Scholar]
- Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine. 1985;8:163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for linear mixed models. SAS Institute; Cary, NC: 1996. [Google Scholar]
- Okifuji A, Turk DC, Sinclair JD, Starz TW, Marcus DA. A standardized manual tender point survey. I. Development and determination of a threshold point for the identification of positive tender points in Fibromyalgia Syndrome. The Journal of Rheumatology. 1997;24(2):377–383. [PubMed] [Google Scholar]
- Potter PT, Zautra AJ, Reich JW. Stressful events and information processing dispositions moderate the relationship between positive and negative affect: Implications for pain patients. Annals of Behavioral Medicine. 2000;22(3):191–198. doi: 10.1007/BF02895113. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JM, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Guilford Press; New York: 2002. [Google Scholar]
- Singer JD. Using SAS PROC MIXED to fit multilevel models hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;24(4):323–355. [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70:275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Affects separable and inseparable: On the hierarchical arrangement of the negative affects. Journal of Personality and Social Psychology. 1992;62(3):489–505. [Google Scholar]
- Watson D, Clark LA. The PANAS-X manual for the positive and negative affect schedule--Expanded form. [September, 24, 2003];1999 from the University of Iowa Web Site: http://www.psychology.uiowa.edu/Faculty/Watson/PANAS-X.pdf.
- Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology criteria for the classification of Fibromyalgia. Arthritis and Rheumatism. 1990;33(2):160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Berkhof J, Nicolson NA. Changes in affect interrelations as a function of stressful events. Cognition and Emotion. 2002;16(2):309–318. [Google Scholar]
- Zautra AJ, Burleson MH, Smith CA, Blalock SJ, Wallston KA, DeVellis RF, DeVellis BM, Smith TW. Arthritis and perceptions of quality of life: An examination of positive and negative affect in rheumatoid arthritis patients. Health Psychology. 1995;14(5):399–408. doi: 10.1037//0278-6133.14.5.399. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Hamilton N, Burke HM. Comparison of stress responses in women with two types of chronic pain: Fibromyalgia and Osteoarthritis. Cognitive Therapy and Research. 1999;23:209–230. [Google Scholar]
- Zautra AJ, Reich JW, Davis MC, Potter PT, Nicolson NA. The role of stressful events in the relationship between positive and negative affects: Evidence from field and experimental studies. Journal of Personality. 2000;68(5):927–951. doi: 10.1111/1467-6494.00121. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Reich JW, Guarnaccia CA. Some everyday life consequences of disability and bereavement for older adults. Journal of Personality and Social Psychology. 1990;59(3):550–561. doi: 10.1037//0022-3514.59.3.550. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Smith BW. Depression and reactivity to stress in older women with rheumatoid arthritis and osteoarthritis. Psychosomatic Medicine. 2001;63:687–696. doi: 10.1097/00006842-200107000-00022. [DOI] [PubMed] [Google Scholar]
- Zautra A, Smith B, Affleck G, Tennen H. Examinations of chronic pain and affect relationships: applications of a dynamic model of affect. Journal of Consulting and Clinical Psychology. 2001;69(5):786–795. doi: 10.1037//0022-006x.69.5.786. [DOI] [PubMed] [Google Scholar]