Abstract
Objective
Reactive hyperemia is the compensatory increase in blood flow that occurs after a period of tissue ischemia, and this response is blunted in patients with cardiovascular risk factors. The predictive value of reactive hyperemia for cardiovascular events in patients with atherosclerosis and the relative importance of reactive hyperemia compared with other measures of vascular function have not been previously studied.
Methods and Results
We prospectively measured reactive hyperemia and brachial artery flow-mediated dilation by ultrasound in 267 patients with peripheral arterial disease referred for vascular surgery (age 66±11 years, 26% female). Median follow-up was 309 days (range 1 to 730 days). Fifty patients (19%) had an event, including cardiac death (15), myocardial infarction (18), unstable angina (8), congestive heart failure (6), and nonhemorrhagic stroke (3). Patients with an event were older and had lower hyperemic flow velocity (75±39 versus 95±50 cm/s, P=0.009). Patients with an event also had lower flow-mediated dilation (4.5±3.0 versus 6.9±4.6%, P<0.001), and when these 2 measures of vascular function were included in the same Cox proportional hazards model, lower hyperemic flow (OR 2.7, 95% CI 1.2 to 5.9, P=0.018) and lower flow-mediated dilation (OR 4.2, 95% CI: 1.8 to 9.8, P=0.001) both predicted cardiovascular events while adjusting for other risk factors.
Conclusions
Thus, lower reactive hyperemia is associated with increased cardiovascular risk in patients with peripheral arterial disease. Furthermore, flow-mediated dilation and reactive hyperemia incrementally relate to cardiovascular risk, although impaired flow-mediated dilation was the stronger predictor in this population. These findings further support the clinical relevance of vascular function measured in the microvasculature and conduit arteries in the upper extremity.
Keywords: endothelium, cardiovascular risk, surrogate markers, reactive hyperemia, flow-mediated dilation
Reactive hyperemia is a complex response that occurs after a period of tissue ischemia and primarily depends on local production of adenosine and other non–endothelium-dependent vasodilators that dilate tissue microvessels.1 Studies in humans have shown that endothelium-derived nitric oxide also contributes to reactive hyperemia.2,3 Peak brachial artery hyperemic flow velocity after 5-minute cuff occlusion of the arm relates inversely to traditional cardiovascular disease risk factors4 and to markers of inflammation5 in the Framingham Heart Study. Smaller scale mechanistic studies suggest that the nitric oxide–dependent component of reactive hyperemia may be particularly affected by risk factors.3 The relation of reactive hyperemia to the incidence of cardiovascular disease events in atherosclerosis has not been previously studied.
We previously demonstrated that brachial artery flow-mediated dilation, a measure of conduit artery endothelial vasodilator function, relates inversely to cardiovascular disease events in a high-risk cohort of patients with peripheral arterial disease.6 In the present study, we related peak hyperemic flow velocity in the brachial artery, a measure of microvascular function, to cardiovascular events in a larger cohort that included subjects from our previous study. Because reactive hyperemia is the stimulus for flow-mediated dilation and has been suggested to explain in large part the relationship between flow-mediated dilation and cardiovascular disease,4,7 we examined the relative predictive value of both of these measures of vascular function for cardiovascular events.
Methods
Study Subjects
Patients with peripheral artery disease undergoing nonemergent vascular surgery between November 1998 and May 2006 were eligible for participation. Patients were excluded if they had recent (up to 1 month) history of unstable angina, myocardial infarction, coronary revascularization, stroke, or decompensated heart failure. We previously reported the relation between flow-mediated dilation and long-term outcomes in 185 patients from this cohort.6 Since that time, we consecutively recruited an additional 82 subjects yielding a total of 267 patients in the present report, which examined the relation between reactive hyperemia and cardiovascular events. All participants provided written informed consent as approved by Boston Medical Center Institutional Review Board.
Preoperative Assessment
Study personnel prospectively reviewed medical records and interviewed each subject to determine clinical characteristics including age, gender, and ethnicity, and clinical history of coronary artery disease, congestive heart failure, cigarette smoking, diabetes mellitus, hypertension, and hypercholesterolemia. We also recorded lipid values, complete blood count, and serum creatinine when available from the medical record.
Up to 1 month before surgery, brachial artery flow-mediated dilation and reactive hyperemia were assessed by ultrasound using an established and standardized method.8,9 Briefly, patients were studied after at least a 6-hour fast and were asked to refrain from smoking overnight before study. Two-dimension ultrasound images of the conduit brachial artery were recorded before and 1 minute after induction of reactive hyperemia by 5-minute cuff occlusion of the upper arm. Doppler flow signals were recorded at baseline and for 15 seconds after cuff release to identify peak reactive hyperemia. After a 10-minute rest to allow return of brachial diameter and flow to the basal state, 2-dimensional images of the brachial artery were recorded before and 3 minutes after a 0.4 mg sublingual dose of nitroglycerin in a subset of patients. The nitroglycerin portion of the study was omitted if the patient declined or had previous adverse reactions to nitroglycerin, history of migraine headache, critical carotid stenosis, systolic blood pressure less than 100 mm Hg, or use of a sildenafil, tadalafil, or vardenafil within 1 week of the study. All images were digitized online and analyzed using customized software (Medical Imaging Applications Inc) in a blinded manner. Baseline and hyperemic flows were expressed as flow velocity measured by ultrasound and as flow volume calculated from peak flow velocity and vessel cross-sectional area. Flow-mediated dilation was expressed as percentage change from baseline and as the actual change from baseline expressed in millimeters. Brachial artery shear stress was calculated as 8μV/diameter, where μ is blood viscosity (assumed to be 0.035 dyne-sec/cm2) and V is brachial velocity at baseline or at peak hyperemia.
Reproducibility for measurement of flow-mediated dilation is well established and has been previously reported for our laboratory.10 To assess reproducibility of the primary end point of this study, the same ultrasonographer analyzed hyperemic flow velocity 5 separate times in 64 patients, and the intraobserver coefficient of variation was 2.8%. When hyperemic flow was measured on 2 separate occasions in a group of 65 patients with coronary artery disease, the coefficient of variation was 15.5%.
Follow-Up and Assessment of Cardiovascular Events
Patients were monitored for cardiovascular events beginning the day of surgery for up to 2 years. We prospectively measured serum troponin and obtained an ECG after surgery to ascertain postoperative myocardial infarction. After hospital discharge, patients were then contacted by telephone 30 days and every 6 months after surgery to obtain event information. If an event had occurred, medical records were obtained and the presence or absence of a cardiovascular event was adjudicated by a committee of 3 cardiologists, as previously described.6,11 The events included cardiovascular death, myocardial infarction, unstable angina, decompensated heart failure, and nonhemorrhagic stroke. The first event in each patient was included in the analysis.
Statistical Analysis
We grouped the study subjects according to the presence or absence of a cardiovascular event and compared clinical characteristics and vascular function for the 2 groups using the chi-square test for categorical variables and the Student t test or the Mann–Whitney test for continuous variables that had a normal or skewed distribution, respectively.
We completed Kaplan–Meier analysis to examine the relation between reactive hyperemia or flow-mediated dilation and event-free survival. When a subject had more than 1 event, we considered only the time to the first event. In these analyses, we categorized hyperemia as tertile of peak hyperemic flow velocity and flow-mediated dilation as tertile of flow-mediated dilation expressed as percent of baseline.6,11 We also completed forward conditional Cox regression analyses to determine whether reactive hyperemia and flow-mediated dilation were multivariable predictors of events while adjusting for baseline variables that had a probability value less than 0.10 in the univariable analysis (Table 1), including age, gender, diabetes mellitus, serum creatinine, hypertension, current smoking, and more invasive surgery (surgery other than carotid endarterectomy). We completed the same analysis including both flow-mediated dilation and reactive hyperemia in the model.
Table 1.
Baseline Characteristics
| Characteristic | No Event (n=217) | Event (n=50) | P |
|---|---|---|---|
| Age, years | 64±11 | 71±9 | <0.001 |
| Gender, % female | 53 (24%) | 17 (34%) | 0.17 |
| Race, % Black | 45 (21%) | 8 (16%) | 0.45 |
| Diabetes mellitus, % | 85 (39%) | 29 (58%) | 0.02 |
| Hypertension, % | 154 (71%) | 42 (84%) | 0.06 |
| Coronary artery disease, % | 78 (36%) | 24 (48%) | 0.11 |
| History of heart failure, % | 16 (7%) | 6 (12%) | 0.28 |
| History of smoking, % | 165 (76%) | 33 (66%) | 0.14 |
| Ex-smoker (%) | 72 (33%) | 20 (40%) | 0.36 |
| Current Smoker (%) | 93 (43%) | 13 (26%) | 0.03 |
| History of hypercholesterolemia, % | 132 (61%) | 30 (63%) | 0.86 |
| Total cholesterol, mg/dL (n=194) | 175±40 | 166±55 | 0.23 |
| LDL cholesterol, mg/dL (n=182) | 100±35 | 84±35 | 0.02 |
| HDL cholesterol, mg/dL (n=191) | 42±12 | 40±13 | 0.30 |
| Triglyceride, mg/dL (n=186) | 172±103 | 200±227 | 0.48 |
| Creatinine, mg/dL (n=267) | 1.2±1.4 | 1.6±1.6 | 0.06 |
| White blood cell count, 1000/μL (n=259) | 8.3±2.8 | 9.0±3.0 | 0.15 |
| Hematocrit, % (n=167) | 38.6±6.5 | 38.5±5.5 | 0.92 |
| Carotid endarterectomy, % | 59 (27%) | 4 (8%) | 0.004 |
| ACE inhibitor or ARB therapy, % | 90 (42%) | 27 (54%) | 0.11 |
| Lipid lowering therapy, % (n=257) | 111 (53%) | 23 (48%) | 0.52 |
| Beta-blocker therapy, % | 117 (54%) | 33 (66%) | 0.12 |
| Calcium channel blocker, % | 40 (18%) | 11 (22%) | 0.56 |
| Nitrate, % | 12 (6%) | 3 (6%) | 0.90 |
| Aspirin and/or clopidogrel, % | 126 (58%) | 31 (62%) | 0.61 |
| Ascorbic acid therapy, % (n=226) | 8 (4%) | 3 (7%) | 0.48 |
Data are mean±SD or No. and percentage as indicated. Sample size is 267 unless otherwise indicated. ACE indicates angiotensin converting enzyme; ARB, angiotensin receptor blocker.
Analysis was completed using SPSS for Windows version 12.0.1 (SPSS Inc). Data were presented as mean±SD, and a probability value <0.05 was considered statistically significant.
Results
Study Subjects
A total of 267 patients enrolled in the study. All underwent a vascular surgical operation after enrollment, including carotid endarterectomy (n=63), peripheral bypasses (n=132), abdominal aortic aneurysm repair (n=46), limb amputation (n=19), or other surgery, including femoral endarterectomy or wound exploration and debridement (n=7). The median follow-up time was 309 days (ranging from 1 to 730 days). An event occurred in 50 patients (19%) during the follow-up period, including cardiovascular death (n=15), myocardial infarction (n=18), unstable angina (n=8), heart failure (n=6), and nonhemorrhagic stroke (n=3).
The clinical characteristics of patients with and without an event are listed in Table 1. As shown, patients with an event were older, and were more likely to have diabetes mellitus. Patients with an event were less likely to have undergone carotid endarterectomy. Unexpectedly, LDL cholesterol was lower in patients with an event, possibly reflecting indication bias.
Brachial Artery Ultrasound Results
For the group as a whole, mean hyperemic flow velocity was 91±48 cm/s (n=267), mean flow-mediated dilation was 6.4±4.5% (n=267), and mean nitroglycerin-mediated dilation was 10.6±6.6% (n=86). The vascular function variables for patients with and without an event are listed in Table 2. As shown, the subjects with an event had lower hyperemic flow velocity and flow-mediated dilation. They also had lower nitroglycerin-mediated dilation and lower hyperemic shear stress. In contrast, there were no group differences in mean baseline brachial diameter, flow volume, flow velocity, or shear stress. There also were no differences in hyperemic flow volume or percent change in flow volume.
Table 2.
Brachial Ultrasound Results
| No Event (n=217) | Event (n=50) | P | |
|---|---|---|---|
| Baseline | |||
| Brachial diameter, mm | 4.06±0.87 | 4.11±0.91 | 0.72 |
| Flow volume, mL/min | 156±114 | 142±108 | 0.45 |
| Flow velocity, cm/s | 20±14 | 17±10 | 0.18 |
| Shear stress, dyne/cm2 | 14±11 | 12±7 | 0.13 |
| Hyperemic | |||
| Flow volume, mL/min | 788±562 | 650±490 | 0.11 |
| Flow velocity, cm/s | 95±50 | 75±39 | 0.004 |
| Shear stress, dyne/cm2 | 68±39 | 53±30 | 0.004 |
| Change from baseline | |||
| Flow-mediated dilation, % | 6.9±4.6 | 4.5±3.0 | <0.001 |
| Flow-mediated dilation, mm | 0.27±0.17 | 0.18±0.11 | <0.001 |
| Nitroglycerin-mediated dilation, %* | 11.5±6.7 | 7.6±5.3 | 0.02 |
| Change in flow volume, % | 472±330 | 438±319 | 0.52 |
n=86 for nitroglycerin-mediated dilation. The remainder of subjects had a contra-indication or declined to take nitroglycerin.
Predictive Value of Hyperemic Flow Velocity and Flow-Mediated Dilation
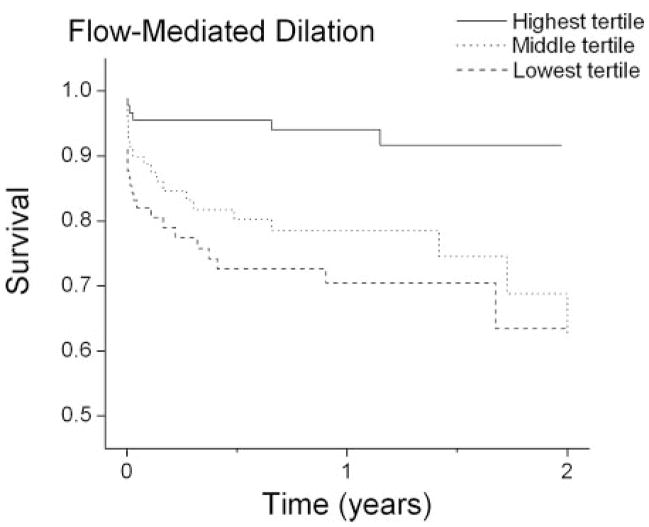
Kaplan–Meier plots according to tertiles of hyperemic flow velocity and flow-mediated dilation are shown in Figure 1 and Figure 2, respectively. As shown, subjects with hyperemic flow velocity in the highest tertile (≥ 105 cm/sec) had better event-free survival compared with subjects in the middle and lower tertiles (P=0.01 for both). Similarly, subjects with the highest flow-mediated dilation (≥7.9%) had better event-free survival compared with subjects in the lower and middle tertiles (P<0.001 and P=0.002, respectively). Because the middle and lower tertiles had comparable event-free survival for both measures of vascular function, these tertiles were grouped together in subsequent analyses.
Figure 1.
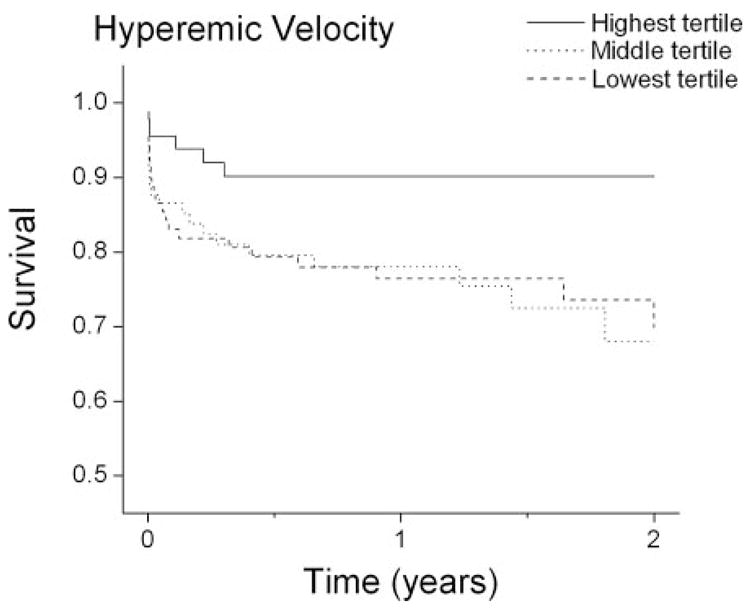
Kaplan–Meier plots showing survival according to tertile of hyperemic velocity. Overall, survival differed according to tertile of hyperemic velocity by log-rank test (P=0.03). By pairwise comparison, the survival curves for the lower (8 to 61 cm/sec, n=89) and middle (63 to 105 cm/sec, n=89) tertiles did not differ (P=0.91), but both differed from the highest tertile (105 to 269 cm/sec, n=89) by log-rank test (P=0.01 for both).
Figure 2.
Kaplan–Meier plots showing survival according to tertile of flow-mediated dilation. Overall, survival differed according to tertile of flow-mediated dilation by log-rank test (P<0.001). By pairwise comparison, the survival curves for the lower (−2.3 to 4.1%, n=89) and middle (4.2 to 7.9%, n=89) tertiles did not differ (P=0.34), but both differed from the highest tertile (8.0% to 25%, n=89) by log-rank test (P<0.001 and P=0.002, respectively).
We further explored the relation between hyperemic flow velocity and events by examining the incidence of specific events according to hyperemic flow velocity. As shown in Table 3, the incidence of death and the combined primary end point of any event were significantly higher in subjects with lower hyperemic flow velocity. There was a trend for a higher incidence of unstable angina in patients with lower hyperemic flow. The incidence of myocardial infarction was numerically higher and the incidence of stroke was numerically lower in patients with lower hyperemic flow, but these differences did not reach statistical significance, possible reflecting type 2 statistical error due to the relatively low number of individual events. We also considered the possibility that the relationship between cardiovascular events and hyperemic flow might be different for events in the immediate post-operative period compared with more chronic events. As shown in Table 3, reactive hyperemia predicted events in both periods.
Table 3.
Cardiovascular Events According to Hyperemic Response
| Hyperemic Velocity
|
|||
|---|---|---|---|
| Lower Two Tertiles <105 cm/sec (n=178) | Upper Tertile ≥105 cm/sec (n=89) | P Value* | |
| Death | 14 (7.9%) | 1 (1.1%) | 0.02 |
| Myocardial infarction | 15 (8.4%) | 3 (3.4%) | 0.12 |
| Unstable angina | 8 (4.5%) | 0 | 0.06 |
| Heart failure | 5 (2.8%) | 1 (1.1%) | 0.67 |
| Ischemic stroke | 1 (0.6%) | 2 (2.2%) | 0.26 |
| Any event | 43 (24%) | 7 (7.9%) | 0.001 |
| Early events (<30 days)† | 25 (14%) | 4 (5.5%) | 0.02 |
| Late events (30 days to 2 years) | 22 (12%) | 3 (3.4%) | 0.02 |
Chi Square test. n=267;
Four subjects had an event in both the early and late periods.
Multivariable Analyses
Table 4 displays the results of multivariable analyses of the relation between vascular function and the primary endpoint of any cardiovascular event. As shown (Model 1), lower hyperemic flow velocity, older age, and more invasive surgical procedure were significant predictors in an analysis that also included gender, diabetes mellitus, hypertension, current smoking, and serum creatinine as candidate variables. As previously reported in a subset of the present cohort,6 flow-mediated dilation was also a significant multivariable predictor of events (Model 2).
Table 4.
Stepwise Models for Predictors of Cardiovascular Events
| Odds Ratio | 95.0% CI | P | |
|---|---|---|---|
| Model 1 | |||
| Low hyperemic flow velocity | 2.6 | 1.2–5.9 | 0.019 |
| Age (per decade) | 1.9 | 1.4–2.5 | <0.001 |
| More invasive surgery | 3.8 | 1.4–11 | 0.01 |
| Model 2 | |||
| Low flow-mediated dilation | 4.1 | 1.8–9.7 | 0.001 |
| Age (per decade) | 1.8 | 1.3–2.3 | <0.001 |
| More invasive surgery | 4.3 | 1.5–12 | 0.005 |
| Model 3 | |||
| Low hyperemic flow velocity | 2.7 | 1.2–5.9 | 0.018 |
| Low flow-mediated dilation | 4.2 | 1.8–9.8 | 0.001 |
| Age (per decade) | 1.8 | 1.3–2.4 | <0.001 |
| More invasive surgery | 3.9 | 1.4–11 | 0.01 |
Candidate variables for all models included age, gender, serum creatinine, more invasive (noncarotid) surgery, diabetes mellitus, hypertension, and current cigarette smoking. Model 1 also included hyperemic flow, Model 2 also included flow-mediated dilation, and Model 3 also included both vascular function variables.
To assess the relative strength of hyperemic flow velocity and flow-mediated dilation as predictors of events, we repeated the Cox regression analysis including both measures of vascular function as candidate variables. As shown in Table 4 (Model 3), hyperemic flow velocity and flow-mediated dilation were both significant predictors of events, suggesting that these measures of vascular function provide incremental information about cardiovascular risk. The concept that hyperemic flow velocity and flow-mediated dilation provide distinct information about risk is further supported by the finding that there was no significant correlation between the 2 variables (r=0.12, P=0.053). There also was no significant a correlation between hyperemic flow volume and flow-mediated dilation (r=0.12, P=0.06). There was, however, a significant correlation between hyperemic shear stress and flow-mediated dilation (r=0.24, P<0.001). The study had 80% power (alpha=0.05) to detect an r value of 0.17.
Discussion
In this prospective study, older age, more invasive (noncarotid) surgery, and lower hyperemic flow velocity in the brachial artery predicted cardiovascular events in a high risk group of patients with peripheral arterial disease referred for surgery. When hyperemic flow velocity, a measure of microvascular function, flow-mediated dilation, a measure of conduit artery function, and other risk factors were included in the same multivariable model, both measures of vascular function were significant predictors, although flow-mediated dilation was the stronger predictor of risk. These findings suggest that microvascular and conduit artery vasodilator function provide incremental information about cardiovascular risk, and that both may relate to the pathogenesis of cardiovascular events.
Reactive hyperemia is a fundamental homeostatic response of the vasculature that serves to accelerate oxygen delivery to tissues following a period of ischemia. Hyperemic blood flow peaks within a few seconds after restoration of flow and flow then declines in an exponential fashion to basal levels over a period of 2 to 3 minutes. Early studies by Rubio and Berne suggested that this response depends on increased tissue level of adenosine, which dilates resistance vessels and increases blood flow.12 Reactive hyperemia has been shown to depend on several other factors, including prostaglandins, potassium, pH,13 and hydrogen peroxide.14 Studies in animal models15 have shown that reactive hyperemia also depends, in part, on endothelium-derived nitric oxide, which may be produced as a secondary response to increased flow and local shear stress.
Reactive hyperemia after 5-minute cuff occlusion has frequently been examined in humans by measuring hyperemic flow velocity or volume flow by ultrasound, as was done in the present study, or by measuring hyperemic volume flow using venous occlusion plethysmography. Using the latter methodology, several groups have shown that reactive hyperemia in healthy volunteers depends, in part, on endothelium-derived nitric oxide.2,3,16 Human studies have also demonstrated that reactive hyperemic is blunted in patients with atherosclerosis17,18 or cardiovascular disease risk factors.3–5 For example, recent studies from the Framingham Heart Study demonstrated inverse correlations between hyperemic flow velocity and traditional coronary risk factors4 and systemic markers of inflammation.5
A number of studies have examined the mechanisms of blunted reactive hyperemia in patients with risk factors. Higashi and colleagues observed that the nitric oxide synthase inhibitor mono-methyl-L-arginine reduces reactive hyperemia in healthy subjects, but not hypertensive subjects, suggesting that blunted reactive hyperemia reflects, in part, a loss of endothelium-derived nitric oxide.3 On the other hand, histological examination of microvessels in skeletal muscle from hypertensive patients reveals increased medial thickness and other structural changes that might impair vasodilator capacity.19 Thus, it appears likely that multiple mechanisms contribute to blunted reactive hyperemia in the setting of hypertension and other forms of cardiovascular disease.
Impairment of reactive hyperemia in the coronary circulation has the potential to worsen myocardial ischemia, and, thus, could contribute to the pathogenesis of cardiovascular events. Our study provides support for this possibility. Two prior studies examined this issue in patients with end-stage renal disease and demonstrated associations between cardiovascular events and postocclusive hyperemia in the forearm20 and in the skin.21 Those studies involved relatively small numbers of patients (n=78 and n=70, respectively), and in the latter study the investigators did not perform a multivariable analysis. The present study had a larger sample size and greater statistical power to adjust for potential confounders, and thus provides additional and stronger support for hypothesis that impaired reactive hyperemia contributes to cardiovascular risk. Our findings with a noninvasive method also fit well with prior studies that used intraarterial infusion of specific endothelium-dependent vasodilators to show that endothelial dysfunction in forearm microvessels predicts cardiovascular events.22,23
It is notable that we observed a relationship between events and hyperemic flow velocity, but the relationship was not statistically significant with hyperemic flow volume. This observation is consistent with our prior study showing no relationship with events when hyperemia was expressed as percent change in flow volume.11 The study by Mitchell and colleagues from the Framingham Heart Study also demonstrated a weaker relationship between percent change in hyperemic flow volume and cardiovascular risk factors, whereas hyperemic flow velocity and hyperemic shear stress both correlated much more strongly with risk factors.4 The explanation for the stronger relationship with hyperemic flow velocity is not entirely clear but may reflect greater variability in the volume results, which is calculated as the product of velocity and the square of the arterial diameter, compounding the measurement variability associated with each variable. Alternatively, brachial diameter is larger whereas velocity is lower in patients with risk factors, and these opposing trends may confound the volume flow analysis. In the present study, we have focused on flow velocity based on our prior studies at the Framingham Heart Study that examined the cross-sectional relation of hyperemic flow velocity with risk factors.4,5 The present prospective study provides new evidence that hyperemic flow velocity provides prognostic information in patients with atherosclerosis.
In addition to presenting new data on hyperemic flow, which reflects microvascular function, we also reexamined the relationship between conduit artery vasodilator function and cardiovascular events in this somewhat larger cohort. As we previously reported in a subset of the patients used in the present study, patients with an event had lower brachial artery flow-mediated dilation.6 In our prior report, we observed no significant relationship between nitroglycerin-mediated dilation and events in the subset of 65 patients that received nitroglycerin. In the present study, 86 patients received nitroglycerin and the vasodilator response was significantly lower in the group of patients with an event. We attribute these apparently discrepant results to the larger sample size of the present study. Although the nitroglycerin findings are limited by the small sample size, they are consistent with prior work by other investigators.22,24
Recently, there has been controversy about the relative clinical utility of reactive hyperemia and brachial artery flow-mediated dilation, which also has been shown to predict cardiovascular events.6,11,25–27 Investigators have suggested that reactive hyperemia might be a better predictor, because Mitchell and colleagues observed that reactive hyperemic velocity and hyperemic shear stress correlated more strongly with risk factors than flow-mediated dilation in the Framingham Heart Study.4,7 Furthermore, adjusting for hyperemic velocity in multivariable models greatly attenuated the inverse correlation between flow-mediated dilation and risk factors.4 Because reactive hyperemia is the stimulus for flow-mediated dilation, investigators interpreted these findings to suggest that the previously reported relationship between flow-mediated dilation and cardiovascular disease might be attributable to reactive hyperemia.7
The present study directly compared the relative predictive values of these 2 measures of vascular function. If diminished reactive hyperemia accounted for the observed relation between impaired flow-mediated dilation and events, we would have expected that inclusion of both variables in the multivariable model would have decreased the odds ratio and lessened the degree of statistical significance. In our study, both variables were retained in the model (Table 4, Model 3) and the odds ratios were actually increased, suggesting that both measures of vascular function provide distinct and incremental information about cardiovascular risk.
Our study has several limitations. First, we examined a relatively select population of patients with advanced atherosclerosis referred for surgery and the findings may not be more generally applicable. Second, we did not control medications or time of vascular study. We previously demonstrated, however, that withholding medications does not alter the results of our studies of vascular function,28 and such factors would be expected to bias the study toward a null result. Third, it is likely that a larger study would have allowed us to identify other predictors of cardiovascular risk that approached significance in our study such as prevalent coronary artery disease, hypertension, white blood cell count, and hyperemic volume flow.29–31 Finally, we were only able to administer nitroglycerin to a minority of patients and could not administer an inhibitor of nitric oxide synthase, so we cannot categorically conclude that the relation between flow-mediated dilation and events reflects endothelial function. Balancing these limitations are the prospective study design and simultaneous comparison of hyperemic flow velocity and flow-mediated dilation in the same patients.
In conclusion, our study demonstrated for the first time that both hyperemic flow velocity and conduit artery flow-mediated dilation predicted long-term cardiovascular events in patients with peripheral artery disease referred for vascular surgery. These findings support the relevance of conduit artery dysfunction and microvascular dysfunction in the pathogenesis of cardiovascular events and support the possibility that such testing might have clinical utility for patient management.
Acknowledgments
Sources of Funding
This study was supported by NIH grants HL75795, HL60886, HL55993, HL 083269, and HL083781. Drs Huang and Silver received support from the Boston University School of Medicine Basic Science Cardiovascular Training Program (T32 HL 07224).
Footnotes
Disclosures
None.
References
- 1.Loscalzo J, Vita JA. Ischemia, hyperemia, exercise, and nitric oxide: Complex physiology and complex molecular adaptations. Circulation. 1994;90:2556–2559. doi: 10.1161/01.cir.90.5.2556. [DOI] [PubMed] [Google Scholar]
- 2.Meredith IT, Currie KE, Anderson TJ, Roddy MA, Ganz P, Creager MA. Postischemic vasodilation in human forearm is dependent on endothelium-derived nitric oxide. Am J Physiol. 1996;270:H1435–H1440. doi: 10.1152/ajpheart.1996.270.4.H1435. [DOI] [PubMed] [Google Scholar]
- 3.Higashi Y, Sasaki S, Nakagawa K, Matsuura H, Kajiyama G, Oshima T. A noninvasive measurement of reactive hyperemia that can be used to assess resistance artery endothelial function in humans. Am J Cardiol. 2001;87:121–125. doi: 10.1016/s0002-9149(00)01288-1. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell GF, Parise H, Vita JA, Larson MG, Warner E, Keaney JF, Jr, Keyes MJ, Levy D, Vasan RS, Benjamin EJ. Local shear stress and brachial artery flow-mediated dilation: The Framingham Heart Study. Hypertension. 2004;44:134–139. doi: 10.1161/01.HYP.0000137305.77635.68. [DOI] [PubMed] [Google Scholar]
- 5.Vita JA, Keaney JF, Jr, Larson MG, Keyes MJ, Massaro JM, Lipinska I, Lehman B, Fan S, Osypiuk E, Wilson PWF, Vasan RS, Mitchell GF, Benjamin EJ. Brachial artery vasodilator function and systemic inflammation in the Framingham Offspring Study. Circulation. 2004;110:3604–3609. doi: 10.1161/01.CIR.0000148821.97162.5E. [DOI] [PubMed] [Google Scholar]
- 6.Gokce N, Keaney JF, Jr, Hunter LM, Watkins MT, Nedeljkovic ZS, Menzoian JO, Vita JA. Predictive value of non-invasively-determined endothelial dysfunction for long-term cardiovascular events in patients with peripheral vascular disease. J Am Coll Cardiol. 2003:1769–1775. doi: 10.1016/s0735-1097(03)00333-4. [DOI] [PubMed] [Google Scholar]
- 7.O’Rourke MF, Nichols WW. Shear stress and flow-mediated dilation. Hypertension. 2004;44:119–120. doi: 10.1161/01.HYP.0000137301.99716.e8. [DOI] [PubMed] [Google Scholar]
- 8.Vita JA. Nitric oxide-dependent vasodilation in human subjects. Methods Enzymol. 2002;359:186–200. doi: 10.1016/s0076-6879(02)59183-7. [DOI] [PubMed] [Google Scholar]
- 9.McMackin CJ, Vita JA. Update on nitric oxide-dependent vasodilation in human subjects. Methods Enzymol. 2005;396:541–553. doi: 10.1016/S0076-6879(05)960-16-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duffy SJ, Keaney JF, Jr, Holbrook M, Gokce N, Swerdloff PL, Frei B, Vita JA. Short- and long-term black tea consumption reverses endothelial dysfunction in patients with coronary artery disease. Circulation. 2001;104:151–156. doi: 10.1161/01.cir.104.2.151. [DOI] [PubMed] [Google Scholar]
- 11.Gokce N, Keaney JF, Jr, Menzoian JO, Watkins M, Hunter L, Duffy SJ, Vita JA. Risk stratification for postoperative cardiovascular events via noninvasive assessment of endothelial function. Circulation. 2002;105:1567–1572. doi: 10.1161/01.cir.0000012543.55874.47. [DOI] [PubMed] [Google Scholar]
- 12.Rubio R, Berne RM. Release of adenosine by the normal myocardium in dogs and its relationship to the regulation of coronary resistance. Circ Res. 1969;25:407–415. doi: 10.1161/01.res.25.4.407. [DOI] [PubMed] [Google Scholar]
- 13.Sparks HV, Jr, Belloni FL. The peripheral circulation: local regulation. Annu Rev Physiol. 1978;40:67–92. doi: 10.1146/annurev.ph.40.030178.000435. [DOI] [PubMed] [Google Scholar]
- 14.Wolin MS, Rodenburg JM, Messina EJ, Kaley G. Similarities in the pharmacological modulation of reactive hyperemia and vasodilation to hydrogen peroxide in rat skeletal muscle arterioles: effects of probes for endothelium-derived mediators. J Pharmacol Exp Ther. 1990;253:508–512. [PubMed] [Google Scholar]
- 15.Kostic MM, Schrader J. Role of nitric oxide in reactive hyperemia of the guinea pig heart. Circ Res. 1992;70:208–212. doi: 10.1161/01.res.70.1.208. [DOI] [PubMed] [Google Scholar]
- 16.Tagawa T, Imaizumi T, Endo T, Shiramoto M, Harasawa Y, Takeshita A. Role of nitric oxide in reactive hyperemia in human forearm vessels. Circulation. 1994;90:2285–2290. doi: 10.1161/01.cir.90.5.2285. [DOI] [PubMed] [Google Scholar]
- 17.Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, Lloyd JK, Deanfield JE. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–1115. doi: 10.1016/0140-6736(92)93147-f. [DOI] [PubMed] [Google Scholar]
- 18.Lieberman EH, Gerhard MD, Uehata A, Selwyn AP, Ganz P, Yeung AC, Creager MA. Flow-induced vasodilation of the human brachial artery is impaired in patients <40 years of age with coronary artery disease. Am J Cardiol. 1996;78:1210–1214. doi: 10.1016/s0002-9149(96)00597-8. [DOI] [PubMed] [Google Scholar]
- 19.James MA, Watt PA, Potter JF, Thurston H, Swales JD. Pulse pressure and resistance artery structure in the elderly. Hypertension. 1995;26:301–306. doi: 10.1161/01.hyp.26.2.301. [DOI] [PubMed] [Google Scholar]
- 20.London GM, Pannier B, Agharazii M, Guerin AP, Verbeke FH, Marchais SJ. Forearm reactive hyperemia and mortality in end-stage renal disease. Kidney Int. 2004;65:700–704. doi: 10.1111/j.1523-1755.2004.00434.x. [DOI] [PubMed] [Google Scholar]
- 21.Kruger A, Stewart J, Sahityani R, O’Riordan E, Thompson C, Adler S, Garrick R, Vallance P, Goligorsky MS. Laser Doppler flowmetry detection of endothelial dysfunction in end-stage renal disease patients: correlation with cardiovascular risk. Kidney Int. 2006;70:157–164. doi: 10.1038/sj.ki.5001511. [DOI] [PubMed] [Google Scholar]
- 22.Heitzer T, Schlinzig T, Krohn K, Meinertz T, Munzel T. Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation. 2001;104:2673–2678. doi: 10.1161/hc4601.099485. [DOI] [PubMed] [Google Scholar]
- 23.Perticone F, Ceravolo R, Pujia A, Ventura G, Iacopino S, Scozzafava A, Ferraro A, Chello M, Mastroroberto P, Verdecchia P, Schillaci G. Prognostic significance of endothelial dysfunction in hypertensive patients. Circulation. 2001;104:191–196. doi: 10.1161/01.cir.104.2.191. [DOI] [PubMed] [Google Scholar]
- 24.Schachinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long- term outcome of coronary heart disease. Circulation. 2000;101:1899–1906. doi: 10.1161/01.cir.101.16.1899. [DOI] [PubMed] [Google Scholar]
- 25.Modena MG, Bonetti L, Coppi F, Bursi F, Rossi R. Prognostic role of reversible endothelial dysfunction in hypertensive postmenopausal women. J Am Coll Cardiol. 2002;40:505–510. doi: 10.1016/s0735-1097(02)01976-9. [DOI] [PubMed] [Google Scholar]
- 26.Brevetti G, Silvestro A, Schiano V, Chiariello M. Endothelial dysfunction and cardiovascular risk prediction in peripheral arterial disease: Additive value of flow-mediated dilation to ankle-brachial pressure index. Circulation. 2003;108:2093–2098. doi: 10.1161/01.CIR.0000095273.92468.D9. [DOI] [PubMed] [Google Scholar]
- 27.Chan SY, Mancini GB, Kuramoto L, Schulzer M, Frohlich J, Ignaszewski A. The prognostic importance of endothelial dysfunction and carotid atheroma burden in patients with coronary artery disease. J Am Coll Cardiol. 2003;42:1037–1043. doi: 10.1016/s0735-1097(03)00927-6. [DOI] [PubMed] [Google Scholar]
- 28.Gokce N, Holbrook M, Hunter LM, Palmisano J, Vigalok E, Keaney JF, Jr, Vita JA. Acute effects of vasoactive drug treatment on brachial artery reactivity. J Am Coll Cardiol. 2002;40:761–765. doi: 10.1016/s0735-1097(02)02034-x. [DOI] [PubMed] [Google Scholar]
- 29.Gillespie DL, LaMorte WW, Josephs LG, Schneider T, Floch NR, Menzoian JO. Characteristics of patients at risk for perioperative myocardial infarction after infrainguinal bypass surgery: an exploratory study. Ann Vasc Surg. 1995;9:155–162. doi: 10.1007/BF02139658. [DOI] [PubMed] [Google Scholar]
- 30.Hiatt WR. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001;344:1608–1621. doi: 10.1056/NEJM200105243442108. [DOI] [PubMed] [Google Scholar]
- 31.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM, Jr, White CJ, White J, White RA, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic) Circulation. 2006;113:e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]