Abstract
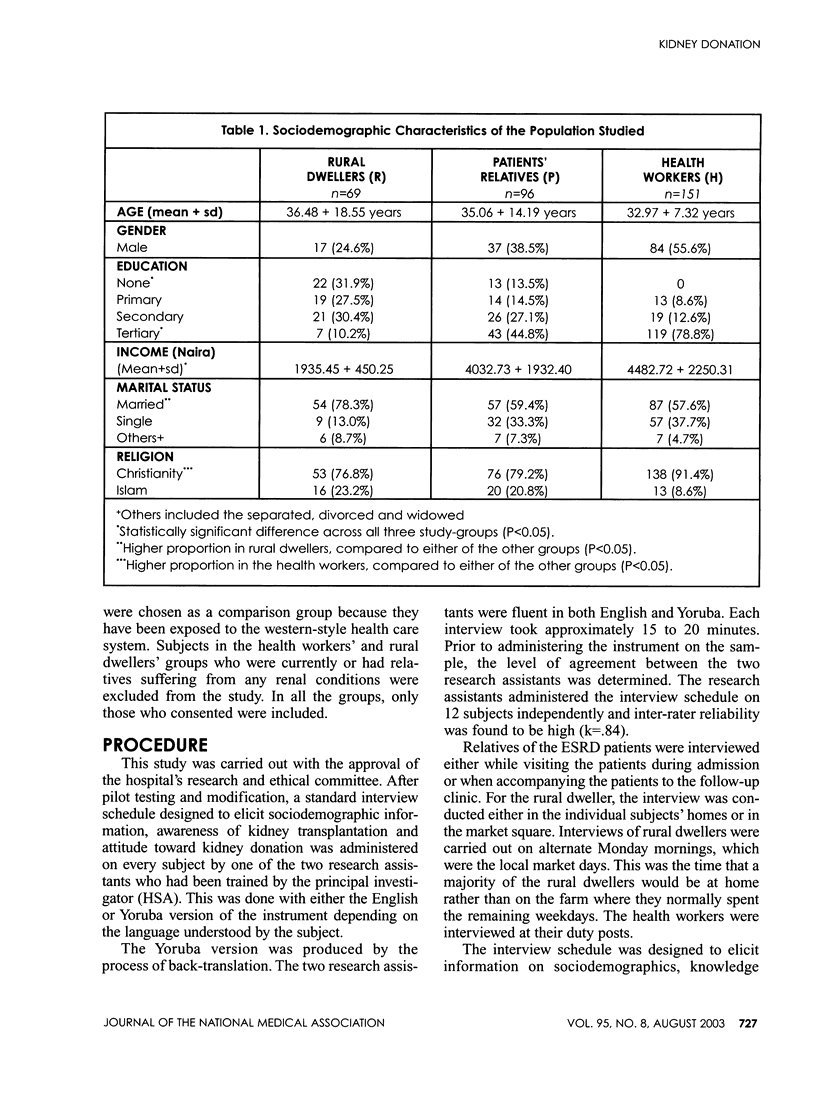
The Renal Unit of Obafemi Awolowo University Teaching Hospital Ile-Ife in Southwest Nigeria intends commencing a kidney transplantation program. This cross-sectional study aimed at examining the willingness of Nigerians to be living-related kidney donors. Three hundred and sixteen Nigerians (96 first-degree relatives of end-stage renal disease patients, 69 rural dwellers and 151 health workers) were interviewed regarding their willingness to donate kidneys using an interview schedule designed to elicit socio-demographic information, knowledge about kidney transplantation and attitude toward kidney donation. Sixty-two percent of health workers, 52.1% of the patients' relatives and 27.1% of rural dwellers expressed willingness to donate. Higher proportions of health workers and patients' relatives--compared with the rural dwellers--were willing to donate a kidney to their children, full-siblings and parents (P<0.05). The level of awareness about kidney transplantation was highest among health workers and least among rural dwellers (P<0.001). Altruism was the primary motivation for those willing to donate a kidney. The most important reason for refusal to donate was fear of adverse health consequences. Among the rural dwellers, never-married persons were more willing than the married to donate (P<0.05). Programs aimed at increasing awareness about the safety of kidney donation, reducing adverse beliefs about kidney donation, and encouraging altruistic tendencies will increase the availability of kidney donors.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aghanwa H. S., Morakinyo O. Psychiatric complications of hemodialysis at a kidney center in Nigeria. J Psychosom Res. 1997 May;42(5):445–451. doi: 10.1016/s0022-3999(96)00360-1. [DOI] [PubMed] [Google Scholar]
- Akinsola W., Odesanmi W. O., Ogunniyi J. O., Ladipo G. O. Diseases causing chronic renal failure in Nigerians--a prospective study of 100 cases. Afr J Med Med Sci. 1989 Jun;18(2):131–137. [PubMed] [Google Scholar]
- Barsoum Rashad S. Renal transplantation in a developing country: the Egyptian 17 year experience. . Afr J Health Sci. 1994 Feb;1(1):30–36. [PubMed] [Google Scholar]
- Beekman G. M., van Dorp W. T., van Es L. A., van Bockel J. H., van Saase J. L., van der Woude F. J., Valentijn R. M. Analysis of donor selection procedure in 139 living-related kidney donors and follow-up results for donors and recipients. Nephrol Dial Transplant. 1994;9(2):163–168. [PubMed] [Google Scholar]
- Beer J. Body image of patients with ESRD and following renal transplantation. 1995 May 25-Jun 7Br J Nurs. 4(10):591–598. doi: 10.12968/bjon.1995.4.10.591. [DOI] [PubMed] [Google Scholar]
- Bia M. J., Ramos E. L., Danovitch G. M., Gaston R. S., Harmon W. E., Leichtman A. B., Lundin P. A., Neylan J., Kasiske B. L. Evaluation of living renal donors. The current practice of US transplant centers. Transplantation. 1995 Aug 27;60(4):322–327. doi: 10.1097/00007890-199508270-00003. [DOI] [PubMed] [Google Scholar]
- Boulware L. Ebony, Ratner Lloyd E., Sosa Julie Ann, Tu Alexander H., Nagula Satish, Simpkins Christopher E., Durant Raegan W., Powe Neil R. The general public's concerns about clinical risk in live kidney donation. Am J Transplant. 2002 Feb;2(2):186–193. doi: 10.1034/j.1600-6143.2002.020211.x. [DOI] [PubMed] [Google Scholar]
- Canaud B., Mion C. Place de la dialyse péritonéale continue ambulatoire (DPCA) au sein d'un programme de traitement de l'insuffisance rénale chronique. Problèmes poséses par les transferts de DPCA en transplantation ou en hémodialyse. Nephrologie. 1995;16(1):129–135. [PubMed] [Google Scholar]
- Creecy R. F., Wright R., Berg W. E. Discriminators of willingness to consider cadaveric kidney donation among black Americans. Soc Work Health Care. 1992;18(1):93–105. doi: 10.1300/j010v18n01_06. [DOI] [PubMed] [Google Scholar]
- Gibson V. The factors influencing organ donation: a review of the research. J Adv Nurs. 1996 Feb;23(2):353–356. doi: 10.1111/j.1365-2648.1996.tb02678.x. [DOI] [PubMed] [Google Scholar]
- Gokal R. Quality of life in patients undergoing renal replacement therapy. Kidney Int Suppl. 1993 Feb;40:S23–S27. [PubMed] [Google Scholar]
- Grenier C. E., Joseph A. S. Louisiana neurosurgeons and the organ procurement shortage: a comparative analysis of perceptions, attitudes, and ethical values. J La State Med Soc. 1995 Oct;147(10):465–471. [PubMed] [Google Scholar]
- Hillebrand G. F., Land W. Renal transplantation: progress and prospects. Artif Organs. 1996 May;20(5):403–407. doi: 10.1111/j.1525-1594.1996.tb04523.x. [DOI] [PubMed] [Google Scholar]
- Kasiske B. L., Ma J. Z., Louis T. A., Swan S. K. Long-term effects of reduced renal mass in humans. Kidney Int. 1995 Sep;48(3):814–819. doi: 10.1038/ki.1995.355. [DOI] [PubMed] [Google Scholar]
- Lawry K. W., Brouhard B. H., Cunningham R. J. Cognitive functioning and school performance in children with renal failure. Pediatr Nephrol. 1994 Jun;8(3):326–329. doi: 10.1007/BF00866349. [DOI] [PubMed] [Google Scholar]
- Mitzel Heather, Snyders Michele. Anonymous donation: a transplant center's experience. Nephrol Nurs J. 2002 Jun;29(3):275–277. [PubMed] [Google Scholar]
- Ndlovu S. R., Kobryn A., Modiba M. C. Attitudes of black South Africans concerning organ donation. J Transpl Coord. 1998 Dec;8(4):241–242. doi: 10.7182/prtr.1.8.4.k310u6n837433540. [DOI] [PubMed] [Google Scholar]
- Oyediran A. B., Akinkugbe O. O. Chronic renal failure in Nigeria. Trop Geogr Med. 1970 Mar;22(1):41–44. [PubMed] [Google Scholar]
- Procci W. R., Hoffman K. I., Chatterjee S. N. Sexual functioning of renal transplant recipients. J Nerv Ment Dis. 1978 Jun;166(6):402–407. doi: 10.1097/00005053-197806000-00003. [DOI] [PubMed] [Google Scholar]
- Sanner M. Attitudes toward organ donation and transplantation. A model for understanding reactions to medical procedures after death. Soc Sci Med. 1994 Apr;38(8):1141–1152. doi: 10.1016/0277-9536(94)90229-1. [DOI] [PubMed] [Google Scholar]
- Siminoff L. A., Arnold R. M., Caplan A. L., Virnig B. A., Seltzer D. L. Public policy governing organ and tissue procurement in the United States. Results from the National Organ and Tissue Procurement Study. Ann Intern Med. 1995 Jul 1;123(1):10–17. doi: 10.7326/0003-4819-123-1-199507010-00037. [DOI] [PubMed] [Google Scholar]
- Slama H., Fisch H. U., Frey F. J. Quantitative Erfassung der Lebensqualität bei Patienten mit einer Nierenersatztherapie. Schweiz Rundsch Med Prax. 1993 Nov 2;82(44):1253–1262. [PubMed] [Google Scholar]
- Spital A. Do U.S. transplant centers encourage emotionally related kidney donation? Transplantation. 1996 Feb 15;61(3):374–377. doi: 10.1097/00007890-199602150-00007. [DOI] [PubMed] [Google Scholar]
- Spital A. Mandated choice for organ donation: time to give it a try. Ann Intern Med. 1996 Jul 1;125(1):66–69. doi: 10.7326/0003-4819-125-1-199607010-00010. [DOI] [PubMed] [Google Scholar]
- Woo K. T. Social and cultural aspects of organ donation in Asia. Ann Acad Med Singapore. 1992 May;21(3):421–427. [PubMed] [Google Scholar]