Abstract
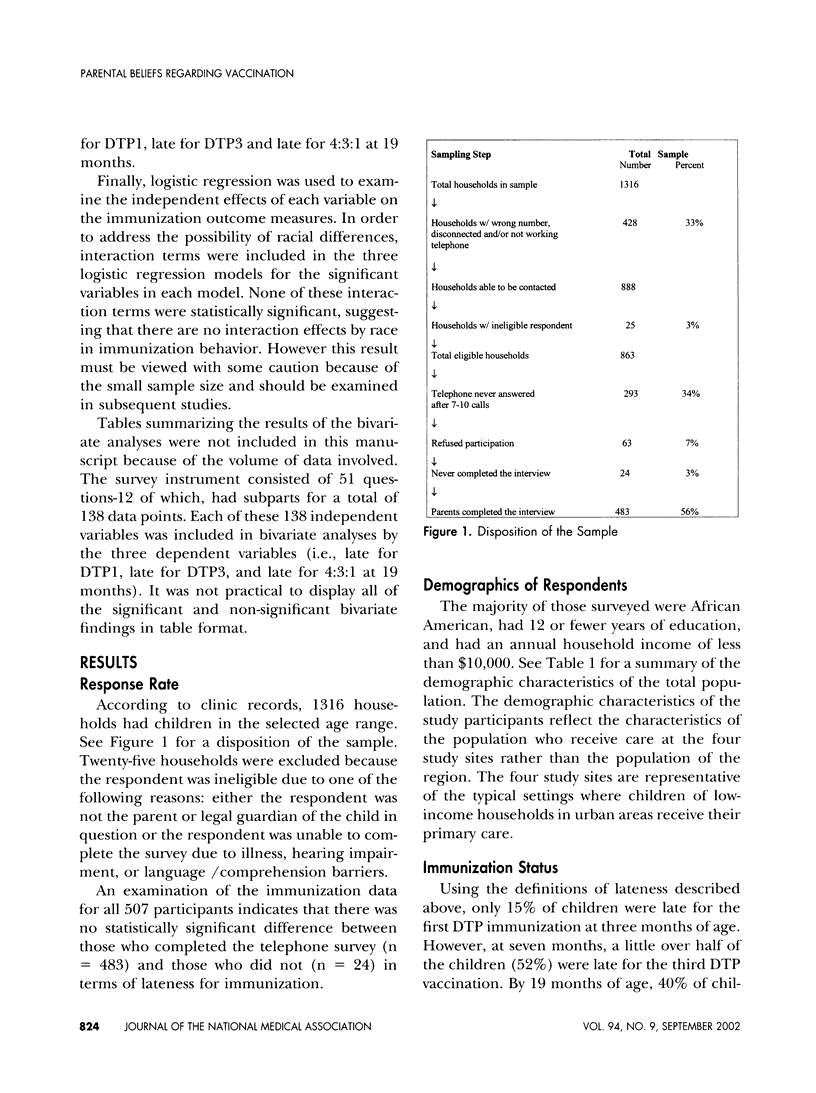
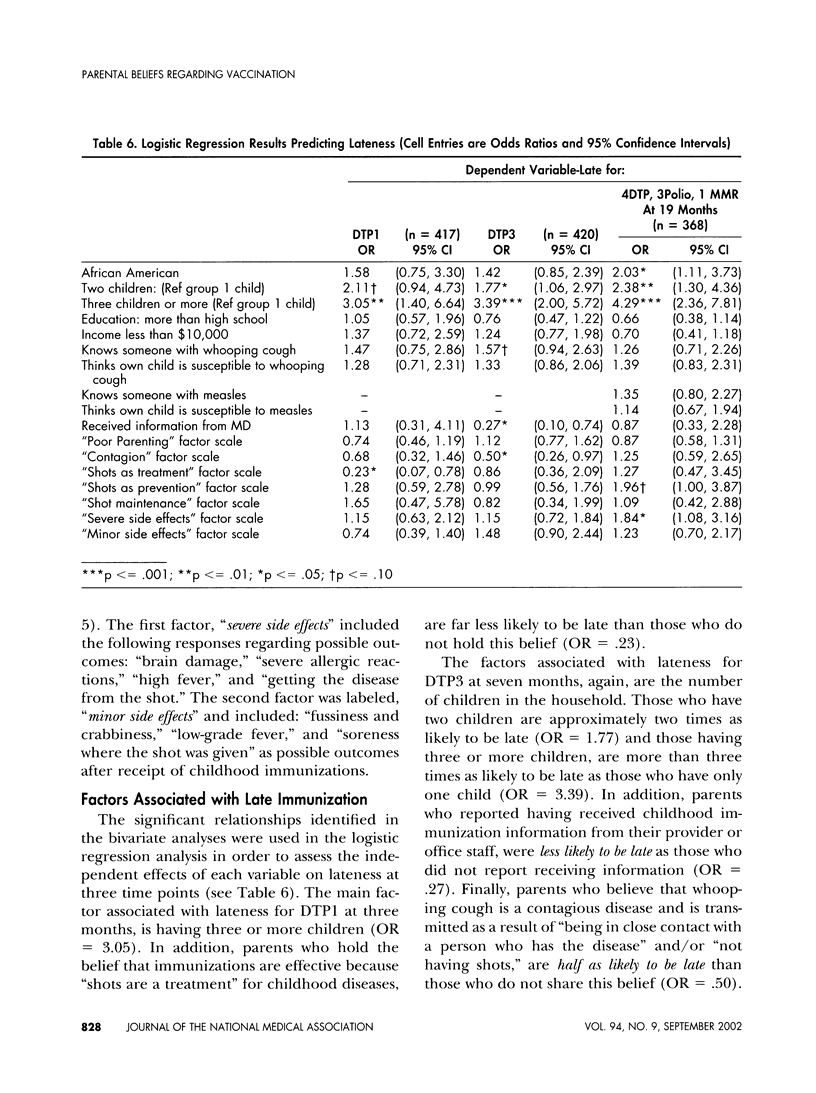
OBJECTIVE: The objective of this study was to understand how low income, inner-city parents of preschool children think about childhood diseases and prevention and the impact that this has on late receipt of vaccines. METHODS: Parents of all children born between January 1, 1991, and May 31, 1995, whose child received medical assistance and health care at one of four inner-city, primary care clinics in Pittsburgh, PA, completed a telephone interview and gave consent for a vaccine record review. The main outcome measures were lateness for first and third diphtheria and tetanus toxoids and pertussis vaccines (DTP) and not receiving at least four DTP, three polio virus containing and one measles, mumps and rubella (MMR) doses by 19 months. RESULTS: A total of 483 parents participated. Fifteen percent of children were late for the first DTP, 52% for the third DTP, and 40% had not received at least four DTP, three polio and one MMR by 19 months of age. Statistically significant factors associated with lateness at 19 months included: having three or more children, having two children, beliefs regarding the severity of immunization side effects, and being African American. CONCLUSIONS: The results of this study indicate that a combination of life circumstances, as well as cognitive factors were associated with late immunization.
Full text
PDF





Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bates A. S., Fitzgerald J. F., Dittus R. S., Wolinsky F. D. Risk factors for underimmunization in poor urban infants. JAMA. 1994 Oct 12;272(14):1105–1110. [PubMed] [Google Scholar]
- Bobo J. K., Gale J. L., Thapa P. B., Wassilak S. G. Risk factors for delayed immunization in a random sample of 1163 children from Oregon and Washington. Pediatrics. 1993 Feb;91(2):308–314. [PubMed] [Google Scholar]
- Cutts F. T., Orenstein W. A., Bernier R. H. Causes of low preschool immunization coverage in the United States. Annu Rev Public Health. 1992;13:385–398. doi: 10.1146/annurev.pu.13.050192.002125. [DOI] [PubMed] [Google Scholar]
- Freeman T. R., Bass M. J. Determinants of maternal tolerance of vaccine-related risks. Fam Pract. 1992 Mar;9(1):36–41. doi: 10.1093/fampra/9.1.36. [DOI] [PubMed] [Google Scholar]
- Gellin B. G., Maibach E. W., Marcuse E. K. Do parents understand immunizations? A national telephone survey. Pediatrics. 2000 Nov;106(5):1097–1102. doi: 10.1542/peds.106.5.1097. [DOI] [PubMed] [Google Scholar]
- Guyer B., Hughart N., Holt E., Ross A., Stanton B., Keane V., Bonner N., Dwyer D. M., Cwi J. S. Immunization coverage and its relationship to preventive health care visits among inner-city children in Baltimore. Pediatrics. 1994 Jul;94(1):53–58. [PubMed] [Google Scholar]
- Lannon C., Brack V., Stuart J., Caplow M., McNeill A., Bordley W. C., Margolis P. What mothers say about why poor children fall behind on immunizations. A summary of focus groups in North Carolina. Arch Pediatr Adolesc Med. 1995 Oct;149(10):1070–1075. doi: 10.1001/archpedi.1995.02170230024003. [DOI] [PubMed] [Google Scholar]
- Melman S. T., Chawla T., Kaplan J. M., Anbar R. D. Multiple immunizations. Ouch! Arch Fam Med. 1994 Jul;3(7):615–618. doi: 10.1001/archfami.3.7.615. [DOI] [PubMed] [Google Scholar]
- Prislin R., Dyer J. A., Blakely C. H., Johnson C. D. Immunization status and sociodemographic characteristics: the mediating role of beliefs, attitudes, and perceived control. Am J Public Health. 1998 Dec;88(12):1821–1826. doi: 10.2105/ajph.88.12.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salsberry P. J., Nickel J. T., Mitch R. Why aren't preschoolers immunized? A comparison of parents' and providers' perceptions of the barriers to immunizations. J Community Health Nurs. 1993;10(4):213–224. doi: 10.1207/s15327655jchn1004_2. [DOI] [PubMed] [Google Scholar]
- Schaffer S. J., Szilagyi P. G. Immunization status and birth order. Arch Pediatr Adolesc Med. 1995 Jul;149(7):792–797. doi: 10.1001/archpedi.1995.02170200082013. [DOI] [PubMed] [Google Scholar]
- Strobino D., Keane V., Holt E., Hughart N., Guyer B. Parental attitudes do not explain underimmunization. Pediatrics. 1996 Dec;98(6 Pt 1):1076–1083. [PubMed] [Google Scholar]
- Weinstein N. D. The precaution adoption process. Health Psychol. 1988;7(4):355–386. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- Williams I. T., Dwyer D. M., Hirshorn E. M., Bonito R. C., Graham N. M. Immunization coverage in a population-based sample of Maryland children. Arch Pediatr Adolesc Med. 1994 Apr;148(4):350–356. doi: 10.1001/archpedi.1994.02170040016003. [DOI] [PubMed] [Google Scholar]
- Wood D., Donald-Sherbourne C., Halfon N., Tucker M. B., Ortiz V., Hamlin J. S., Duan N., Mazel R. M., Grabowsky M., Brunell P. Factors related to immunization status among inner-city Latino and African-American preschoolers. Pediatrics. 1995 Aug;96(2 Pt 1):295–301. [PubMed] [Google Scholar]


